Fig. 12.1
Types of anastomoses seen in Brescia–Cimino fistulae. (a) Normal anatomy. (b) End-to-end anastomosis. (c) End-to-side anastomosis
AVGs are synthetic grafts made of Dacron or polytetrafluoroethylene (PTFE) usually 6–8 mm in diameter. Nonsynthetic grafts include bovine carotid artery or venous grafts (cadaveric or noncadaveric). Loop grafts are usually placed within the forearm and anastomosed to the brachial artery and to the basilic or brachial vein (Fig. 12.2). Grafts in the upper arm are usually straight connecting the brachial artery to either the antecubital, cephalic, basilic, or axillary vein. Generally, the venous limb of a forearm loop graft is placed within the medial aspect of the forearm with the exception of reversed grafts where the arterial limb is located medially. AVGs can be placed within the groin to anastomose the femoral artery to the femoral vein or to the greater saphenous vein. AVGs are easier to cannulate and mature quicker but are less durable than AVFs [3]. It is generally recommended that AVGs be placed only if AVFs cannot be created.
Fig. 12.2
Typical types of upper extremity grafts. (a) Loop graft. (b) Straight graft
Indications/Contraindications
A hemodialysis access is deemed dysfunctional if there is a hemodynamically significant stenosis, if the access (AVF) has failed to mature, if the access cannot be cannulated for hemodialysis, or if the access has thrombosed. A hemodynamically significant stenosis occurs when there is a greater than 50 % reduction in normal vessel diameter [2]. The most common cause of hemodialysis access dysfunction is venous outflow stenosis in greater than 80 % of cases. In AVGs, venous stenoses typically occur at the venous anastomosis but can also occur in a more central location. Subclavian and brachiocephalic vein stenoses are typically result from prior placement of central venous catheters. In AVFs, the area of stenosis is typically within 3 cm of the anastomosis [3]. Arterial stenosis occurs in less than 5 % of cases (Table 12.1).
Table 12.1
Causes of hemodialysis access failure
1. Thrombosis |
2. Stenosis |
(a) Venous (80 % in AVGs, 25 % in AVFs) |
(b) Arterial anastomotic (10 % in AVGs, 52 % in AVFs) |
(c) Central (27 %) |
3. Pseudoaneurysm formation (5 % in AVGs and 15 % in AVFs) |
4. Arterial steal |
Hemodialysis access dysfunction requiring fistulography can be detected with various surveillance modalities (Table 12.2). Physical examination is an important monitoring tool [4, 5]. The loss of a continuous thrill indicates flow rates <450 mL/min and that an intervention is necessary. Other clinical indicators include prolonged bleeding after decannulation; extremity swelling; a rigid, enlarging, or abnormally flat pseudoaneurysm; a loss of a continuous bruit on auscultation; palpable outflow stenosis (AVFs); the presence of prominent skin veins; or a decompressed outflow vein (AVFs). Evaluation of central venous stenosis after surgical thrombectomy and evaluation of vascular steal are additional indicators for fistulography. The main indication for thrombectomy is to restore patency of a thrombosed graft.
Table 12.2
Measured flow rate parameters indicating access dysfunction (DOQI)
1. Direct intra-access flow measurement (Transonics) of less than 600 mL/min (AVGs) or less than 1000 mL/min (AVFs) or a decrease by more than 25 % over 4 months |
2. Elevated static (venous limb pressure > 40 % systemic pressure) or dynamic venous pressure (>150 mmHg at 200–250 mL/min) |
3. Non-urea recirculation of >5 % indicating retrograde flow. Urea-based (two-needle method) recirculation of >10–20 % (AVFs) |
4. Unexplained decreases in the amount of hemodialysis delivered (decreased Kt/V) |
5. Elevated negative arterial pressure resulting in decreased blood flow |
The only absolute contraindication to intervention is infection within a thrombosed access. Relative contraindications include significant metabolic disturbance, right to left shunts, severe pulmonary compromise, significant contrast allergy, and severe right heart failure.
Central venous angioplasty is not advised in patients who are coagulopathic since venous rupture would be life threatening. In the treatment of thrombosed grafts, the use of tissue plasminogen activator is contraindicated in patients with recent cerebrovascular accident, active internal bleeding, recent surgical procedures, and the presence of an intracranial aneurysm. In those cases, mechanical thrombectomy rather than thrombolysis would be performed. Severe contrast allergy can be pretreated prior to the procedure.
Preprocedure Workup
A clinical examination of the AVF or AVG is important to confirm a thrombosed graft, absence of a thrill, to evaluate pseudoaneurysms, to evaluate for superficial collateral veins, and to evaluate location of the arterial and venous limb of the AVG. Ultrasound is a great tool for use in AVFs to evaluate patency of the anastomosis as well as location of thrombus and/or stenoses which will aid in determining the point of access prior to intervention. Cardiorespiratory examination is important to evaluate for fluid overload. If the patient has missed more than two dialysis sessions, it is important to rule out hyperkalemia. An ill patient with an elevated serum concentration of potassium greater than 5 mEq/L who has not been dialyzed may be better served with a temporary dialysis catheter. Emergent therapy of hyperkalemia is indicated especially with the presence of ECG changes if the serum concentration of potassium is greater than 6.5 mEq/L [6]. Obtaining coagulation values is recommended prior to central venous intervention.
Sedation
All children will require some degree of sedation during fistulography. Younger children under the age of 12 will likely require general anesthesia. Older children greater than 12 years of age may respond well to moderate sedation. The majority will require general anesthesia for percutaneous thrombectomy.
Fistulography
The goal of fistulography is to image the arterial inflow, the entire fistula or graft, and the entire venous outflow including the central veins.
Fistulography: Arteriovenous Grafts
If the interventionalist is unsure which limb of the graft is venous or arterial, manually compressing the apex of the graft will result in absence of pulsatility within the venous limb with continued pulsatility of the arterial limb. The venous limb is typically punctured in an antegrade fashion pointing toward the venous outflow with subsequent contrast injection since venous outflow stenosis is the main cause of hemodialysis access dysfunction (Fig. 12.3). A second retrograde puncture of the venous limb may be required if the arterial inflow or intragraft stenosis of the arterial limb needs to be treated (Fig. 12.4). Alternatively, the apex of the graft can be punctured to allow access to both the venous and arterial limb. Once the venous outflow has been treated, the access can be reversed to allow intervention on the arterial limb [7]. A 6 Fr high-flow sheath is typically sufficient to allow placement of up to a 10 Fr balloon. Upsizing to a larger sheath will be needed for placement of a covered stent. In order to visualize the arterial anastomosis and the arterial limb, reflux fistulography is performed. This can be accomplished during balloon inflation when treating the venous outflow, by manual compression of the venous limb or by venous outflow compression using a blood pressure cuff with simultaneous injection of contrast. Alternatively, direct fistulography can be performed by catheterization of the arterial inflow through the retrograde venous limb access in order to visualize the entire AVG and arterial anastomosis.
Get Clinical Tree app for offline access
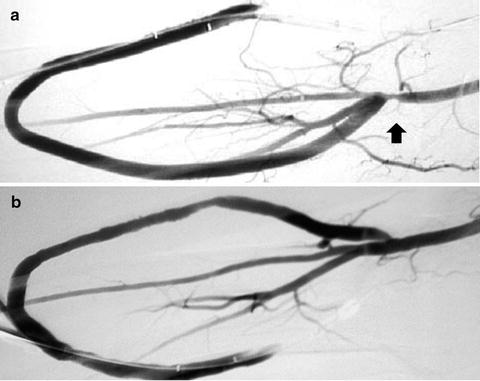
Fig. 12.3
Forearm loop fistulography post declotting procedure demonstrating a significant venous anastomotic stenosis