Hepatobiliary
QUESTIONS
1 A previously healthy 27-year-old male presents with right upper quadrant pain and jaundice. Which of the following is the most likely diagnosis?
|
A. Hepatitis
B. Cirrhosis
C. Acute cholecystitis
D. Acalculous cholecystitis
View Answer
1 Answer A. The first image shows a markedly thickened and striated gallbladder wall. The second image shows a part of the liver parenchyma that appears normal. The gallbladder wall is considered thickened when it is over 3 mm. Diffuse gallbladder wall thickening occurs in the setting of both biliary and nonbiliary processes. Biliary etiologies include cholecystitis, gallbladder cancer, adenomyomatosis, primary sclerosing cholangitis, and AIDS cholangitis. Nonbiliary causes due to edema include hepatitis, ascites, cirrhosis, portal hypertension, hypoproteinemia, and lymphatic obstruction. The initial evaluation of gallbladder wall thickening should include a careful assessment for gallstones and a sonographic Murphy sign to exclude acute cholecystitis.
This patient overdosed on Tylenol. Gallbladder wall thickening can be the only sonographic sign of acute hepatitis. Gallbladder wall thickening is hypothesized to be due to an inflammatory reaction, such as hyperemia, in the serosal and muscular layers adjacent to the liver in response to necrosis and inflammation of the liver tissues. Hepatomegaly and periportal edema (with relative echogenicity of the biliary triads—“starry sky” appearance) can also be seen, especially in viral hepatitis.
The hepatic echotexture would be expected to be coarsened in a patient with cirrhosis (answer choice B), and it is normal in this case. No gallbladder distension or gallstones are shown to support the diagnosis of acute cholecystitis (answer choice C). Acalculous cholecystitis (answer choice D) usually occurs in critically ill ICU patients, and the gallbladder would be expected to be distended in that case as well.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:46-48.
Smith EA, Dillman JR, Elsayes KM, et al. Cross-sectional imaging of acute and chronic gallbladder inflammatory disease. AJR Am J Roentgenol 2009;192(1):188-196.
2a This 60-year-old female was found to have gallbladder wall thickening on CT. What is the next best step for management of this finding?
|
A. No need for follow-up
B. Cholecystectomy
C. MRCP
D. Contrast-enhanced CT
View Answer
2a Answer A. Focal thickening of the wall of the gallbladder fundus is noted to contain both a rounded cystic focus and an echogenic reflector with comet-tail artifact. The presence of an echogenic focus with comet-tail artifact is highly specific for adenomyomatosis and is the result of cholesterol crystals within Rokitansky-Aschoff sinuses. Adenomyomatosis is relatively common and is a hyperplastic cholesterolosis of the gallbladder wall, a benign condition. Therefore, no further work-up is needed.
2b Adenomyomatosis is most commonly associated with:
A. Gallbladder carcinoma
B. Cholelithiasis
C. Pancreatitis
D. Cirrhosis
View Answer
2b Answer B. Although some data suggest a possible association of adenomyomatosis and gallbladder carcinoma, there is no conclusive evidence yet for the increased risk for gallbladder carcinoma. There is a clear association of adenomyomatosis (especially segmental type) with gallstones, possibly related to fundal stasis.
References: Boscak AR, Al-Hawary M, Ramsburgh SR. Best cases from the AFIP: adenomyomatosis of the gallbladder. RadioGraphics 2006;26:941-946.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:45-46.
3a This 50-year-old female presented with right upper quadrant pain, and images of the common duct are shown. What is the most appropriate management?
|
A. Sphincterotomy
B. Cholecystectomy
C. ERCP
D. HIDA scan
View Answer
3a Answer C. The differential diagnosis for cystic lesions within the porta hepatis includes hepatic cyst, enteric duplication cysts, pancreatic pseudocyst, biliary cysts, and hepatic artery aneurysm. The images show a fusiform cystic structure containing echogenic nonmobile tissue with papillary projections. The structure communicates directly with the hepatic ducts (left side of image 1), indicating a choledochocele. Type I choledochal cyst is the most common type of choledochal cyst, accounting for 80% to 90%, and is confined to the extrahepatic bile duct. Type I choledochoceles are associated with an increased risk of both cholangiocarcinoma and gallbladder cancer. The papillary configuration and static nature of the intraluminal lesion are particularly concerning for a cholangiocarcinoma. ERCP would be appropriate for further evaluation and would permit tissue sampling for diagnosis.
3b What is the most common complication associated with choledochoceles?
A. Malignancy
B. Liver abscess
C. Pancreatitis
D. Biliary and pancreatic calculi
View Answer
3b Answer D. Although cholangiocarcinoma is the most ominous complication, it is the second most common complication behind calculus formation within the biliary tree, choledochocele, gallbladder, or pancreatic duct. Other potential complications include pancreatitis, rupture in infants and neonates, and, rarely, cholangitis, liver abscesses, portal hypertension, and ascites.
3c Which type(s) of biliary cyst is (are) commonly treated with a Roux-en-Y hepaticojejunostomy?
A. Types II and III
B. Types I and III
C. Types I and IV
D. Type V
View Answer
3c Answer C. A large majority (˜90%) of carcinomas related to choledochal cysts occur within types I (fusiform extrahepatic) and IV (multiple intra- and extrahepatic). Hence, the general recommendation is for those cysts to be completely removed. Patients with type II cysts can often be treated with cyst excision, and those with type III cysts can be treated with sphincterotomy or endoscopic resection. Choledochal cysts are a premalignant state, with cancer occurring more frequently and earlier than in the general population. The risk increases with age. Observed cancer types in these patients include adenocarcinoma (73% to 84%), anaplastic carcinoma (10%), undifferentiated cancer (5% to 7%), squamous cell carcinoma (5%), and other carcinoma (1.5%). The sites of malignancy are the extrahepatic bile duct (50% to 62%), usually within the choledochal cyst; gallbladder (38% to 46%); intrahepatic bile ducts (2.5%); and liver and pancreas (0.7% each). Most of the cancers are associated with type I choledochal cysts (68%) followed by type IV choledochal cysts (21%) and <10% for other types.
References: Kim OH, Chung HJ, Choi BG. Imaging of the choledochal cyst. RadioGraphics 1995;15:69-88.
Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol 2014;12(2):196.
Singham J, Yoshida EM, Scudamore CH. Choledochal cysts part 1 of 3: classification and pathogenesis. Can J Surg 2009;52(5):434-440.
4a Shown here are transverse and sagittal images of the gallbladder. What is the most concerning sonographic finding?
|
A. Presence of color Doppler flow
B. Wall discontinuity
C. Intraluminal mass
D. Absence of ring-down artifact
View Answer
4a Answer B. The echogenic mass within the gallbladder fundus with power Doppler flow indicates a solid mass. The echogenic wall is interrupted anteriorly at the site of the mass. Although the differential diagnosis for a polypoid lesion containing Doppler flow includes both gallbladder carcinoma and benign polyp, the large size and replacement of the gallbladder lumen are features concerning for malignancy. Wall discontinuity is an especially ominous sign of transmural tumor spread, indicating at least an AJCC stage III tumor (not a candidate for curative resection) with a poor prognosis. Although ring-down artifact is a feature of adenomyomatosis, the absence of ring-down artifact alone does not exclude adenomyomatosis.
4b Patients with gallbladder carcinoma are most likely to also have:
A. Porcelain gallbladder
B. Sludge
C. Gallbladder polyps
D. Gallstones
View Answer
4b Answer D. Gallstones are present in 70% to 90% of patients with gallbladder cancer. The risk for malignancy is higher in patients with larger gallstones and longer duration of cholelithiasis.
4c The most common appearance of gallbladder carcinoma is:
A. Mass replacing gallbladder lumen
B. Intraluminal polypoid lesion
C. Gallbladder wall thickening
D. Cystic mass within the gallbladder
View Answer
4c Answer A. 40% to 65% of patients with gallbladder carcinoma at initial detection are found to have a mass nearly filling or replacing the gallbladder lumen. Gallbladder carcinoma presents as focal or diffuse wall thickening in 20% to 30% of cases. In 15% to 25% of cases, gallbladder carcinoma is initially detected as a polypoid lesion.
References: Franquet T, Montes M, Ruiz de Azua Y, et al. Primary gallbladder carcinoma: imaging findings in 50 patients with pathologic correlation. Gastrointest Radiol 1991;16:143-148.
Hsing AW, Gao YT, Han TQ, et al. Gallstones and the risk of biliary tract cancer: a population-based study in China. Br J Cancer 2007;97(11):1577-1582.
Levy AD, Murakata LA, Rohrmann CA. Gallbladder carcinoma: radiologic-pathologic correlation. RadioGraphics 2001;21:295-314.
5 This patient received a liver transplant 10 years ago and presents with liver dysfunction. What is the most likely diagnosis?
|
A. Biliary anastomotic stricture
B. Recurrent primary sclerosing cholangitis
C. Hepatic arterial anastomotic stenosis
D. Portal vein anastomotic stenosis
View Answer
5 Answer C. Image A: irregular intrahepatic biliary ductal dilatation is shown with intraluminal echogenic tissue along with a complex cystic intrahepatic collection. Images B and C: spectral hepatic arterial waveforms show a parvus tardus waveform indicating an upstream stenosis. The constellation of findings is compatible with hepatic arterial anastomotic stenosis resulting in biliary injury, known as ischemic type biliary lesion (ITBL). Biliary complications occurring after liver transplantation include bile leaks, anastomotic strictures, nonanastomotic strictures, and ampullary dysfunction. The biliary epithelium is particularly vulnerable to ischemic injury because of its reliance on hepatic arterial perfusion, whereas the hepatic parenchyma receives dual blood supply from the portal venous and hepatic arterial system. Ischemic injury can result in biliary necrosis, cast formation, scarring, and multifocal stenosis.
Reference: Seehofer D, Eurich D, Veltzke-Schlieker W, et al. Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant 2013;13:253-265.
6 A right upper quadrant ultrasound is performed. On review of the study, the radiologist notices that the gallbladder was not shown and requests that the technologist obtain additional images to show the gallbladder. This is an example of which quality process?
A. Quality improvement
B. Quality assurance
C. Quality control
View Answer
6 Answer C. Quality control (QC) is the process by which a desired level of quality is verified and maintained in a product or service. QC requires planning, use of proper equipment, continued inspection, and corrective action as necessary. A range of acceptable quality is determined to guide QC measures.
Quality assurance (QA) is an older, less often used term, referring to a reactive, generally retrospective process of determining who was at fault after a medical error is committed and sometimes involving punitive measures.
Quality improvement (QI) is a continuous process of improving quality, often focusing on finding weaknesses in the system in order to prevent errors from occurring rather than attributing blame to individuals. QI activities involve measuring quality and determining how to make things better in an ongoing fashion.
Reference: Quality and safety domain specification and resource guide, core exam study guide. Tucson, AZ: American Board of Radiology, 2016:5.
7a An image from a right upper quadrant ultrasound in a 42-year-old female with abdominal pain is shown. What is the next best step in management of this patient?
|
A. Further characterization by MRI
B. Follow-up imaging
C. Cholecystectomy
D. Hepatobiliary cholescintigraphy
View Answer
7a Answer C. Cholecystectomy is recommended for gallbladder polyps that measure >1 cm because of risk of malignancy. Follow-up imaging can be performed for gallbladder polyps that measure >6 mm but <10 mm. There is no role for MRI or hepatobiliary cholescintigraphy in further characterization of these lesions.
7b When evaluating patients with gallbladder polyps on ultrasound, which imaging feature is most predictive of malignancy?
A. Adjacent gallbladder wall thickening
B. Internal vascular flow on Doppler imaging
C. Size >10 mm
D. Sessile shape
View Answer
7b Answer C. Size >10 mm is most predictive of malignancy.
Reference: Corwin MT, Siewert B, Sheiman RG, et al. Incidentally detected gallbladder polyps: is follow-up necessary?—Long-term clinical and US analysis of 346 patients. Radiology 2011;258(1):277-282.
8 An echogenic focus is identified within the gallbladder lumen. Which of the following maneuvers could help distinguish a true lesion from an artifact?
|
A. Turn off harmonics.
B. Reposition the probe.
C. Increase transducer power.
D. Increase the depth.
View Answer
8 Answer B. The image shows an example of side lobe artifact from echogenic bowel being located adjacent to the anechoic gallbladder lumen. In addition to the main ultrasound beam, an ultrasound probe emits off-center ultrasound pulses. When a strong reflector is encountered by one of these off-center pulses, it can be reflected back to the ultrasound probe and interpreted as being located in the path of the main ultrasound beam. This artifact is generally only a problem when imaging anechoic, fluid-filled structures like the bladder or gallbladder, as the artifact from the side lobe is generally only detectable when imaging an anechoic structure. However, it still occurs when imaging solid organs, but the artifact is usually imperceptible.
The image (on the following page) shows the gallbladder from a slightly different angle than from the image in the question. This image more convincingly shows the echogenic structure “within” the gallbladder lumen to be artifactual. An additional clue that the echogenic structure in the gallbladder is not a gallstone but rather artifactual is the lack of clean shadowing posterior to the echogenic focus that would be expected from a stone. In this case, there is dirty shadowing posterior to the gallbladder, suggestive of bowel gas. The use of harmonic imaging can effectively minimize side lobe artifacts, so turning off harmonics would accentuate this artifact. Increasing transducer power will increase the amplitudes of both the primary beam and side lobes, so the artifact will increase. Increasing the depth of imaging will not decrease this artifact.
|
Reference: Feldman MK, Katyal S, Blackwood MS. US artifacts. RadioGraphics 2009;29(4):1179-1189.
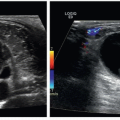
9 A 34-year-old man has a history of acute myeloid leukemia (AML), status post chemotherapy, and stem cell transplant. He is presenting now with acute right upper quadrant pain, weight gain, and elevated liver function tests (LFTs). What is the most likely diagnosis?
|
A. Chemotherapy-induced steatosis
B. Acute cholecystitis
C. Sinusoidal obstruction syndrome
D. Cirrhosis
View Answer
9 Answer C. Image A shows a small amount of perihepatic ascites. Image B shows marked gallbladder wall thickening, and Image C shows reversal of flow in the main portal vein. Based on the clinical history and the provided images, the best answer is C, sinusoidal obstruction syndrome (SOS), also known as venoocclusive disease (VOD).
SOS/VOD is thought to result directly from chemotherapy or radiation-induced destruction of hepatic microvasculature during cytoreductive HSCT (hematopoietic stem cell transplant) conditioning and represents the most common cause of liver disease during the first 20 days after stem cell transplant, affecting 10% to 60% of patients. Clinically, the patient presents with weight gain, painful hepatomegaly, jaundice, and ascites, usually within 3 weeks following hematopoietic stem cell transplantation. It may also happen following some forms of chemotherapy and liver transplantation. Imaging findings mimic those of graft versus host disease (GVHD). Ultrasound findings include hepatosplenomegaly, ascites, gallbladder/periportal edema, hepatofugal flow in the portal vein on Doppler, and elevated RI (>0.75).
Chemotherapy-induced steatosis is not the best choice because the liver is not more echogenic than the adjacent kidney, as one would expect with steatosis. Also, the portal triads and diaphragm are visible indicating normal acoustic penetration. Additionally, this does not explain the findings of gallbladder wall thickening and ascites. Acute cholecystitis is not the best choice because the gallbladder is not distended. It also does not explain the findings of ascites and hepatofugal flow in the portal vein. Cirrhosis is not the best choice because it does not explain the marked gallbladder wall thickening, nor is it the best fit for the clinical scenario.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:68-69.
Mahgerefteh SY, Sosna J, Bogot N, et al. Radiologic imaging and intervention for gastrointestinal and hepatic complications of hematopoietic stem cell transplantation. Radiology 2011;258(3):660-671.
View Answer
10 Answer key:
A. Caudate lobe
B. Left lateral segment
C. Fissure for ligamentum venosum
D. Umbilical portion of left portal vein
E. Main portal vein
F. Common bile duct
G. Right hepatic artery
11 A 38-year-old man with abdominal pain has the following finding on his ultrasound. He is otherwise in good health. What is the most appropriate management for this process?
|
A. Consult surgery for cholecystectomy. There is a 20% increased risk for development of gallbladder carcinoma.
B. Draw blood and test for triglycerides. This finding is associated with hypertriglyceridemia.
C. No further workup is necessary. This finding is almost certainly benign.
D. Perform an MRCP for a search for gallstones. This finding frequently coexists with gallstones.
View Answer
11 Answer C. The three images show the gallbladder with multiple small polyps, the so-called “balls on the wall” sign seen in cholesterolosis. Cholesterolosis is a benign condition in which cholesterol esters are deposited within the lamina propria of the gallbladder. Cholesterol polyps are by far the most common type of gallbladder polyp. They are enlarged papillary fronds filled with lipid-laden macrophages and are not true neoplasms. They are adherent to the wall by a slender stalk, which is rarely seen. They are usually 5 mm or less in size and rarely grow larger than 10 mm. They are distinguished from stones by their lack of shadowing and nonmobility. Their nonmobility distinguishes them from sludge balls. If there are multiple small polyps, they are almost certainly cholesterol polyps and can be ignored. Therefore, answer choice C is the correct answer.
There is no association of cholesterol polyps with gallbladder cancer; therefore answer choice A is not correct. The cause is unknown, but there is no association with serum lipid levels; therefore, answer choice B is incorrect. Cholesterolosis has the same risk factors as cholelithiasis, but the two conditions rarely coexist. Therefore, answer choice D is an incorrect statement.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:44-45.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:209-210.
12 Increasing the depth or width of the field of view will:
A. Decrease the frame rate
B. Increase the frame rate
C. Increase acoustic impedance
D. Decrease acoustic impedance
View Answer
12 Answer A. Increasing the depth or width of the field of view will increase the image size and reduce the frame rate. It has no effect on acoustic impedance.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:11.
13 The speed of sound in soft tissues is:
A. 1,440 m/s
B. 1,540 m/s
C. 1,640 m/s
D. 1,740 m/s
View Answer
13 Answer B.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:4.
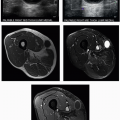
14 This patient is being evaluated for abnormal liver enzymes in the setting of a previous liver transplant. What is the most likely diagnosis?
|
A. Obstructing mass
B. Portal biliopathy
C. Choledocholithiasis
D. Biliary cast syndrome
View Answer
14 Answer D. The ultrasound images show mild biliary dilatation in the setting of a prior liver transplant as well as nonshadowing echogenic material within the extrahepatic bile duct. The hepatic artery shows a “parvus et tardus” waveform, the typical Doppler waveform of an artery downstream from an area of stenosis. Because of the biliary epithelium’s reliance on hepatic arterial perfusion, biliary complications are common in the setting of hepatic arterial stenosis. Biliary cast syndrome (BCS) is among these potential complications and has been reported in 4% to 18% of liver transplants. Casts consisting of bilirubin, collagen, bile acids, and cholesterol form within the bile duct lumen and lead to biliary obstruction.
BCS is associated with increased morbidity, mortality, and graft rejection. The increased echogenicity within the common duct in this case is typical of biliary cast syndrome. A noncontrast CT image shows tubular hyperattenuating material within the biliary tree also representing cast. Given the constellation of findings typical of BCS, choledocholithiasis (answer choice C) and an obstructing mass (answer choice A) are less likely. Portal biliopathy (answer choice B) is biliary obstruction that can occur in the setting of cavernous transformation of the portal vein. The numerous collateral vessels formed following thrombosis of the main portal vein in the porta hepatis result in biliary obstruction.
|
Reference: Gor NV, Levy RM, Ahn J, et al. Biliary cast syndrome following liver transplantation: predictive factors and clinical outcomes. Liver Transpl 2008;14(10):1466-1472.
15 Which of the following can cause “pseudo-sludge” in the gallbladder?
A. Posterior acoustic enhancement
B. Side lobe artifact
C. Mirror image
D. Speed displacement
View Answer
15 Answer B. A strong reflector located outside the main ultrasound beam may generate echoes that are detectable by the transducer. These echoes are falsely displayed as having originated from within the main beam. This artifact is known as the side lobe artifact. It is more likely to be recognized when the misplaced echoes overlap a structure that is normally anechoic, such as the gallbladder. Therefore, in imaging of the gallbladder, which is normally anechoic, the side lobes can produce an artifactual appearance of sludge.
References: Bushberg JT, Seibert JA, Leidholdt EM. The essential physics of medical imaging, 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2011:566-567.
Feldman MK, Katyal S, Blackwood MS. US artifacts. RadioGraphics 2009;29(4): 1179-1189. doi:10.1148/rg.294085199.
16 Which of the following anatomic structures is primarily responsible for the artifact shown by arrow in this image?
|
A. Diaphragm
B. Lung
C. Liver
D. Pleura
View Answer
16 Answer B. The ultrasound image is of the right upper quadrant showing mirror image artifact. Liver parenchyma is shown both below and above the diaphragm. Mirror image artifacts are generated by the false assumption that an echo returns to the transducer after a single reflection. In this scenario, the primary beam encounters a highly reflective interface. The reflected echoes then encounter the “back side” of a structure and are reflected back toward the reflective interface before being reflected to the transducer for detection. The display shows a duplicated structure equidistant from but deep to the strongly reflective interface.
Gas is the best acoustic mirror in the body because it reflects almost 100% of the ultrasound beam. In right upper quadrant US, the base of the right lung acts as an acoustic mirror. It forms a mirror image of the liver and diaphragm. The trachea is another structure with a large smooth gas interface. It therefore acts as a mirror on scans of the neck.
References: Feldman MK, Katyal S, Blackwood MS. US artifacts. RadioGraphics 2009;29(4):1179-1189.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:20-22.
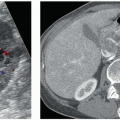
17a A 29-year-old female presents with right upper quadrant pain and fever. US and CT images are shown. Which other organ may be affected in this patient?
|
A. Pancreas
B. Spleen
C. Kidneys
D. Adrenals
View Answer
17a Answer C. The ultrasound image shows multiple coarse shadowing calcifications. At least two of these calcifications are shown to be within a tubular anechoic structure (bile duct). The CT image shows several cystic liver lesions, many with central intraluminal fibrovascular bundles corresponding to portal vein radicals. Many cystic spaces also contain coarse calcifications. These imaging findings are characteristic of Caroli disease.
Caroli disease is also known as communicating cavernous ectasia of the intrahepatic bile ducts and is an autosomal recessive disorder. It results from the arrest of or a derangement in the normal embryologic remodeling of ducts and causes varying degrees of destructive inflammation and segmental dilatation. If the large intrahepatic bile ducts are affected, the result is Caroli disease, whereas abnormal development of the small interlobular bile ducts results in congenital hepatic fibrosis. If all levels of the biliary tree are involved, features of both congenital hepatic fibrosis and Caroli disease are present. This condition has been termed Caroli syndrome. Caroli disease typically manifests as saccular or fusiform cystic dilatations of the intrahepatic bile ducts up to 5 cm in diameter, often containing calculi or sludge.
Autosomal dominant and autosomal recessive polycystic kidney, as well as medullary sponge and medullary cystic kidney, can be seen in association with Caroli disease. Renal cysts are seen with disorders of the ductal plate, and renal developmental abnormalities can be caused by the same genetic determinants.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:99-100.
Levy AD, Rohrmann CA, Murakata LA, et al. Caroli’s disease: radiologic spectrum with pathologic correlation. AJR Am J Roentgenol 2002;179(4):1053-1057.
Santiago I, Loureiro R, Curvo-Semedo L, et al. Congenital cystic lesions of the Biliary tree. AJR Am J Roentgenol 2012;198(4):825-835.
17b What is the characteristic imaging finding seen in this entity?
A. Reverse target sign
B. Cluster of grapes sign
C. Water-lily sign
D. Central dot sign
View Answer




17b Answer D. The presence of portal radicles partially or completely surrounded by dilated bile ducts (known as the central-dot sign) is considered characteristic of Caroli disease. Ultrasound may also show dilated intrahepatic bile ducts with intraductal calculi. Echogenic septa may traverse the lumens of dilated bile ducts, an appearance termed intraductal bridging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree