Horner’s syndrome (HS) occurs when there is interruption of the oculosympathetic pathway (OSP). This article reviews the anatomy of the OSP and clinical findings associated with lesions located at various positions along this pathway. The imaging findings of lesions associated with HS at various levels of the OSP, classified as preganglionic HS (first- and second-order neuron HS) or postganglionic HS (third-order neuron HS), are demonstrated.
Horner’s syndrome (HS) occurs when there is interruption of the oculosympathetic pathway (OSP). This article reviews the anatomy of the OSP and clinical findings associated with lesions located at various positions along this pathway. The imaging findings of lesions associated with HS at various levels of the OSP, classified as preganglionic HS (first- and second-order neuron HS) or postganglionic HS (third-order neuron HS), are demonstrated.
Anatomy of the oculosympathetic pathway
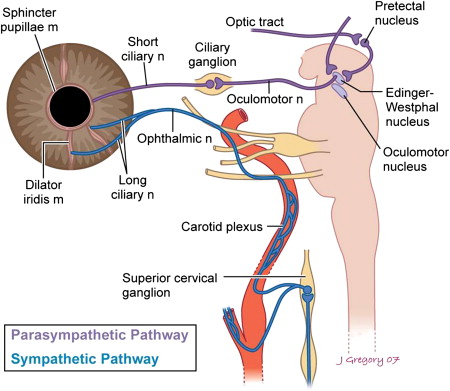
The OSP supplies sympathetic innervation to the sweat glands (ipsilateral body and face), dilator muscles of the eye, and retractor muscles of the upper and lower eyelids. This pathway consists of three neurons and two relay centers (ciliospinal center of Budge-Waller and the superior cervical ganglion).
First-Order Neuron (FON)
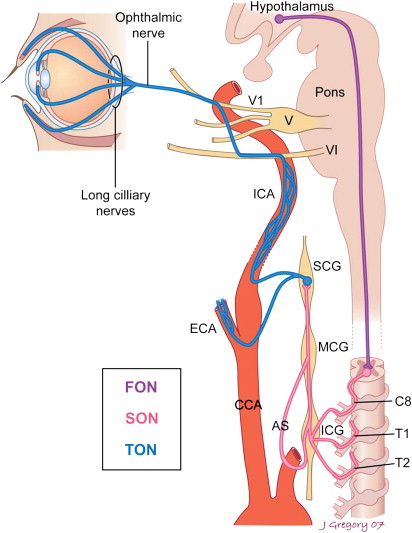
The first-order neuron (FON) of the OSP is located in the posterior lateral aspect of the hypothalamus ( Fig. 1 ). Postganglionic fibers (PGF) from this neuron descend in the reticular formation through the brainstem, cervical spinal cord, and proximal thoracic spinal cord and synapse in the second-order neurons (SON). The SON is located in the intermediolateral (IML) gray substance of the spinal cord at the level C8-T2 (Ciliospinal Center of Budge-Waller).
Second-Order Neuron (SON)
The SON is located in the IML gray substance of the spinal cord between C8 and T2 (ciliospinal center of Budge-Waller) (see Fig. 1 ). The PGF exit in the ventral spinal roots (white rami communicantes) of C8, T1, and T2. These fibers pass through the inferior cervical or stellate ganglion (fusion of inferior cervical and first thoracic ganglia) and middle cervical ganglion without synapsing and eventually synapse in the superior cervical ganglion.
The inferior cervical and first thoracic ganglions are fused in 80% of the population. This results in the formation of a large ganglion called the stellate ganglion. This ganglion (inferior cervical or stellate) is located posterior to the vertebral artery between the transverse process of the C7 vertebra and the first rib. The middle cervical ganglion is at the level of the cricoid cartilage and has two or more connections to the inferior cervical or stellate ganglia. This ganglion will be referred to as the inferior cervical ganglion in this article.
Third-Order Neuron (TON)
The superior cervical ganglion (TON) is located at the level of C2-C3, posterior to the carotid sheath and anterior to the longus colli muscle. There are numerous PGF with many anastomoses; however, only pertinent to a discussion of HS are the anterior fibers, which ascend and travel with the internal and external carotid arteries. The PGF of the TON travel in the adventitia of the internal carotid artery (carotid plexus) for a short distance and then attach to the cavernous sinus. Once in the cavernous sinus they attach to the abducens nerve (CN VI) and then onto the ophthalmic nerve (V1). The fibers then travel with the long ciliary nerve, a branch of the ophthalmic nerve (V1), through the superior orbital fissure (see Fig. 1 ). These fibers innervate the rectractor muscles of the upper and lower eyelids (Müller’s muscles), dilator muscles of the pupil, lacrimal glands, and orbital vasomotor fibers. Fibers traveling with the external carotid artery follow the internal maxillary artery to the face and innervate the sweat glands of the face. Therefore, a lesion distal to the carotid bifurcation will not be associated with significant impairment of facial sweating. There are a few nerve fibers responsible for sweat to the forehead and lateral aspect of the nose that travel with the internal carotid artery (ICA). This explains the loss of sweat production in these areas with lesions distal to the carotid bifurcation.
Horner’s syndrome clinical findings
Johann Friedrich Horner first described the classic clinical triad of symptoms seen in HS, (ptosis, miosis, and anhidrosis) in 1869 ( Fig. 2 ).

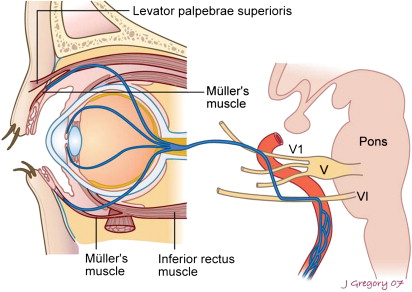
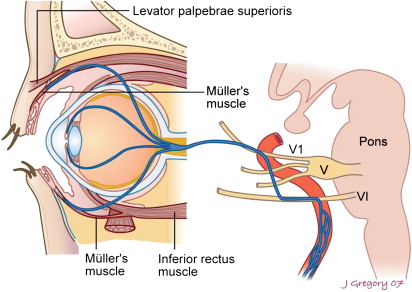
Ptosis refers to a moderate drop of the upper eyelid. The levator palpebrae superioris muscle elevates the upper eyelid. This muscle is innervated by the oculomotor nerve (CN III). Müller’s muscle in the upper eyelid is a thin sheet of smooth muscle arising from the undersurface of the levator palpebrae superioris muscle ( Fig. 3 ). It also elevates the upper eyelid and controls the resting position of the upper eyelid (when the eye is open). It is innervated by the sympathetic nervous system, and therefore, interruptions of the sympathetic nerve supply result in ptosis.
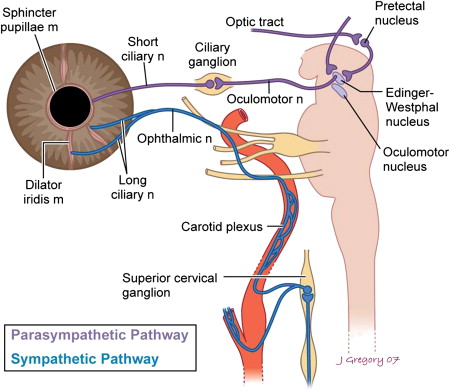
Miosis is a decrease in pupil size as a result of paralysis of the iris dilator muscles. This occurs when there is an interruption of the sympathetic innervation to the dilator muscle of the pupil ( Fig. 4 ). The sphincter and dilator muscles of the pupil are innervated respectively by the sympathetic and parasympathetic systems. When the sympathetic system is interrupted, there are no forces to counteract the sphincter muscle, therefore the pupil will decrease in size.
Anhidrosis occurs when there is interruption of sympathetic innervation to the sweat glands, resulting in a lack of sweat production. Unilateral absence of sweat to the forehead, face, or body is a good indication of HS. Different patterns in the distribution of anhidrosis are associated with FON, SON, and TON HS. Anhidrosis is often not readily noticed by patients and it can be difficult to diagnose, thus it is not a routinely measurable sign.
Other Clinical Findings
Upside-down ptosis is best appreciated when the upper eyelid is in the resting position. Sympathetic fibers innervate retractor fibers in the lower eyelid (also called Müller’s muscle), which arise from the fascial extension of the inferior rectus muscle (see Fig. 3 ). The lower lid will rise slightly in HS (“upside-down” ptosis). This, in conjunction with the upper eyelid changes, causes narrowing of the palpebral fissure and may give the false appearance of enophthalmos (see Fig. 2 ).
Conjunctival hyperemia is a transient early sign of acute HS that is rarely present after the first few weeks. The conjunctiva is the mucous membrane that lines the eyelid and surface of the globe. Sympathetic denervation leads to vasodilatation of the capillaries in the conjunctiva (blood-shot eyes).
Dilation lag refers to slower dilatation of the sympathetic denervated pupil in the dark when compared with the normal pupil. The sympathetic denervated pupil dilates slower than the normal pupil because the dilator muscles are innervated by the sympathetic nervous system.
Dilation lag is best observed when photographs of the eye are taken in the dark after 5 and 15 seconds.
Iris heterochromia occurs when there is interruption of the OSP during the first year of life, resulting in a light-colored iris ( Fig. 5 ). This finding is occasionally seen in HS, particularly in congenital lesions. In patients with brown eyes, the light-colored pupil is usually abnormal, however in patients with light-colored eyes the darker pupil is usually on the abnormal side. This finding, however, is not useful in the perinatal period because iris color is not established until several months of age.

The precise etiology for iris heterochromia in HS has not been established. It has been suggested that an intact OSP is required for pigmentation of the iris to develop in the first year of life, because the formation of pigmentation granules by stromal melanocytes is controlled by the sympathetic nervous system.
Harlequin sign refers to the unilateral facial flushing seen in pediatric patients with congenital HS. The areas that do not flush correspond with anhidrotic areas. There is also a decrease in the skin temperature on the affected side. These findings are the result of impaired sympathetic vasodilatation.
Horner’s syndrome clinical findings
Johann Friedrich Horner first described the classic clinical triad of symptoms seen in HS, (ptosis, miosis, and anhidrosis) in 1869 ( Fig. 2 ).

Ptosis refers to a moderate drop of the upper eyelid. The levator palpebrae superioris muscle elevates the upper eyelid. This muscle is innervated by the oculomotor nerve (CN III). Müller’s muscle in the upper eyelid is a thin sheet of smooth muscle arising from the undersurface of the levator palpebrae superioris muscle ( Fig. 3 ). It also elevates the upper eyelid and controls the resting position of the upper eyelid (when the eye is open). It is innervated by the sympathetic nervous system, and therefore, interruptions of the sympathetic nerve supply result in ptosis.
Miosis is a decrease in pupil size as a result of paralysis of the iris dilator muscles. This occurs when there is an interruption of the sympathetic innervation to the dilator muscle of the pupil ( Fig. 4 ). The sphincter and dilator muscles of the pupil are innervated respectively by the sympathetic and parasympathetic systems. When the sympathetic system is interrupted, there are no forces to counteract the sphincter muscle, therefore the pupil will decrease in size.
Anhidrosis occurs when there is interruption of sympathetic innervation to the sweat glands, resulting in a lack of sweat production. Unilateral absence of sweat to the forehead, face, or body is a good indication of HS. Different patterns in the distribution of anhidrosis are associated with FON, SON, and TON HS. Anhidrosis is often not readily noticed by patients and it can be difficult to diagnose, thus it is not a routinely measurable sign.
Other Clinical Findings
Upside-down ptosis is best appreciated when the upper eyelid is in the resting position. Sympathetic fibers innervate retractor fibers in the lower eyelid (also called Müller’s muscle), which arise from the fascial extension of the inferior rectus muscle (see Fig. 3 ). The lower lid will rise slightly in HS (“upside-down” ptosis). This, in conjunction with the upper eyelid changes, causes narrowing of the palpebral fissure and may give the false appearance of enophthalmos (see Fig. 2 ).
Conjunctival hyperemia is a transient early sign of acute HS that is rarely present after the first few weeks. The conjunctiva is the mucous membrane that lines the eyelid and surface of the globe. Sympathetic denervation leads to vasodilatation of the capillaries in the conjunctiva (blood-shot eyes).
Dilation lag refers to slower dilatation of the sympathetic denervated pupil in the dark when compared with the normal pupil. The sympathetic denervated pupil dilates slower than the normal pupil because the dilator muscles are innervated by the sympathetic nervous system.
Dilation lag is best observed when photographs of the eye are taken in the dark after 5 and 15 seconds.
Iris heterochromia occurs when there is interruption of the OSP during the first year of life, resulting in a light-colored iris ( Fig. 5 ). This finding is occasionally seen in HS, particularly in congenital lesions. In patients with brown eyes, the light-colored pupil is usually abnormal, however in patients with light-colored eyes the darker pupil is usually on the abnormal side. This finding, however, is not useful in the perinatal period because iris color is not established until several months of age.
The precise etiology for iris heterochromia in HS has not been established. It has been suggested that an intact OSP is required for pigmentation of the iris to develop in the first year of life, because the formation of pigmentation granules by stromal melanocytes is controlled by the sympathetic nervous system.
Harlequin sign refers to the unilateral facial flushing seen in pediatric patients with congenital HS. The areas that do not flush correspond with anhidrotic areas. There is also a decrease in the skin temperature on the affected side. These findings are the result of impaired sympathetic vasodilatation.
Classification
HS can be classified as preganglionic or postganglionic, based on the location of a lesion in the OSP with reference to the superior cervical ganglion ( Fig. 6 ).
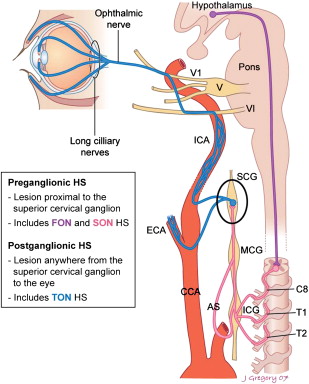
The preganglionic segment is the segment of the OSP proximal to the superior cervical ganglion. It can be further subdivided into two subsegments:
- 1.
The central, or FON, subsegment is located between the hypothalamus and IML before the FON PGF synapse in the ciliospinal center of Budge-Waller.
- 2.
The peripheral, or SON, subsegment refers to the portion of the pathway from the SON before the PGF synapse with the superior cervical ganglion.
The postganglionic, or TON, segment is the portion of the pathway between the superior cervical ganglion and the eye.
To reiterate, the preganglionic segments include both the first- and second-order neurons; the third-order neuron is postganglionic.
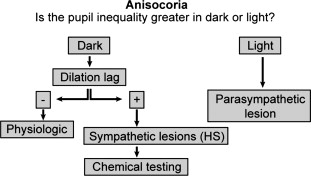
Clinical evaluation
Anisocoria (unequal pupil size) may be a result of aging or sympathetic or parasympathetic dysfunction. Examination of the pupil in the dark will help determine the etiology ( Fig. 7 ). The question to be answered is: “Is the pupil inequality greater in the dark or in the light?” If the inequality is greater in the light, this is consistent with a parasympathetic lesion. Examination of the eye in the dark will help differentiate physiologic anisocoria from sympathetic dysfunction. There is no dilation in patients with physiologic anisocoria. The sympathetic denervated pupil dilates slower than the normal pupil in the dark; therefore, the presence of dilation lag is consistent with interruption of the sympathetic pathway. This diagnosis should be confirmed by pharmacological testing. Patients with physiologic anisocoria do not have dilation lag.