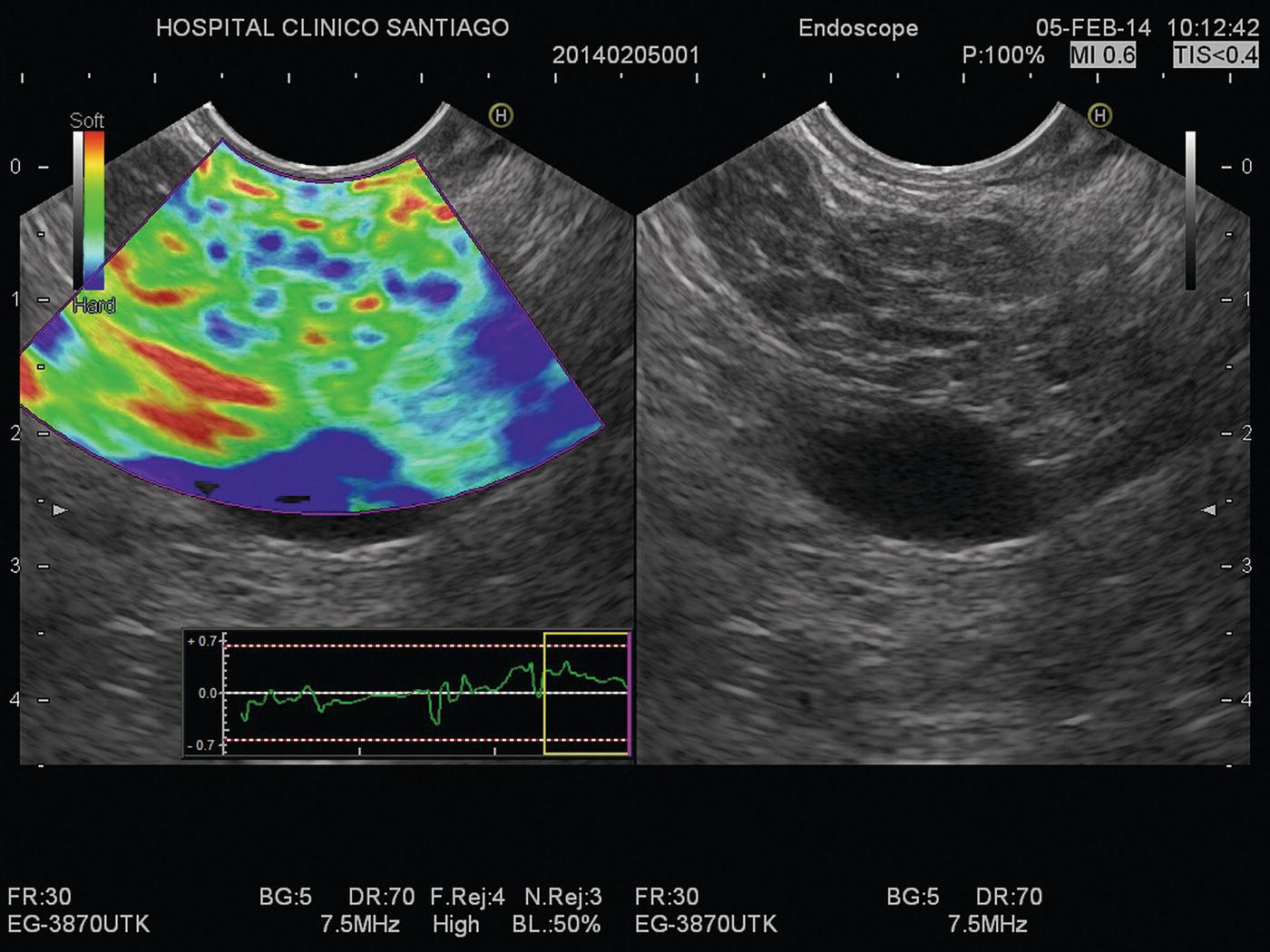
Julio Iglesias‐Garcia, Jose Lariño‐Noia, Daniel de la Iglesia‐García, and J. Enrique Dominguez‐Muñoz Department of Gastroenterology and Hepatology, Health Research Institute, University Hospital of Santiago de Compostela, Santiago de Compostela, Spain The introduction of endoscopic ultrasound (EUS) in clinical practice is an important advancement in the management of a wide variety of diseases. EUS has been demonstrated to have significantly changed the diagnosis and/or management in up to 25–50% of cases. Nevertheless, an accurate diagnosis cannot always be determined using only conventional B‐mode EUS imaging. However, in 80–95% of cases, EUS‐guided tissue acquisition can provide a definitive diagnosis, but there remain a few cases which require efforts to increase this diagnostic yield. Hence, new methods have been warranted, allowing for a more accurate but still noninvasive characterization of lesions, limiting the need for EUS‐guided tissue sampling and guided biopsies of areas with the highest suspicion of malignancy in cases where tissue sampling is still necessary. Among them, EUS‐guided elastography has arisen as a very promising technique. Elastography is a novel technique for tissue characterization, providing a noninvasive method for the evaluation of the mechanical properties of different tissues, in this case tissue stiffness. Elastography has emerged from the development of the fremitus technique in breast ultrasonography, which demonstrates that healthy breast tissue vibrates more than solid malignant lesions, despite their isoechoic appearance under B‐mode ultrasound. It is well known that inflammatory processes and neoplastic infiltration induce changes in normal tissue structure, thus causing a change in its elasticity, becoming harder or softer. This is a qualitative method for evaluating tissue stiffness based on external or internal generated force, which in EUS is based on the internal force concept. The measurement algorithm is based on the extended combined autocorrelation method. It is based on stiff tissues presenting lower strain so that they deform less under compression when compared with soft tissues. With strain elastography, the compression‐induced tissue deformations within a region of interest (ROI) are assessed in a comparative fashion and are visualized using a transparent color overlay on the B‐mode image. As previously described, several different diseases, including cancer, can induce alterations in tissue stiffness. In this chapter we focus on how to perform an EUS‐guided elastography study, and briefly mention the main indications of this method, according to the clinical evidence. Before describing the method, we need to initially emphasize that no specific preparation of the patient is needed for performing EUS‐guided elastography. Patient positioning does not differ from that required for the performance of a standard EUS exploration. Elastography evaluates stiffness through the application of slight compression, using the tip of the scope (ultrasound part), to the targeted tissue (lesion) and recording the resulting tissue displacement from the region evaluated. Basically, elastography relies on the quantification of the compression‐induced deformation of the structures in the B‐mode image using the degree of deformation as an indicator of tissue stiffness. During EUS, together with the compression performed by the tip of the scope, we also use the physiologic vascular pulsations and respiratory movements to obtain important additional vibration and compressions necessary for the study. Small structural deformations will be caused by compression and be detected on the B‐mode image, so that the strain is smaller in hard tissues than in soft tissues. To optimize and have confidence in the evaluation, large blood vessels should be avoided because movement of blood produces an artificially large displacement or softness. A ROI is used to define an area in a similar way to Doppler evaluation (Figure 48.1). As described previously, little compression is necessary because the regular pressure variation from the pulsation of adjacent vessels is sufficient. The size of the ROI is crucial because it needs to be sufficiently large to include both the pathologic tissue and surrounding normal tissue as reference (Figure 48.2). The best image quality has been documented when the area under study covers 25–50% of the ROI. At this point, there are two different options for EUS‐guided elastography: qualitative and quantitative evaluation. We describe both methodologies.
48
How to do EUS Elastography
Introduction
Technique

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree