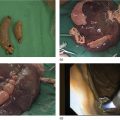
M. Phillip Fejleh and Wilson T. Kwong Division of Gastroenterology, University of California San Diego Health Sciences, La Jolla, CA, USA Endoscopic retrograde cholangiopancreatography (ERCP) and certain endoscopic ultrasound (EUS) procedures can be challenging when managing pancreaticobiliary diseases in patients with altered gastrointestinal tract anatomy. A regularly encountered situation is the need for ERCP in a patient with prior Roux‐en‐Y gastric bypass (RYGB). ERCP via deep balloon‐assisted enteroscopy can be considered but has limited success rates even when performed by expert endoscopists and therapeutic options and accessories are very limited. Laparoscopy‐assisted ERCP is also feasible but requires laparoscopy and coordination with a surgeon. Endoscopic ultrasound‐directed transgastric ERCP or EUS (EDGE) was developed to overcome the difficulty of these situations by using a lumen‐apposing metal stent (LAMS) to create a fistula tract between the gastric pouch and the excluded stomach after gastric bypass. This technique allows for standard ERCP or EUS interventions in the duodenum. EDGE can be performed in a single session for patients with urgent indications for ERCP including cholangitis, or it can be staged into two or more sessions to allow for maturation of the fistula tract for increased safety in patients who do not require urgent intervention. Practice patterns continue to evolve but EDGE can be considered as first‐ or second‐line management for patients with RYGB who require ERCP. Risks and benefits and all three approaches should be discussed with the patient and a bariatric surgeon for shared decision‐making. The patient should also be counseled on the possible risk of weight regain and persistent fistula (though uncommon). When EDGE is undertaken, it should be performed by an endoscopist experienced in interventional EUS as well as ERCP. The EDGE procedure can be performed on an inpatient or outpatient basis, and this will likely be determined in most cases by the nature of the patient’s condition and the indication for the procedure. General anesthesia is recommended given the procedure duration and aspiration risk, and periprocedural antibiotics should be considered given the transmural nature of the procedure and biliary instrumentation. Available cross‐sectional imaging should be reviewed to assess the proximity of the excluded stomach to the gastric pouch and also assess other findings that may be a contraindication to EDGE (ascites, large distance between gastric pouch and excluded stomach, malignancy, and to verify gastric bypass anatomy vs. other bariatric surgery). An upper endoscopy should be performed to clearly define the anatomy. Next, a linear therapeutic echoendoscope is advanced to the gastric pouch to locate the excluded stomach under ultrasound imaging and to find a suitable window for gastro‐gastric fistula creation (Figure 55.1). The excluded stomach can contain fluid in which case it is easy to identify but may also appear as collapsed folds of the gastric wall without a clear lumen. A site for fistula creation should be identified without intervening vessels and at a site which is ideally 10 mm or less from the gastric pouch. Once a site has been chosen on EUS, the site should be verified endoscopically to ensure the site is within the gastric pouch and not within the esophagus or jejunum as a fistula from the pouch is preferable.
55
How to Perform Endoscopic Ultrasound‐directed Transgastric Endoscopic Retrograde Cholangiopancreatography (EDGE)
Introduction
Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree