Case presentation
A 3-month-old male presents with what the parents describe as fussiness since yesterday. The child has had nasal congestion over the past few days so they took him to an emergency department 1 day ago, where he had a respiratory syncytial virus test that was negative and a chest x-ray that was reported to be unremarkable, per the parents. The parents noted that, after discharge from the facility, the child appeared to have pain when his left leg was manipulated, and this has persisted over the past 24 hours.
Physical examination reveals a well-appearing child in no obvious distress. He is afebrile, with a heart rate of 150 beats per minute, a respiratory rate of 36 breaths per minute, and a room air oxygen saturation of 98%. Blood pressure was not obtained. He has no obvious signs of trauma and is moving all of his extremities without difficulty. The remainder of his physical examination is unremarkable until you palpate the proximal portion of his left lower leg—this action elicits crying from the child.
Imaging considerations
Imaging plays a critical role in the evaluation of nonaccidental trauma (NAT). There are guidelines promulgated by the American College of Radiology (ACR) and the American Academy of Pediatrics that are designed to guide the clinician in choosing appropriate imaging for children who may have sustained NAT.
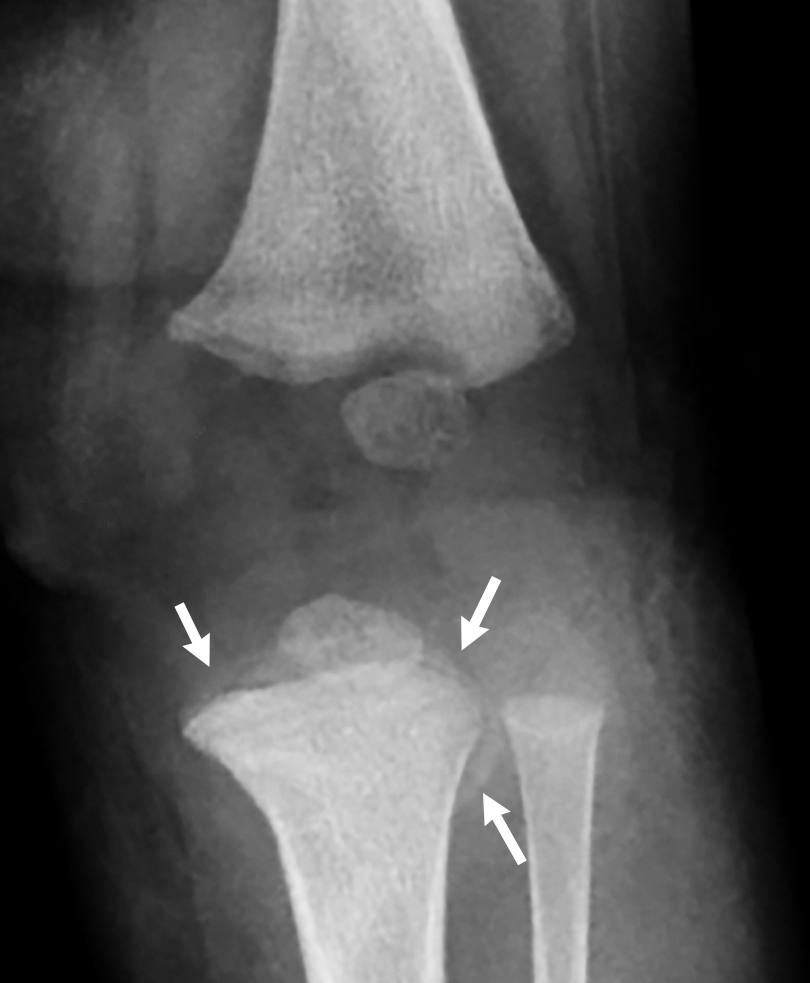
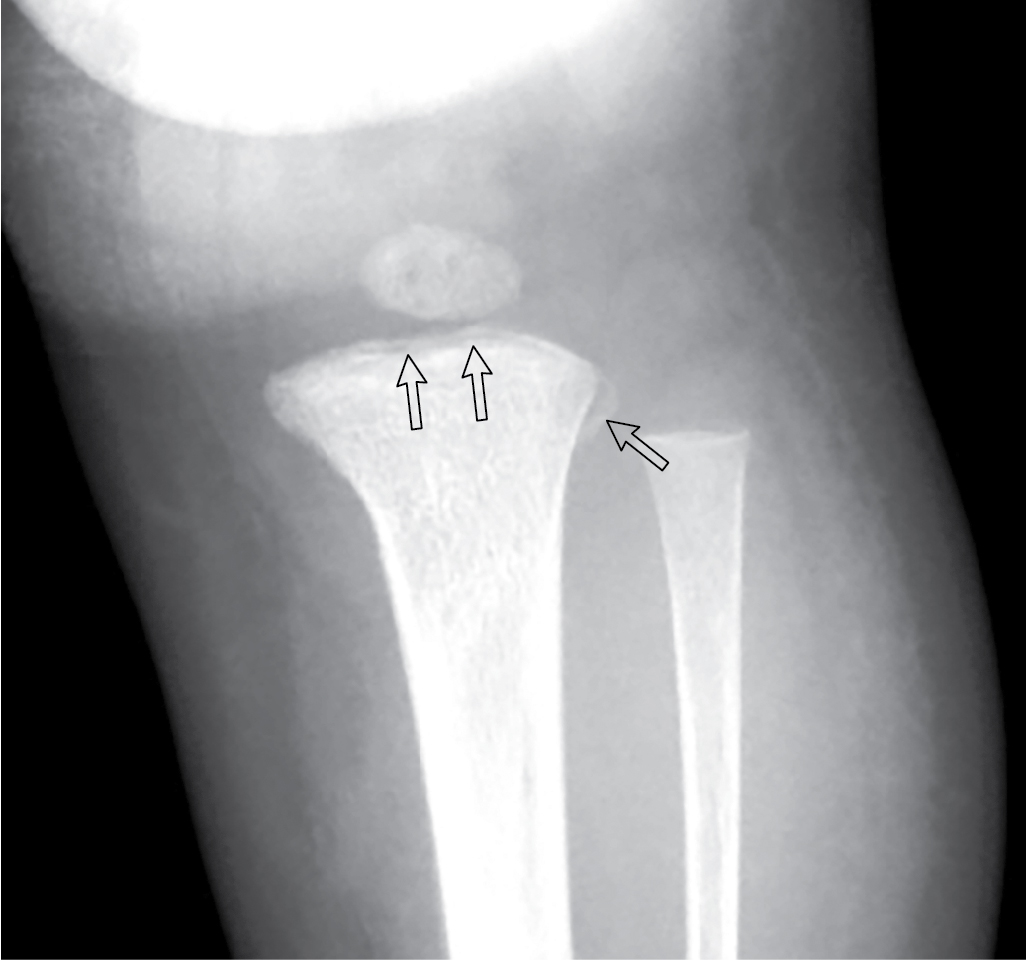
After cutaneous findings, such as bruising, fractures are the second most common manifestation of NAT, especially in children under 18 months to 2 years of age. Fractures in children with NAT can be seen in every location, and while no fracture is absolutely diagnostic of abuse, there are radiographic patterns that suggest NAT. Any fracture raises the suspicion of abuse in the setting of an absent, inappropriate, or changing history. Fractures with high specificity for abusive injury include rib fractures in young children, particularly posterior rib fractures; multiple fractures at various stages of healing without underlying metabolic bone disease or skeletal dysplasia; classic metaphyseal fractures; scapula fractures; sternum fractures; and spinous process fractures. Metaphyseal fractures, colloquially called “bucket handle fracture” or “corner fracture,” are the result of shearing forces applied to long bones and generally not the result of falls. , , These injuries are highly specific for NAT in children under 1 year of age. , , Common locations for these fractures include the distal femur, distal humerus, and proximal tibia and fibula.
Posterior and lateral rib fractures have also been found to have high association with NAT in children under 1 year of age. , These injuries occur when the thorax is squeezed. One study found that posterior rib fractures have a positive predictive value of 95% for NAT that increased to 100% when clinical history was taken into account. , Interestingly, anterior rib fractures have been rarely reported in association with cardiopulmonary resuscitation (CPR), and whether or not the two-thumb CPR technique commonly employed in infant CPR administration leads to an increase in posterior rib fractures remains to be determined. The pliability of the pediatric rib cage makes rib fractures, outside of NAT, rare, and rib fractures in various stages of healing are highly specific for NAT, especially in the absence of metabolic or skeletal disease.
Abusive head trauma is a common form of nonaccidental injury in the pediatric population and is a leading cause of death in children under 1 year of age. , , , Mechanisms of injury vary and can produce both fractures and intracranial hemorrhage, although a fracture may or may not be associated with intracranial hemorrhage. Neuroimaging, both computed tomography (CT) and magnetic resonance imaging (MRI), plays an important role in the acute management of a patient with suspected NAT as well as assists with patient prognosis. Isolated, linear skull fractures or isolated intracranial injuries are not specific for NAT, and linear skull fractures occur in both accidental and abusive injuries. Therefore, correlation with the clinical history and evaluation are necessary, and one should consider further evaluation with a skeletal survey if there is a lack of a credible history to explain the injury, , , , Multiple skull fractures, fractures that cross suture lines, or bilateral skull fractures are radiographic features significantly associated with abusive head trauma. , Subdural hematomas are the most common intracranial finding associated with NAT but are not specific. , , Correlation with history, physical examination, laboratory, and other radiographic findings is critical to help establish if the presence of an intracranial hemorrhage is due to NAT.
There are other underlying metabolic and genetic conditions that may mimic the radiographic findings of NAT. For example, patients with osteogenesis imperfecta are more susceptible to fractures. However, metabolic bone disease will have predictable patterns that can be seen on imaging. Additionally, fractures due to NAT are far more likely to occur as opposed to fractures due to a metabolic abnormality. ,
Plain radiography
The radiographic skeletal survey is an initial, integral, imaging study utilized for the evaluation of children with suspected NAT. There are practice parameters that have been promulgated by the ACR and the Society for Pediatric Radiology recommending the views for a skeletal survey in children under the age of 2 years with suspected NAT. , , , Each anatomic region should be imaged separately, not combining separate regions such as the humerus and forearm and not obtaining views of the right and left extremities together. Further dedicated imaging of areas for clarification of initial imaging findings from the skeletal survey should be performed, for example, addition of lateral views and views coned down to a region of interest such as the wrist or knee. Complete skeletal survey views include the following: , , ,
| APPENDICULAR SKELETON VIEWS | AXIAL SKELETON VIEWS |
| Humeri (AP) | Skull (frontal and lateral, to include cervical spine) |
| Forearms (AP) | Cervical spine (lateral, if not included adequately on lateral skull) |
| Hands (PA) | Thorax (AP, lateral, and bilateral oblique, including ribs, spine) |
| Femurs (AP) | |
| Lower legs (AP) | Lumbosacral spine (lateral) |
| Feet (AP) | Abdomen to include the pelvis (AP) |
A proper and complete skeletal survey has been shown to increase the detection of fractures. , , A “babygram” (single view of the entire skeleton) is NOT adequate for proper visualization of fractures in the evaluation of NAT and should not be obtained. , In children who have equivocal findings or in whom NAT is strongly suspected, a follow-up skeletal survey should be performed 2 to 3 weeks after the initial survey, since this increases the chance of detecting occult fractures and increases the sensitivity and specificity for detecting healing fracture. , , , However, if the initial radiographic evaluation is unremarkable and there is low suspicion of NAT by other evaluation and investigation, repeat imaging is not indicated.
Computed tomography
CT of the head is utilized in instances where there is suspected intracranial injury or if a skull fracture is suspected, either clinically or by history. CT increases sensitivity for detecting skull fractures. , Such injuries are often occult, , so a high index of suspicion for intracranial injury should always be maintained when evaluating children for NAT. Young children (<6 months of age) and any child with signs of trauma to the head, mental status changes, or focal neurologic findings should be considered candidates for neuroimaging. ,
CT of the abdomen is employed if there is suspicion, either clinically or by laboratory findings, of an intraabdominal injury. Intravenous contrast should be utilized. , ,
Magnetic resonance imaging (MRI)
MRI is often used as a follow-up study when there are abnormal findings on initial neuroimaging (CT) and can be used to assist in patient prognosis. , , , MRI may also be utilized in the nonacute setting to evaluate for the presence of parenchymal injury or hemorrhage. , This modality may not be readily available in the emergent setting and may require sedation to complete a meaningful study.
Imaging findings
The chief complaint and physical examination findings prompted plain radiography of the left femur, tibia, and fibula. These images are presented here.
Two-view imaging of the left femur and left tibia-fibula demonstrated metaphyseal abnormalities of the distal femur and proximal tibia in a pattern consistent with classic metaphyseal lesions/fractures ( Figs. 50.1–50.3 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








