Fig. 15.1
Hysterosalpingogram image of a patient with bilateral hydrosalpinges
Ultrasound Appearance
Using standard transabdominal or transvaginal ultrasonography, the appearance of a hydrosalpinx is that of a hypoechoic cystic adnexal mass. Patel et al. evaluated the utility of four specific sonographic findings in diagnosing hydrosalpinges: incomplete septation, short linear projection, tubular shape, and presence of a waist [12]. The authors calculated the likelihood ratio for each finding. The presence of a “waist” in a cystic collection refers to diametrically opposed indentations in the wall of the collection. The waist sign in combination with tubular shape was found in 12 of 26 hydrosalpinges and no other masses (likelihood ratio of between 18.9 and infinity). Small round projections combined with tubular shape was found in 14 hydrosalpinges and one other mass (likelihood ratio of 22.1). The authors concluded that when these combinations are identified in a cystic adnexal mass that does not have solid-appearing areas or features characteristic of hemorrhagic cysts, endometriomas, or dermoid cysts, one can make the diagnosis of hydrosalpinx with a high level of confidence. Waist sign (Fig. 15.2a) and beads on a string (Fig. 15.2b) are classic features of a hydrosalpinx on ultrasound.
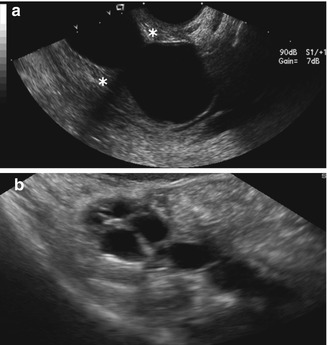
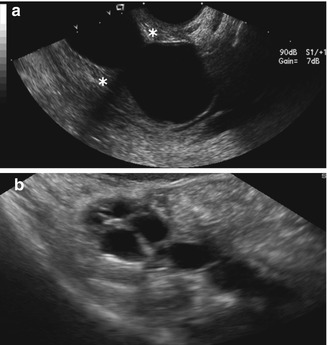
Fig. 15.2
(a) “Waist sign” of a hydrosalpinx, marked by the asterisks, as seen with 2-D ultrasound. (b) “Beads on a string” sign of a hydrosalpinx demonstrated by 2-D ultrasound
Color Doppler Sonography
Color Doppler sonography is used to assess blood flow in a given organ and assesses directional flow as well. The utility of color Doppler to improve the evaluation of hydrosalpinges has been studied. In this regard, the addition of color Doppler does not seem to increase the accuracy of standard 2-D transvaginal ultrasonography in detecting hydrosalpinges. More specifically, Guerriero et al. prospectively evaluated 239 consecutive premenopausal, nonpregnant women who shortly thereafter underwent surgery for adnexal masses, with transvaginal B-mode ultrasonography with and without color Doppler, and CA-125 measurements. The sensitivity, specificity, and positive and negative predictive values were calculated and found to be identical for each category, with color Doppler and CA-125 levels adding nothing to the diagnostic accuracy of 2-D transvaginal ultrasonography alone [13].
Contrast Medium
As a fluid contrast medium can serve as an acoustic window for ultrasonography, one might expect that adding contrast to enhance ultrasound images would be advantageous in the assessment of the fallopian tubes. As previously discussed in this text, this technique is very useful in the basic infertility evaluation to assess tubal patency. In regard to hydrosalpinges, however, there are no studies that directly address the utility of sonographic contrast in the diagnosis of hydrosalpinx, per se. In a study comparing HSG and transvaginal 2-D ultrasonography with an air/saline mixture as the contrast medium in the evaluation of tubal patency, both had the same high concordance with laparoscopy, 86.7 and 86.7 %, respectively [14]. Strandell et al. compared transvaginal sonography utilizing a commercially available contrast agent (Echovist®) and HSG to the gold standard laparoscopic evaluation and found similarly high concordance rates (83 and 80 %, respectively) [15]. Therefore, it appears that transvaginal ultrasound in combination with a contrast medium is a very good method of assessing tubal patency. However, to determine if a patient has a hydrosalpinx, an ultrasound without contrast must first be performed. Otherwise, one might misdiagnose a patient with a hydrosalpinx who instead has distal tubal occlusion alone and no fluid collection within the fallopian tube. In other words, if contrast medium is used initially to evaluate the fallopian tubes either by HSG or via ultrasound, an “iatrogenic” hydrosalpinx may be misdiagnosed as a true hydrosalpinx.
Three-Dimensional (3-D) Ultrasound
Three-dimensional ultrasonography may be helpful in the identification of hydrosalpinges. In one study, 21 consecutive patients scheduled to have laparoscopy were recruited to undergo the 3-D HyCoSy 2 days before the scheduled laparoscopy. Echovist® (Schering AG, Berlin, Germany), the ultrasound contrast medium, was injected into the uterine cavity via a Foley catheter. The flow of the medium in the fallopian tube was captured by using three-dimensional power Doppler mode and was stored for later analysis. The sensitivity of 3-D HyCoSy for detecting tubal patency was 100 % with a specificity of 67 %. The positive and negative predictive values were 89 and 100 %, respectively; the concordance rate was 91 % [16]. Finally, Timor-Tritsch et al. reported using 3-D ultrasound inversion rendering to diagnose hydrosalpinges (Fig. 15.3). Fifty-two patients with fluid-filled adnexal masses suspected of being abnormal fallopian tubes were scanned by two-dimensional and 3-D transvaginal ultrasound. The acquired volumes were then “inverted” to display a cast-like appearance of the fluid-filled structures. The authors concluded that the rendered images increased their confidence in diagnosing hydrosalpinges [17]. Therefore, it appears that 3-D ultrasonography is a useful tool for the diagnosis of hydrosalpinges and may be utilized initially, or in addition to 2-D ultrasound imaging when the results from 2-D images are equivocal.


Fig. 15.3
3-D ultrasound inversion rendering image used to identify a hydrosalpinx
Utility of Tubal Surgery
In regard to tubal surgery, patients with a good prognosis are those who have no more than limited filmy adnexal adhesions, mildly dilated tubes (<3 cm) with thin and pliable walls, and a lush endosalpinx with preservation of the mucosal folds [18]. The mean cumulative pregnancy rates reported after terminal salpingostomy overall is approximately 30 %, with an ectopic pregnancy rate of 5 %. However, in poor prognosis patients with large hydrosalpinges, thick non-pliable walls, and loss of luminal rugae, the cumulative pregnancy rate may be as low as zero. In comparison, the pregnancy rates following terminal salpingostomy in good prognosis patients who are younger and have a more conserved tubal anatomy may be as high as 80 % [19, 20]. Unfortunately, it is difficult to determine the presence of rugal folds with ultrasonography. This is better evaluated via hysterosalpingogram. Nevertheless, an increased tubal diameter is associated with a greater destruction of tubal rugae and a more rigid tube. Therefore, ultrasonography is a reasonable tool for the assessment of patients for tubal surgery with a hydrosalpinx. However, pregnancy rates with IVF exceed the chances for pregnancy with tubal surgery except for the patients with the best prognosis after surgery.
Assisted Reproduction
Hydrosalpinges have been shown to have an adverse effect on both pregnancy and delivery rates in women undergoing IVF. Similar to women with a unilateral hydrosalpinx and a contralateral patent tube who are trying to conceive without IVF, women with either unilateral or bilateral hydrosalpinges who are undergoing IVF may experience drainage of hydrosalpinx fluid into their uterine cavities with adverse reproductive consequences. In fact, this phenomenon has been widely studied. A meta-analysis of 6713 IVF cycles compared the pregnancy outcomes of women with and without a hydrosalpinx. This study found that the presence of a hydrosalpinx was associated with approximately a 50 % reduction in pregnancy rates and a twofold increase in the risk for spontaneous abortion [21]. Another large study of women with tubal disease who either did or did not have a hydrosalpinx revealed similar results [22




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree