Case presentation
A 13-year-old male is referred to the Emergency Department by his primary care provider. The patient has had left hip pain for the past week, which has progressively interfered with his daily activities, such as sports, and now has made ambulation difficult. He has had subjective fever but no recent illness and denies any trauma. There has been no back pain, abdominal pain, incontinence, weakness, or numbness. The pain radiates from his left hip to the superior aspect of his left knee.
On examination, the patient is a pleasant teenager in no distress. He has a temperature of 100.2 degrees Fahrenheit, a heart rate of 112 beats per minute, a respiratory rate of 20 breaths per minute, and a blood pressure of 120/76 mm Hg. His physical examination reveals no obvious abnormalities, as he is sitting up on the hospital bed. His leg lengths are equal. He is able to ambulate but when doing so states that this produces left lateral hip pain, pointing to the anterior-lateral aspect of the superior iliac crest. When his left leg is examined, he has good range of motion of the leg at the hip joint; he is able to flex and extend the leg without difficulty, but when the knee is flexed and the leg (at the hip joint) is either abducted or adducted, pain is produced at the superior aspect of the left hip. There is no erythema, swelling, warmth, or signs of trauma. He has no abdominal pain or back pain and has a normal genital examination.
Imaging considerations
Plain radiography
This imaging modality is most commonly employed in patients with musculoskeletal complaints, given the low ionizing radiation exposure relative to other modalities and general availability. Plain radiography is useful in investigating alternative causes of pain in patients with suspected osteomyelitis, such as fractures. For osteomyelitis, however, radiography is less useful in the acute period. Changes associated with osteomyelitis will not be evident on plain radiography immediately. Associated soft tissue swelling may be seen approximately 3–4 days into the course of the illness and cortical destruction may not be evident for 10–14 days after onset of the infection. Osteopenia may generally be seen after 30%–50% loss of mineralization. Osseous radiographic findings of osteomyelitis initially include subperiosteal resorption, followed by bone lucencies, then irregular destruction with new periosteal bone formation.
Computed tomography (CT)
CT is not a first-line imaging modality for pediatric musculoskeletal infection, as magnetic resonance imaging is a superior modality for this purpose and also due to ALARA principles. CT may be employed as a follow-up examination once the diagnosis of osteomyelitis has been established. This modality may be useful to delineate cortical destruction, periosteal reaction, and the presence of an abscess; intravenous contrast should be used. , ,
Magnetic resonance imaging (MRI)
Magnetic resonance (MR) imaging is the imaging modality of choice to detect osteomyelitis. This modality can detect cortical changes associated with edema and destruction and can also be used to differentiate between acute and chronic osteomyelitis. , , Contrast-enhanced (gadolinium) and noncontrast images may be obtained, but gadolinium use will delineate abscesses. , , , There have been conflicting reports on the routine use of gadolinium for the detection of osteomyelitis. One study found that the sensitivity of osteomyelitis detection using pregadolinium and postgadolinium images was 89% and 91% and the specificity was 96% and 96%, respectively, although gadolinium did increase the ability to detect abscesses. , However, a study of patients 18 months of age and younger with Staphylococcus aureus osteomyelitis found that gadolinium-enhanced imaging significantly improved the detection (100% sensitivity) of osteomyelitis either isolated to the epiphyseal cartilage or combined with metaphyseal and diaphyseal involvement over noncontrast imaging. As the noncontrast imaging showed only a 22% sensitivity for isolated epiphyseal disease and a 44% sensitivity for epiphyseal and metadiaphyseal involvement, the authors recommended contrast-enhanced imaging in children under 18 months of age in communities where community-acquired Staphylococcus aureus is endemic. In general, if there is suspicion of an abscess in very young children with osteomyelitis, or if spinal osteomyelitis is suspected, gadolinium should be used. , , The decision to use gadolinium can be made jointly by consulting Pediatric Radiology and Pediatric Orthopedics and may be institution dependent. While MRI is an excellent imaging test to detect osteomyelitis, disadvantages include availability and, often, the need for sedation.
Ultrasound (US)
This modality is generally available, avoids ionizing radiation, and is less costly than MRI. US has been used to evaluate patients for osteomyelitis and subperiosteal abscess. , Sonographic features suggestive of osteomyelitis include muscle thickening, soft tissue swelling, thickening of the periosteum, and periosteal elevation. US cannot distinguish between pus and sterile fluid. ,
Radionucleotide scanning (bone scan)
Utilizing technetium 99 m methylene disphosphonate, bone scanning can demonstrate hyperemia and focal increased uptake of this bone agent suggestive of infection and can be utilized to detect multiple areas of possible infection. A three-phase technique (angiographic phase, blood pool phase, and late phase) is used. However, it can be more difficult with this modality to distinguish between other etiologies that will produce abnormal scan findings, such as neoplasm or trauma. , ,
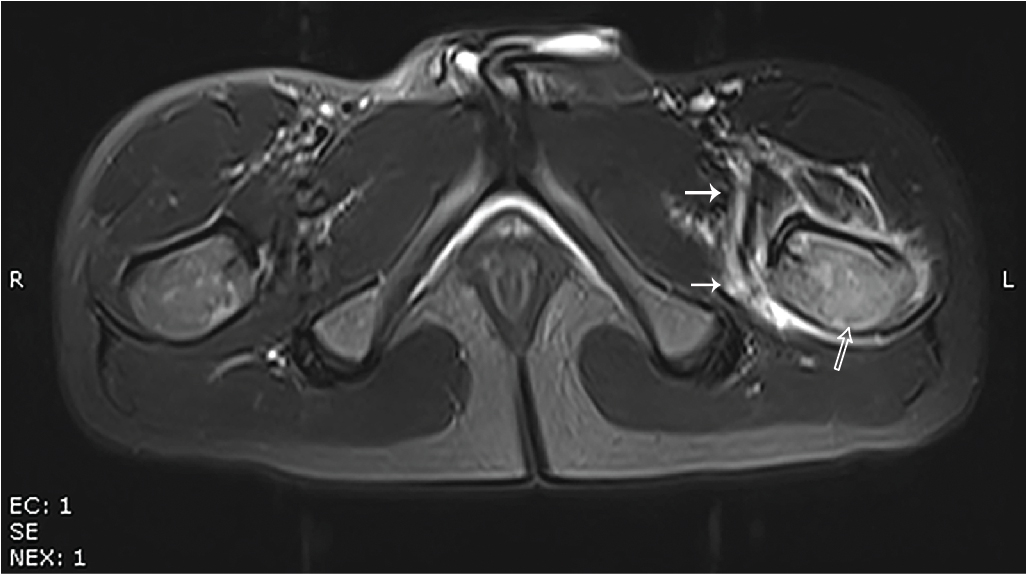
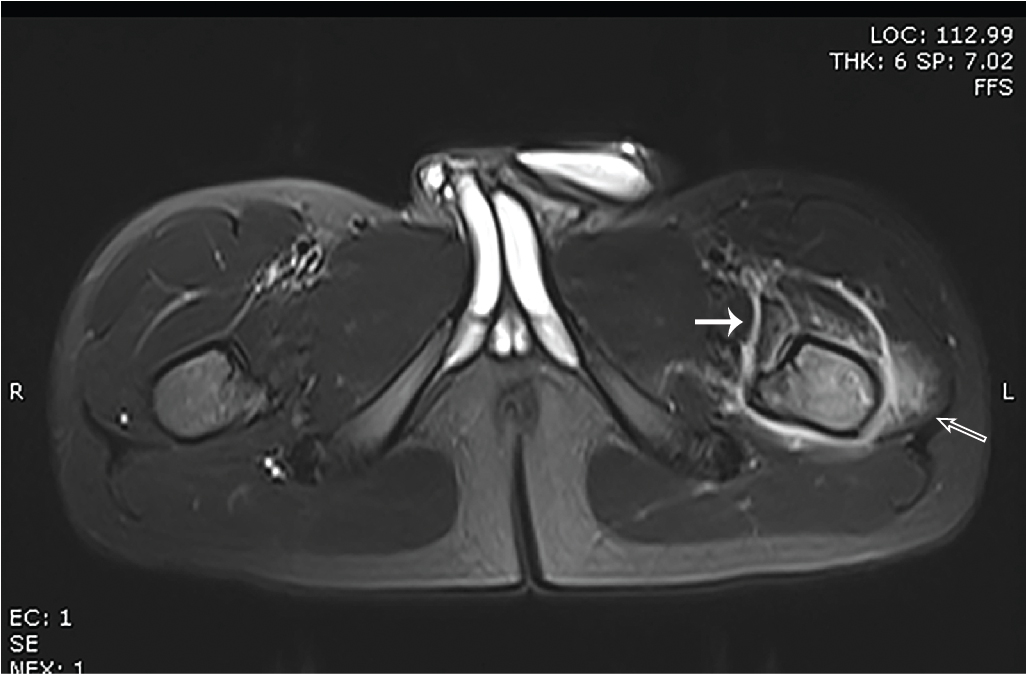
Imaging findings
Plain radiography of the pelvis (two views: anterior-posterior and frog lateral) was obtained and no radiographic abnormality was noted ( Figs. 74.1 and 74.2 ). Laboratory studies were obtained, and given these results, MRI of the hips and femurs was performed. Selected images from this study are provided. There is abnormal bone marrow signal intensity and abnormal enhancement in the left femur, greatest proximally but extending into the diaphysis. Within the proximal femoral diaphysis a focal fluid collection with surrounding enhancement suggests a bone abscess. Surrounding edema in the soft tissues is greatest proximally, with edema and enhancement in adjacent musculature, also consistent with myositis ( Figs. 74.3–74.8 ).