Chapter 3
Image Formation and Radiographic Quality
After completing this chapter, the reader will be able to perform the following:
1. Define all the key terms in this chapter.
2. State all the important relationships in this chapter.
3. Describe the process of radiographic image formation.
4. Explain the process of beam attenuation.
5. Identify the factors that affect beam attenuation.
6. Describe the x-ray interactions termed photoelectric effect and Compton effect.
7. Define the term ionization.
8. State the composition of exit radiation.
9. State the effect of scatter radiation on the radiographic image.
10. Explain the process of creating the various shades of image brightness and densities.
11. Describe the necessary components of radiographic quality.
12. Explain the importance of brightness and density to image quality.
13. Explain the importance of contrast to image quality.
14. Differentiate between high-contrast and low-contrast images.
15. Explain the importance of spatial resolution and recorded detail to image quality.
16. Explain the importance of both size and shape distortion to image quality.
17. Compare and contrast attributes of a digital and film image.
18. Explain the digital characteristics of matrix and pixels.
19. Compare the dynamic range capabilities between digital and film-screen imaging.
20. Recognize the effect of quantum noise and scatter on image quality.
21. Discuss the effects of image artifacts on radiographic quality.
22. Differentiate between the characteristics of a digital and film image.
Image Formation
Differential Absorption
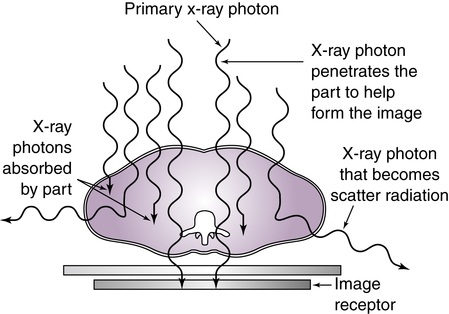
The process of image formation is a result of differential absorption of the x-ray beam as it interacts with the anatomic tissue. Differential absorption is a process whereby some of the x-ray beam is absorbed in the tissue and some passes through (transmits) the anatomic part. The term differential is used because varying anatomic parts do not absorb the primary beam to the same degree. Anatomic parts composed of bone absorb more x-ray photons than parts filled with air. Differential absorption of the primary x-ray beam creates an image that structurally represents the anatomic area of interest (Figure 3-1).
Beam Attenuation
Absorption
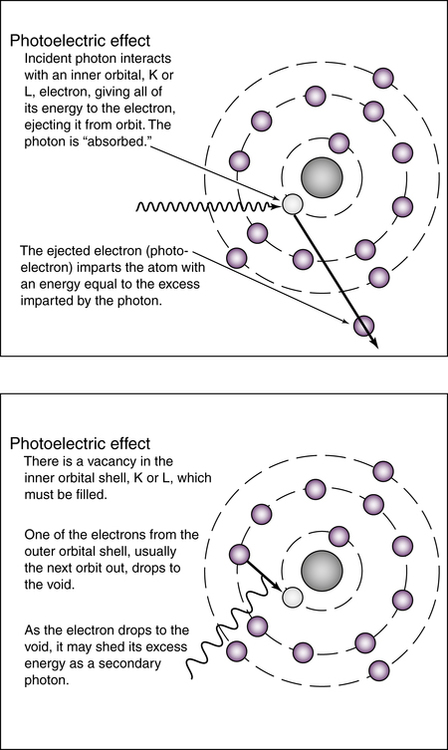
With the photoelectric effect, the ionized atom has a vacancy, or electron hole, in its inner shell. An electron from an outer shell drops down to fill the vacancy. Because of the difference in binding energies between the two electron shells, a secondary x-ray photon is emitted (Figure 3-2). This secondary x-ray photon typically has very low energy and is unlikely to exit the patient.
Scattering
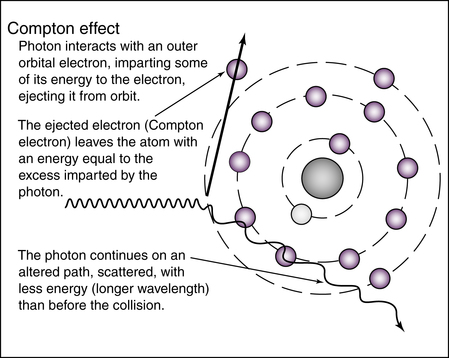
Some incoming photons are not absorbed but instead lose energy during interactions with the atoms comprising the tissue. This process is called scattering. It results from the diagnostic x-ray interaction with matter known as the Compton effect. The loss of energy of the incoming photon occurs when it ejects an outer-shell electron from a tissue atom. The ejected electron is called a Compton electron or secondary electron. The remaining lower-energy x-ray photon changes direction and may leave the anatomic part to interact with the image receptor (Figure 3-3).
When a higher kVp is used, the overall number of x-ray interactions with matter decrease because of increased photon transmission. However, the percentage of photoelectric interactions generally decreases at higher kilovoltages within the diagnostic range, whereas the percentage of Compton interactions is likely to increase at higher kilovoltages within the diagnostic range. Box 3-1 compares photoelectric and Compton interactions.
Factors Affecting Beam Attenuation
Tissue Thickness
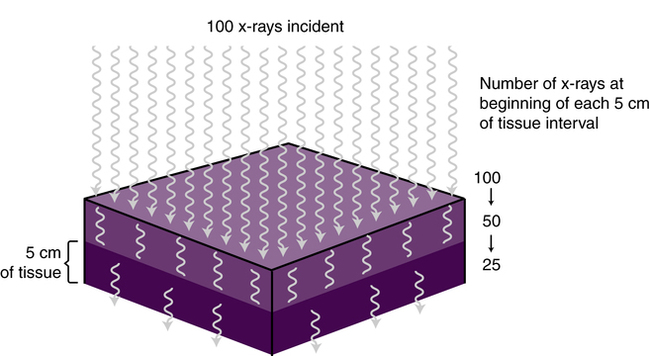
For a given anatomic tissue, increasing its thickness increases beam attenuation by either absorption or scattering. X-rays are attenuated exponentially and generally reduced by approximately 50% for each 4 to 5 cm (1.6 to 2 inches) of tissue thickness (Figure 3-4). More x-rays are needed to produce a radiographic image for a thicker anatomic part. Fewer x-rays are needed to produce a radiographic image for a thinner anatomic part.
X-ray Beam Quality
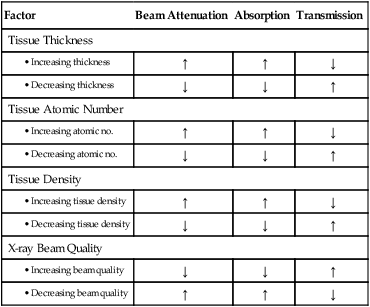
The quality of the x-ray beam or its penetrating ability affects its interaction with anatomic tissue. Higher-penetrating x-rays (shorter wavelength with higher frequency) are more likely to be transmitted through anatomic tissue without interacting with the tissues’ atomic structures. Lower-penetrating x-rays (longer wavelength with lower frequency) are more likely to interact with the atomic structures and be either absorbed or scattered. The kilovoltage selected during x-ray production determines the energy or penetrability of the x-ray photon, and this affects its attenuation in anatomic tissue. Beam attenuation is decreased with a higher-energy x-ray beam and increased with a lower-energy x-ray beam (Table 3-1).
TABLE 3-1
| Factor | Beam Attenuation | Absorption | Transmission |
| Tissue Thickness | |||
| ↑ | ↑ | ↓ | |
| ↓ | ↓ | ↑ | |
| Tissue Atomic Number | |||
| ↑ | ↑ | ↓ | |
| ↓ | ↓ | ↑ | |
| Tissue Density | |||
| ↑ | ↑ | ↓ | |
| ↓ | ↓ | ↑ | |
| X-ray Beam Quality | |||
| ↓ | ↓ | ↑ | |
| ↑ | ↑ | ↓ | |
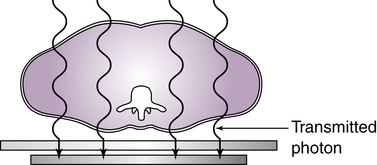
Transmission
If the incoming x-ray photon passes through the anatomic part without any interaction with the atomic structures, it is called transmission (Figure 3-5). The combination of absorption and transmission of the x-ray beam provides an image that structurally represents the anatomic part. Because scatter radiation is also a process that occurs during interaction of the x-ray beam and anatomic part, the quality of the image created is compromised if the scattered photon strikes the image receptor.
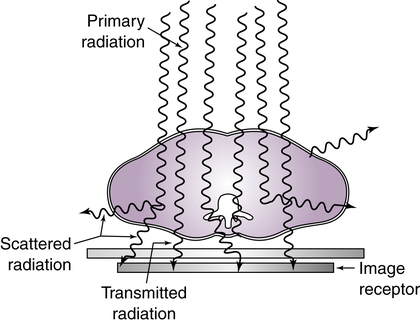
Exit Radiation
When the attenuated x-ray beam leaves the patient, the remaining x-ray beam, referred to as exit radiation or remnant radiation, is composed of both transmitted and scattered radiation (Figure 3-6). The varying amounts of transmitted and absorbed radiation (differential absorption) create an image that structurally represents the anatomic area of interest. Scatter exit radiation (Compton interactions) that reach the image receptor do not provide any diagnostic information about the anatomic area. Scatter radiation creates unwanted exposure on the image called fog. Methods used to decrease the amount of scatter radiation reaching the image receptor are discussed in Chapter 5.
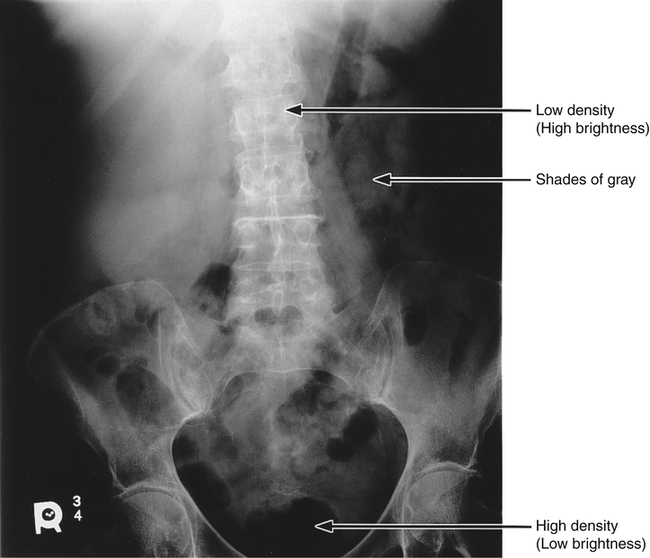
The areas within the anatomic tissue that absorb incoming x-ray photons (photoelectric effect) create the white or clear areas (more brightness or low density) on the displayed image. The incoming x-ray photons that are transmitted create areas of less brightness or high density on the displayed image. Anatomic tissues that vary in absorption and transmission create a range of brightness or shades of gray (Figure 3-7). The various shades of gray recorded in the radiographic image make anatomic tissue visible. Skeletal bones are differentiated from the air-filled lungs because of their differences in absorption and transmission.