IMAGE-GUIDED RADIATION THERAPY FROM A BUSINESS PERSPECTIVE
This chapter outlines the current status of payment policies for image-guided radiation therapy (IGRT) in the context of generally accepted practices of billing for radiation oncology services within the United States system of health care reimbursement.
This chapter is not a detailed primer on how to submit insurance claims for IGRT reimbursement. The intent is to present general considerations and illustrations for how a radiation oncology practice might bill for IGRT services. Health care payment policies and practices by the major health insurers are continually evolving, and the information contained in this chapter will need to be revised and updated periodically. In terms of the federal Medicare program, current payment policy for IGRT is narrowly defined and not likely to expand in the near term due to federal budgetary pressures.
LEARNING OBJECTIVES FOR THIS CHAPTER
Although most current health insurer payment policies are limited in scope and not fully formulated for IGRT, there is value in reviewing the radiation oncology reimbursement model and developing an understanding of how investment in IGRT technology might impact your practice’s revenue model. This chapter focuses on the following learning objectives:
Development of a model format for billing and reimbursement in various practice settings such as outpatient hospital-based practice, professional services only, and freestanding/private office (global billing)
Review of billing framework for radiation oncology, including Current Procedural Terminology (CPT) code structure, use of unlisted CPT codes, types of physician supervision, and National Correct Coding Initiative (NCCI) edits
Examples of how process mapping can be used to help clinical practices optimize their patient care delivery and sustain an efficient daily throughput for IGRT procedures
Best practices in revenue cycle management
IMAGE-GUIDED RADIATION THERAPY: WHY IT IS AN IMPORTANT TECHNOLOGY TO INVEST IN
IGRT can be defined and implemented through various methodologies. There is more than one technique or technical solution for performing IGRT. Theoretically, “image guidance” can be performed either statically or dynamically (in real time), using imaging for monitoring and visually feeding back to the therapist the exact position of the patient’s tumor while the patient is receiving radiation therapy. Billing methodology for IGRT is largely independent of the specific technology used.
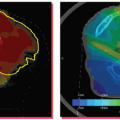
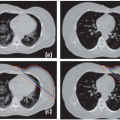
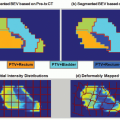
With IGRT, the real-time imaging data can be used to note changes in tumor size and shape over a course of treatment and make real-time adaptations to the treatment plan. Diagnostic imaging technology such as computed tomography (CT) scans, magnetic resonance images (MRIs), or positron emission tomography (PET) scans can be used to guide the radiation treatment setup and delivery. IGRT technology allows for tighter margins around the tumor, minimizing the volume of healthy tissue exposed to the treatment beam. The goal of IGRT is to provide the greatest possible accuracy for tumor targeting, while sparing healthy tissue.
Prior to the development of IGRT, patient positioning and immobilization techniques in radiation therapy relied on the manual dexterity and expertise of therapists to minimize day-to-day variations in patient setup and positioning. Respiratory motion was accounted for by treating a larger margin of healthy tissue around the tumor.
Given the diversity in technologic design approaches for the product offerings from the major vendors, it is not surprising that there is more than one way to implement IGRT capability. Each of the major radiotherapy vendors (e.g., Varian, Siemens, Mitsubishi, Elekta, TomoTherapy, and Accuray) offer IGRT capability in their linear accelerator (linac) product lines. The linac-based systems from Varian, Siemens, and Elekta will likely dominant the provider marketplace, each offering “onboard imagers” comprised of a kilovoltage (kV) x-ray source and a flat panel detector mounted on the rotating linac head and cone beam CT (CBCT). These complete IGRT systems carry a price range of $3.1 to $3.8 million, depending on specific configuration and options chosen.
Additionally, with the latest generation of intensity-modulated radiation therapy (IMRT) linac systems (those <3 years old), IGRT can often be retrofitted to those existing systems, reducing capital investment costs. With the appropriate hardware and software upgrades, each of today’s modern radiation therapy linac platforms can be upgraded and reconfigured to deliver IGRT treatments, thereby extending the useful life of these expensive systems.
IMAGE-GUIDED RADIATION THERAPY IN THE MARKETPLACE
IGRT represents an important evolutionary step in the goal of delivering precision radiotherapy and builds on many of the technical advances that were introduced with the commercialization of IMRT in the mid-1990s, such as digital linac control systems, multileaf collimators (MLCs), flat panel amorphous silicon detectors, and so on.
A recent 2008 MedaCorp survey (unpublished) suggests that <50% of current radiotherapy centers are equipped to deliver IGRT. This suggests an adoption curve not unlike that of IMRT when it was introduced in the mid-1990s. As with IMRT adoption and payment rates in the 1990s, we should expect health insurers’ payment policies for IGRT to lag the marketplace for the immediate future. Overall health care inflation trends will also exert downward pressure on insurers’ willingness to develop IGRT-specific payment rates and expanding insurance coverages.
In the United States health care marketplace, technologic innovation commonly outpaces health insurers’ ability to assess clinical utility and efficacy of these new technologies. As already mentioned, development and implementation of payment policies by health insurers lag the clinical adoption cycle because insurers rely on the published medical literature to evaluate new clinical technology. However, if a new clinical technology offers a compelling and immediate health benefit/outcome, payment policy will develop more rapidly than for technologies that offer only an evolutionary or incremental benefit, such as IGRT. This is somewhat akin to the classic question: Which came first—the chicken or the egg?
A good illustration of the technology adoption rate is the introduction of the MLC. When MLCs were designed and installed on linacs in the mid-1990s, this led to development of IMRT. Leading academic radiotherapy practices then began to purchase MLC-equipped linacs and develop IMRT techniques despite the fact that this added investment was not immediately reimbursable by third-party payors. Nonetheless, during this period, MLC design advanced rapidly from 40-leaf, to 80-leaf, to 120-leaf, causing unexpected and rapid obsolescence for those early adopters.
It took 2 to 3 years after commercial introduction of IMRT technology in the mid-1990s to see IMRT payment policies and reimbursement enacted into Medicare payment policy, which eventually occurred in the federal fiscal year 2000. This then set the benchmark for other health insurers to also develop IMRT payment policies in subsequent years. I would expect a similar time frame for development of IGRT reimbursement.
The Centers for Medicare and Medicaid Services (CMS) have a good track record in evaluating and recognizing clinical innovation and formulating medical policies that foster adoption of new procedures and technologies for the Medicare program and its beneficiaries. Because of this, many of the US’s 1,500+ health insurers rely on Medicare policy formulations to set the pattern.
Thus, not surprisingly with IGRT technology, CMS’s reimbursement policy framework has lagged behind the commercial introduction of IGRT. As of June 2008, the reimbursement/payment rates established for IGRT procedures remain in flux for most major health insurers. It is likely that new CPT codes may need to be established to further differentiate IGRT procedures from a payment policy perspective, even though there are several current CPT codes that can be used to codify IGRT.
A WORD ABOUT VENDOR-GENERATED PRO FORMA REVENUE ANALYSES
If it looks too good to be true, it probably is. It is not uncommon for equipment vendors to offer rosy “pro forma” revenue analyses as part of their sales pitch. The intent of these analyses is to assist customers with calculating estimated payback to help induce and justify the economics of the capital purchase. Such analyses can often be useful, but as with anything, the devil is in the details. In order to assess the reasonableness and validity of such revenue estimates for a specific practice, one must do the following:
Use actual payor mix and caseload volumes from the practice setting.
Use reimbursement rates applicable to the local market and practice type and actual practice patterns.
Ask the physicians to validate the clinical mix of patients for which IGRT would be used now and in the future. Individual physician practice style is also an important factor.
Ask for second opinions from finance professionals who know health care reimbursement and could fairly critique vendor pro formas.
Revenue estimates should generally be conservative in nature, to allow for unknown and uncontrollable variables.
Individual payor payment rates used in the pro forma should not be based on a percentage of the gross charge structure because price-setting policy varies widely from provider to provider.
For the reasons just listed, the financial payback for the capital costs associated with investing in IGRT technology is uncertain, and one should not rely on aggressive revenue estimates that suggest quick payback based solely on the incremental volume of IGRT procedures.
BILLING BASICS AND GENERAL METHODOLOGY
Generally speaking, billing policies and methodology are organized according to the three major practice settings:
Hospital-based (also referred to as “technical” billing)
Non-hospital-based: freestanding centers (global billing)
Non-hospital-based: physician professional fees
Each of these three methodologies has an extensive framework of policies and procedures that are unique and vary by health insurer. A review of this body of knowledge is beyond the scope of this chapter.
It is strongly recommended that your practice employ billing professionals with skill sets that include certification in
coding, an up-to-date understanding of billing regulations and diagnosis coding practices, and the know-how to perform online research. The following knowledge areas need to be well understood by practice managers and are reviewed in a summary fashion in this chapter:
CPT coding structure
Use of unlisted CPT codes
Packaging of IGRT codes and payments
Physical presence requirements
Levels of physician supervision
Billing scenarios by place of service
National correct coding (NCCI) edits
An excellent reference guide for all radiation oncology professionals to have on their bookshelf is the ASTRO/ACR Guide to Radiation Oncology Coding 2007, plus the Guide’s 2008 Supplement. Additional billing reference materials are listed in the References section of this chapter.
CURRENT PROCEDURAL TERMINOLOGY CODE STRUCTURE
In addition to having a working familiarity with the regulations and policies of the major insurers operating in your local market, it is also important to be familiar with the CPT manual, how it is organized, and the section on radiation oncology clinical services, which are listed in the 77xxx range.
The CPT manual also offers limited guidance for possible codes to use in billing of IGRT procedures, and we would also refer the reader to
Chapter 13 of the
ASTRO/ACR Guide to Radiation Oncology Coding 2007, plus the Guide’s 2008 Supplement.
Table 22.1 summarizes the current codes in the 2008 CPT codebook that reflect IGRT procedures.
IMAGE-GUIDED RADIATION THERAPY USING ULTRASOUND (CPT 76950) OR COMPUTED TOMOGRAPHY GUIDANCE (CPT 77014)
The ultrasound and CT codes were available prior to the arrival of linac-based IGRT, with the 76950 code typically used for ultrasound localization at the start of external-beam prostate treatments. These codes are one-time use at the beginning of a course of treatment to localize the target for treatment planning. Port films were used for verification purposes during treatment. With IGRT, they are now used for daily localization of the target volume. So although the frequency of use has changed, the codes and their definitions have remained the same. (Note: The CPT code for “CT guidance” was originally 76370 but was changed to 77014 in 2007.)
IMAGE-GUIDED RADIATION THERAPY USING KILOVOLTAGE GUIDANCE (CPT 77421, STEREOSCOPIC X-RAY GUIDANCE)
For hospital-based practices, IGRT with kV guidance was first reported in 2005 using temporary code C9722, defined as “Stereoscopic kilovolt x-ray imaging with infrared tracking for localization of target volume.” The payment rate was $75.00. In 2006, CPT 77421 was implemented, and C9722 became obsolete. Under Ambulatory Payment Classification (APC) 0257, the payment rate remained at $75.00 for that year. CPT 77421 is currently in use for both the hospital outpatient and physician office settings.
USE OF UNLISTED CURRENT PROCEDURAL TERMINOLOGY CODES (77X99)—NOT RECOMMENDED
In general, the use of “unlisted” CPT codes is not recommended, even though they are listed in the CPT manual. Unlisted codes are defined as those that end in “99.” Today’s claims processing systems look for specificity in coding and will normally reject any codes that are not specific and deny the claim. The usual follow-up is to then resubmit the claim along with the medical record documentation explaining the billed service(s) and its medical necessity.
The
CPT Manual1 states that, “…when a service or procedure is provided that is not listed in a given edition of the CPT codebook, it should be identified by a Special Report and one of the following four unlisted procedure codes: 77299, 77399, 77499, or 77799.… A service that is rarely provided, unusual, variable, or new may require a Special Report in determining medical appropriateness of the service. Pertinent information should include an adequate definition or description of the nature, extent, and need for the procedure; and the time, effort, and equipment necessary to provide the service.…”
If you decide to use an unlisted CPT code for whatever reason, it would be advisable to contact the patient’s health insurer to whom you will be transmitting your claims submission and seek preapproval authorization for the services in question. Keep in mind that you will likely be required to submit detailed medical record documentation to support your request for payment.
REIMBURSEMENT FOR IMAGE GUIDANCE: A WORK IN PROGRESS
As stated earlier in this chapter, current CMS policies reflect a reimbursement philosophy that does not recognize additional separate payment for IGRT in a hospital-based practice setting, despite that fact that linacs equipped to perform IGRT are $500,000 more costly to purchase than non-IGRT linacs.
One can infer that current CMS payment policies result in providers absorbing the incremental costs of acquiring IGRT technology. Medicare is packaging image guidance as part of the overall cost of performing the procedure for which the guidance is needed. This is one part of ongoing federal efforts aimed at controlling national health care cost inflation
and is consistent with how CMS values other procedures. However, providers can decide to bill other insurers for IGRT procedures. But when doing so, providers should expect that IGRT claims will routinely be rejected and should be prepared to aggressively appeal incorrect denials and payment rejections.
As of January 2008, CMS policy states that all image guidance performed in a hospital-based setting is packaged with the radiation therapy procedure performed on that day. Codes affected by policy change are reflected in
Table 22.2. It is important to note that this policy change does not eliminate payment for IGRT in
non-hospital-based practices.
Note on office-based reimbursement: The Deficit Reduction Act (DRA) requirement is to cap Medicare payments for the technical component of office-based imaging services at the rate paid under the Hospital Outpatient Prospective Payment System (HOPPS). Eventually, one can expect that the reimbursement for IGRT in the physician office will be packaged just as it is now for the hospital outpatient setting.
IMAGE-GUIDED RADIATION THERAPY BILLING: DEFINITION OF “PHYSICAL” PRESENCE FOR PHYSICIANS
Physician supervision for IGRT procedures is an important variable from a billing perspective.
There are three levels of physical presence for physicians as defined by CMS regulations, which will impact on the billing of IGRT procedures:
General supervision
Direct supervision
Personal supervision
In hospital and free-standing practice settings, all imaging procedures (IGRT) must be performed under
direct supervision to be billable. See
Table 22.3.
DEFINITIONS OF LEVELS OF PHYSICIAN SUPERVISION
CMS has taken the codes of the American Medical Association’s CPT and its own CMS Healthcare Common Procedure Coding System (HCPCS) and assigned levels to each of them, identifying each level with a numeric key value. Procedures designated by the number 1 must be performed under general supervision, those designated as number 2 require direct supervision, and those designated as number 3 call for personal supervision.
Practices must staff their facilities accordingly in order to comply with these requirements. The levels were first published in the
Federal Register‘s Proposed Rulemaking in 1997.
3 After the comment period, the number 4 was added to designate codes applicable to qualified independent psychologists; 5 and 6 were added for codes applicable to audiologists and physical therapists. Radiologists and radiation oncologists need to concern themselves only with levels 1, 2, and 3.
General supervision: General supervision means that the physician is not necessarily on site. However, the services of the facility are provided under his or her overall supervision and control, and the physician is responsible for the calibration of the equipment, the training of the technologists, and overall operations.
Direct supervision: For an independent diagnostic testing facility (IDTF) that offers services indicating direct supervision, such as CT or MRI with contrast, a physician must be physically on the premises and in the suite of offices where the tests are being performed. In the office setting, the physician must be present in the office suite and immediately available. This is defined as within earshot (not just reachable by beeper and not merely in the same building).
Personal supervision: Where personal supervision is called for, the physician must actually be present in the room with the patient during the performance of the procedure.