Fig. 64.1
Image showing example of surface scanning allowing for navigation with “frameless” systems
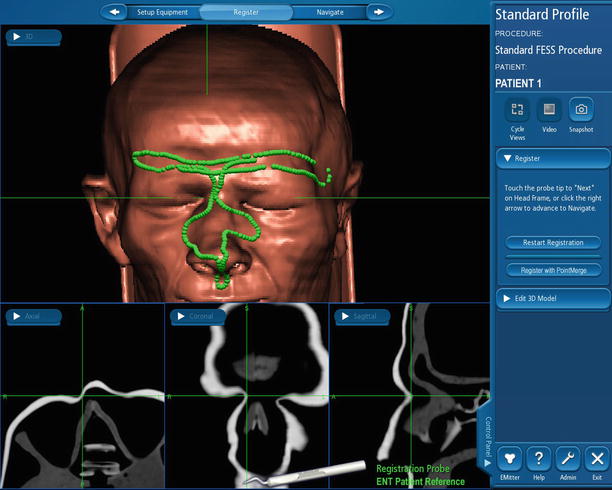
Fig. 64.2
Image showing example of surface scanning allowing for navigation with “frameless” systems
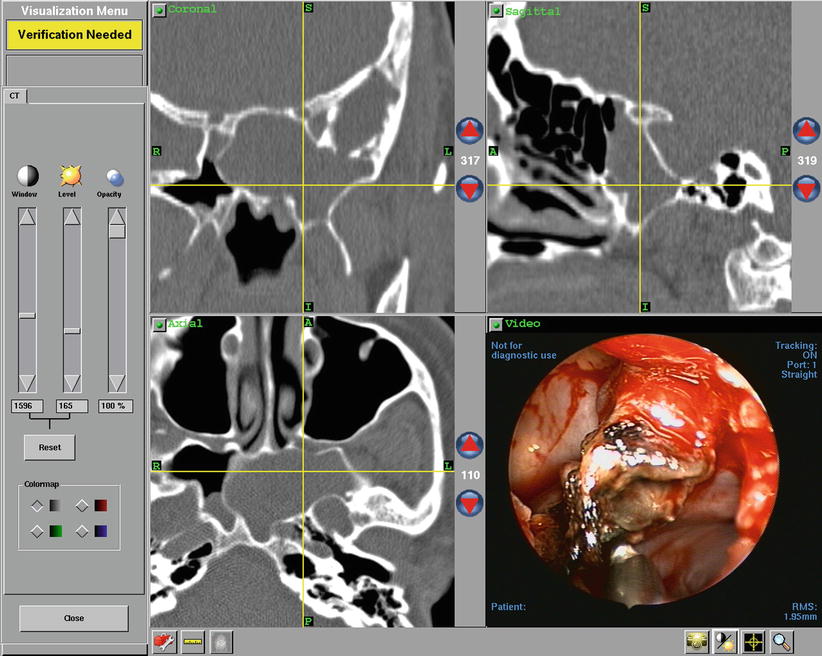
Fig. 64.3
Image demonstrating real time axial, coronal, and sagittal CT views correlating with intra-operative endoscopic image
The optical systems are based on line of sight light-emitting diodes, which are captured in a 3D camera and processed by a computer in a triplanar view similar to the electromagnetic system. Fiducial landmarks are inputted prior to surgery with either a manual probe, laser, or light-emitting diode mask.
Metson et al. prospectively compared an optical system and an electromagnetic system [15]. Despite a significant decrease in operating time with the optical system, this difference was not readily explained. Furthermore, no significant difference was noted in other parameters (e.g., blood loss, complications).
One of the major drawbacks to the optical systems was the need for no line of sight obstruction between the system and the operating room table [16]; however, recent advances have eliminated this barrier [17]. This also required the surgeon to tape down the head of the patient, leaving no maneuverability intraoperatively [12, 18]. Modern systems accommodate head movement, and this has marked implications for surgeons who prefer local anesthesia or intravenous sedation, which was not possible when surgery required absolute immobility.
The registration step generates a correlation between the position of the instrument in the surgical field and the corresponding location on the imaging data set. The location is depicted by on-screen annotations. For instance, a set of crosshairs that moves through the CT slices in concordance with the movement of the instrument. Once registration can be left as is complete and the instruments are calibrated by the system, accuracy is verified by testing and correlating known landmarks on the patient’s face and in the nasal passages. The coordinates are stored and used throughout the procedure to monitor any changes in the accuracy of the device. Normal navigation accuracy for modern systems is commonly between 1.5 and 2 mm [19].
After these preliminary steps, the surgeon can supervise and verify surgical position on the monitor depicting the preoperative three-dimensional image set, often along with an additional frame displaying the endoscopic view of the procedure. Current IGS devices can function with virtually any ESS instrument, allowing the surgeon to elucidate and map out ambiguous or distorted anatomy at critical points in the surgery before proceeding with the next step.
A relatively recent development has been the fusion of CT images with MRI images to create a hybrid image guidance system [20–22]. This allows for adequate visualization of both bony and soft tissue structures and is specifically beneficial in lesions involving the skull base, pituitary, and clivus.
Ultimately, the decision regarding which IGS device to use is individual and institution dependent. Cost and surgeon preference are the major factors involved in deciding which system to use, and the systems on the market today are all quite similar with regard to efficacy, complication rate, and patient postoperative quality of life.
Indications for Image Guidance Systems
Initially, IGS was selected only by tertiary referral centers for revision or unusual sinus cases in which the anatomy was expected to be distorted [23]. However, Anon [6] reported in 1998 that, “because the author’s group has not found it possible to determine preoperatively when computer assistance might be needed, computer-assisted surgery is currently used for all sinus procedures.” As soon as the technology became available in the United States, there was a rapid growth in usage of IGS technology. Metson [24] reported that within the first 2 years of the technology being available, there was a 70 % increase in cases performed and a 92 % increase in the number of surgeons utilizing the technology. As experience has been gained, IGS has now become an integral part of surgery for many otolaryngologists performing ESS in the United States [25].
IGS has not only great value intraoperatively, but it is now a large part of the educational arsenal within teaching institutions, where the ability of the attending surgeon to monitor their resident’s performance, while pointing out specific anatomic features using the guidance system, has greatly advanced the ability to teach sinus surgery in a safe and controlled environment. This was described by Casiano and Numa [26], who observed improved learning curves and safer technique implementation with novice otolaryngology residents practicing on cadavers with the aid of IGS.
Results of Image Guidance in Adult Sinonasal Surgery
IGS has proven most useful in cases involving revision sinus surgery [27, 28], cases involving extensive disease (e.g., extensive sinonasal polyposis), difficult or distorted anatomy (e.g., Onodi cells, narrowed pathways), difficult-to-approach anatomic locations including the frontal and sphenoid sinuses, cases with cerebrospinal fluid (CSF) rhinorrhea, and cases involving benign and malignant sinonasal neoplasms. It has also been enormously beneficial in the growing field of endoscopic skull base surgery [29].
Frontal sinus surgery has traditionally been a challenge for the endoscopic sinus surgeon because it requires using angled telescopes and instruments to visualize and operate within the sinus. The particular challenge of working at unnatural angles to identify the frontal sinus has been the cause of many surgeons’ angst because the skull base, anterior ethmoid artery, and intracranial contents are in such close proximity. IGS now allows the sinus surgeon to identify and work within the frontal sinus with much greater flexibility. In the case of difficult-to-reach frontal sinus disease, Zacharek et al. proposed image-guided trephination as a viable alternative to osteoplastic flap with or without obliteration [30]. In addition, when osteoplastic frontal sinusotomy is considered, IGS has been suggested as a valuable addition to maximize exposure without increasing morbidity [31–34]. Sindwani and Metson reported a series of 24 patients between 1992 and 2003 that demonstrated, for the first time, a reduced complication rate with the use of IGS in frontal sinus obliteration surgery [35].
The sphenoid sinus is commonly thought of as the most dangerous sinus in which to operate due to its close relation to crucial anatomic structures including the carotid artery, intracranial contents, and optic nerve. It is also a gateway to many important intracranial anatomic locations. IGS has greatly improved the ability for surgeons to access the sphenoid sinuses safely and to approach tumors involving areas that previously required craniotomies but now are accessible via a transsphenoidal approach. Otori et al. [36] described the transsphenoidal approach for removal of a pituitary lesion and concluded that this was particularly helpful in patients with narrowed sinonasal anatomy.
As the boundaries are pushed with regard to what is acceptable in endoscopic treatment of intracranial lesions, IGS becomes more and more of a necessity for these complicated transsphenoidal approaches. This route allows midline access and visibility to the suprasellar, retrosellar, and parasellar space while eliminating the large risk of brain retraction and makes possible to treat transsphenoidally a variety of midline skull base and parasellar lesions traditionally approached transcranially. In the hands of experienced otolaryngologists and neurosurgeons, lesions involving the cavernous sinus and posterior fossa are accessible via the transsphenoidal approach [37–39].
IGS has proven to be of great value in the surgical approach to the orbit [40]. White et al. [41] described a transnasal approach with IGS for the drainage of periorbital abscesses. Batra and Lanza [42] described orbital exenteration using the endoscopic image-guided approach which they found helped preserve the ophthalmic artery, thus decreasing bleeding, helping to preserve the eyelid, and helping to preserve the superior and lateral periosteum which facilitate mucosal coverage of the exenterated space. Murchison et al. [43] have recently described the transnasal removal of lesions within the orbital apex, which customarily require orbitotomy and craniotomy approaches.
Results of Image Guidance in Pediatric Sinonasal Surgery
The embryological development of the sinuses leads to distinctive challenges for the pediatric otolaryngologist when dealing with sinonasal disease processes. With sinus development and maturation not completed until late into the second decade, the surgeon must be aware of the unique anatomy involved in pediatric sinus surgery. With this in mind, IGS is a valuable resource to help guide the pediatric surgeon dealing with sinonasal disease.
Due to the relative scarcity of sinonasal surgery in the pediatric population compared to the adult population, there have been no specific studies looking specifically at the safety or efficacy of IGS systems in this age group [44]; however, there are several reports on the use of IGS within the pediatric population, both for common sinonasal processes and for specific disease processes unique to the pediatric population. Postec et al. [45] reviewed their experience with IGS in over 30 patients and discussed its value in assisting with revision cases, polyp removal in children with cystic fibrosis, patients with restenosis of choanal atresia, patients with juvenile nasopharyngeal fibroma, and patients requiring tumor biopsy. Parikh et al. [46] reviewed the largest series of pediatric patients, with 33 patients on whom image-guided sinus surgery was used. Image guidance was only used for advanced sinonasal procedures where there was an anatomic abnormality or disease that extended to the sphenoid sinus, frontal sinus, orbit, or skull base. The most common indications were chronic and acute rhinosinusitis, followed by juvenile nasopharyngeal angiofibroma, and allergic fungal sinusitis, and they had no reported complications with IGS. There have been several other reports [41, 47–49] describing use of image guidance within the pediatric population for cases involving difficult anatomic locations such as the skull base and petrous apex or complicated disease processes including cholesterol granuloma, juvenile nasopharyngeal angiofibroma, and periorbital abscess.
Results of Image-Guided Surgery
The true measurement of any new technology within the medical domain is its ability to improve patient outcomes, decrease complications, and increase postoperative satisfaction. Several retrospective case series have reported lower rates of complications using image guidance systems [23, 28, 35, 50], although this reached statistical significance in only the study performed by Fried et al. [23], who performed a retrospective study on 97 patients and found a significant decrease in complications in the IGS group. In a prospective study performed by Javer and Genoway [51], patients treated with image-guided ESS were compared to non-image-guided ESS. A 31-item questionnaire regarding short-term quality of life measures was used by the authors. They found a significant trend indicating greater quality of life improvement in the short term in the image-guided group relative to the non-image-guided group.
There is some controversy regarding the advantage of using IGS. Tabaee et al. [52] did not demonstrate a difference in overall intraoperative or postoperative complication rates, rates of revision procedures, or postoperative SNOT-20 scores. That review did find a higher incidence of intraoperative CSF leaks in the non-IGS group; however, another review by Tabaee et al. [53] did not find a significant improvement in the rates of successful closure of leaks with IGS. In addition, IGS was found to increase operative time by 15–30 min per surgery and cost on average 500 dollars more per case, with the additional cost involving cases where disposable handpieces and headsets were utilized. IGS has also been associated with higher intraoperative bleeding and minor headset-related complications [23, 54].
While IGS has certain drawbacks, it is universally accepted as a valuable resource for the practice of sinus surgeon. Smith et al. [55] performed a review of the literature regarding image guidance surgery. They noted that, due to the low number of major complications, a controlled trial would have to involve thousands of patients to attain sufficient power. Additionally, they argue that given the availability of this technology—which may confer safety benefits—randomization of patients away from this technology is “not practical, ethical, or feasible.” They conclude that among authors, there is universal agreement that image guidance systems represent a tool that has the potential to assist ESS surgeons but is no substitute for intimate understanding of each patient’s anatomy.
Image-Guided Therapy
Intraoperative image guidance systems rely on a preoperative data set from either CT or MRI images, and it is this stagnant data set that is used throughout the procedure to navigate. Intraoperative imaging systems are being developed that provide data and images that can be used during the procedure, thus allowing the surgeon to monitor the surgical progress and identify any intraoperative concerns that may arise from the changing anatomy. Work has been done to explore both MR-based and CT-based intraoperative systems.
MRI-Based Systems
Fried et al. [56–58] were the first to explore this concept with an intraoperative MR-based system on a series of 12 patients undergoing uncomplicated procedures. The image plane was surgeon controlled, and the MRI updated images in as little as 14 s. The procedures were performed without any complications and provided optimum feedback to the surgeon during the performance. While the initial evaluation of the system was positive, extremely high costs and implementation constraints made routine use impossible. Another constraint to routine use of such a system was the need for system-specific instrumentation [59]; this included metallic instruments and anesthesia devices that would function in a high magnetic environment. Suzuki et al. [60] evaluated the effectiveness of magnetic resonance image (MRI) guidance using an optical tracking system. Fourteen patients, 11 of whom presented with mucocele, were operated on using the real-time MR-based system. The prognosis of the patients was favorable, with no patients showing signs of recurrence of disease; however, they reported an additional 54 min of setup time for patients requiring general anesthesia and 17 min of additional setup time for patients requiring local anesthesia. Anand et al. [61] used real-time MRI in endoscopic pituitary resection, finding that the image quality was sufficient to identify residual tumor in 3 of 10 cases while encountering no complications.
CT-Based Systems
CT-based intraoperative systems are easier to implement practically than MR-based systems, are more appealing to the otolaryngologist because they enable superior visualization of bony structures, and cost significantly less. However, unlike MR-based systems, CT-based systems come with the inherent increase in radiation exposure to the patient.
Rafferty et al. [62, 63] developed a cone-beam CT imaging system and evaluated it on cadaver heads. The system generated intraoperative, volumetric CT images rapidly with an acceptably low radiation exposure to the patient and with image quality sufficient for most surgical tasks. They found that the system increased surgical confidence in accessing the frontal recess, resolved ambiguities with anatomical variations, and provided valuable teaching information to surgeons in training in both preoperative planning and correlation between triplanar CT scans and intraoperative endoscopic findings. Brown et al. [64] demonstrated the feasibility of real-time image guidance surgery using fluoroscopic images, and Manarey et al. [65] verified the safety of the same product by performing radiation dosimetry studies; however, the images produced by this product were deemed inadequate for routine use.
A study by Wise et al. looking at the use of CT-based intraoperative guidance systems has shown that inexperienced surgeons were far more comfortable identifying anatomic structures with IGS with intraoperative CT than they were with IGS with preoperative CT or endoscopy alone [66]. Jackman et al. [67] found that intraoperative acquisition of CT images led to alteration of surgical plan in 30 % of cases. While these systems are not currently routinely used due to high costs and unperfected technology, these studies show that the idea of intraoperative real-time image guidance is clearly the wave of the future for sinus surgeons.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree