Fig. 24.1
Pars interarticularis and pedicle stress reaction. Coronal fat-suppressed T2-weighted (a) and sagittal STIR (b) MRI demonstrate edema (arrow) in the left pedicle extending into the pars interarticularis of L5 consistent with a severe stress reaction
Fig. 24.2
Pars interarticularis stress fracture. Sagittal STIR (a) and T1-weighted (b) MRI demonstrate edema in the pars interarticularis (a, arrow) with clearly defined fracture line (double arrow). Oftentimes, the fracture line is more apparent on a CT scan (c, arrow)
Fig. 24.3
Spondylolisthesis. Sagittal STIR MRI (a, b) and sagittal reformatted CT image (c, d) demonstrate bilateral chronic pars fractures (arrow). Midline images from both studies demonstrate grade I anterolisthesis of L5 on S1 (e, f)
There does not appear to be a greater risk of lumbar disk degeneration when compared to controls (Capel et al. 2009). In men, lifting places significant stresses on the lumbosacral spine with a full press resulting in significantly higher compression forces than an arabesque lift (Alderson et al. 2009). Whether this results in an increased incidence of lumbar disk herniations in men is unclear.
Finally, the increased stresses in the lumbosacral region may be absorbed by or centered on the sacrum. As a result, although not common, stress fractures of the sacrum can occur in ballet dancers. Anecdotal experience indicates that they may be more common in female dancers. For this reason when a dancer with complaints of lower back pain is referred for a lumbar spine MRI, it is advisable to include at least one sequence that covers the sacrum to avoid missing a sacral stress fracture (Fig. 24.4).
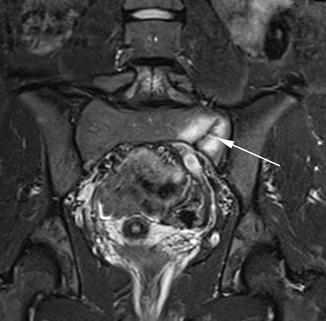
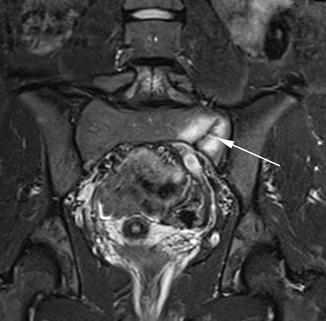
Fig. 24.4
Sacral stress fracture. Coronal STIR MRI demonstrates a left-sided sacral stress fracture with surrounding edema (arrow)
24.4 Appendicular Skeleton
24.4.1 Pelvis and Hips
The pelvis and hips play a central role in the execution of many of the movements in ballet. The degree of range of motion required, particularly at the hips, is beyond what is normal in the vast majority of the population. Although genetic factors play a role in the configuration and flexibility of the hips, there is evidence that training from a young age modifies the configuration, particularly of the femur. For instance, it has been shown that intensive ballet dancing between the ages of 11–14 can result in increased femoral retrotorsion (Hamilton et al. 2006), a configuration which allows a greater degree of external rotation and thus greater turnout. Although this increase in range of motion is adaptive and enables the dancers to achieve and maintain certain positions, moving the hips through the extremes of ranges of motion can place additional stress on surrounding structures. Although classical cam and pincer femoroacetabular impingement are uncommon in ballet dancers, some will have impingement despite normal underlying osseous anatomy. As the hips are moved through the extremes of ranges of motion, the femoral head and acetabulum may come in contact thereby affecting soft tissue structures. One of the more common problems is that of a posterior or posterosuperior acetabular labral tear in the absence of any cam lesion or acetabular retroversion/overcoverage (Fig. 24.5).
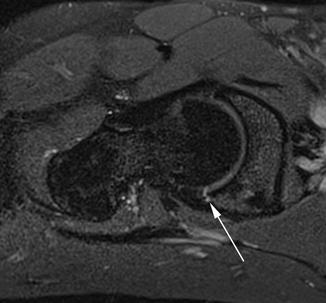
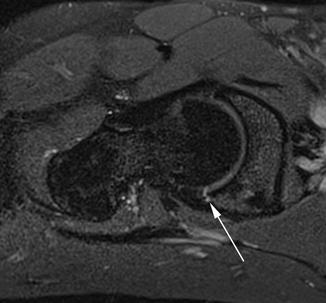
Fig. 24.5
Posterior acetabular labral tear. Oblique fat-suppressed proton density-weighted MRI demonstrates a posterior acetabular labral tear (arrow)
An even more common hip complaint in ballet dancers is that of a snapping hip. It has been reported that over 90 % of ballet dancers experience a snapping hip and that it can be reproduced almost at will in the majority of those dancers. The vast majority have bilateral snapping. Of those with a snapping hip, just over half have associated pain but less than 10 % have had to take time off due to this pain. Using ultrasound, it has been demonstrated that 59 % of the cases were caused by a snapping iliopsoas tendon, whereas only 4 % were due to the iliotibial band. In a third of the cases, the cause of snapping was not evident on ultrasound (Winston et al. 2007). As ultrasound is a dynamic entity, it is the modality of choice in evaluating such symptoms as it can elegantly demonstrate snapping when the iliopsoas tendon passes over the iliopsoas muscle belly with abduction and external rotation and then snaps back to its original position against the bone at the level of the iliopectineal eminence/superior pubic ramus, as the hip is brought back into anatomical position (Fig. 24.6) (Deslandes et al. 2008). On MRI, in the appropriate clinical setting, edema along the iliopsoas as it passes over the pelvic rim can suggest this diagnosis as well (Fig. 24.7). In addition, MRI can demonstrate the typical edema and fluid between the iliotibial band and the greater trochanter associated with iliotibial band snapping (Fig. 24.8).

Fig. 24.6
Snapping iliopsoas. Static transverse dynamic ultrasound images shows the iliopsoas tendon (T) is positioned anteromedial to the muscle (Musc) with the hip in flexion, abduction, and external rotation (a). As the hip is moved into extension (b), the tendon moves posteriorly and comes into contact with the superior pubic ramus or acetabular rim. In some dancers this movement results in an audible snap as the tendon moves from its intramuscular position to its posterior position (Images courtesy of Dr. Lionel Pesquer, Bordeaux, France)
Fig. 24.7
Snapping iliopsoas. Axial STIR (a) and oblique fat-suppressed proton density-weighted (b) MRI demonstrate the psoas tendon (arrow) and adjacent edema (double arrows) at the level where the iliopsoas tendon crosses the iliopectineal eminence and anterior acetabular rim

Fig. 24.8
Iliotibial band snapping. Coronal STIR MRI demonstrates edema (arrow) under the iliotibial band related to friction and snapping at the level of the greater trochanter
Of course, as in the spine and sacrum, the repetitive forces applied to the hips and pelvis can result in stress injuries of the pelvic ring and femoral necks. Ideally, these are identified while they are merely stress reactions. However, due to the nature of ballet and hesitation in seeking medical consultation for fear of losing one’s place in the company, many of these lesions are stress fractures at the time of imaging (Fig. 24.9).
Fig. 24.9
Stress fractures. Three different dancers with stress fractures of the femoral neck on coronal T1-weighted (a), junction of the acetabulum and superior pubic ramus (b), and inferior pubic ramus (c) on axial fat-suppressed T2-weighed MRI
One last condition to consider, particular in skeletally immature dancers, is stress lesions along the apophyses in the pelvis. Apophysitis, micro-avulsions, and complete apophyseal avulsions can be seen at various sites, particularly along the iliac crest, anterior superior and anterior inferior iliac spines, ischial tuberosities, and the lesser trochanter (Fig. 24.10). For this reason, it is crucial for the radiologist to be familiar with the tendinous origins and insertions about the hip to make an accurate and confident diagnosis of an avulsion injury.
Fig. 24.10
Apophyseal injury. Coronal T1-weighted (a) and STIR (b) MRI demonstrate an avulsion of the right iliac crest apophysis (arrow)
Muscle strains, particularly of the adductors, are common in ballet dancers and can present with either acute or chronic symptoms. It should be noted that strains may present with nonspecific, poorly localized, and/or referred pain. For this reason, it is crucial to image the entire pelvis making sure that the symphysis pubis, iliac crests, sacrum, and ischial tuberosities are within the field of view on at least one fluid-sensitive sequence. Muscle strains are often mild and do not require imaging. However, in more severe or persistent cases, MRI is the modality of choice to clearly identify the location and severity of injury as well as to exclude other lesions that may mimic muscular strains (Fig. 24.11).
Fig. 24.11
Groin strains. Coronal (a) and axial STIR (b) MRI demonstrate a mild strain of the right obturator externus (arrow). In another dancer, coronal STIR MRI (c) demonstrates an avulsion of the left common adductor tendon (arrow)
24.4.2 Knees
The knees of dancers undergo repetitive stresses in the form of axial loads, shear forces, and rotational forces. In addition, the knees go through a significant range of motion such as deep flexion with significant external rotation of the hips. Given these complex biomechanics, the knees of ballet dancers are susceptible to a variety of lesions involving the menisci, cruciates, collaterals, and the extensor mechanism.
The meniscal tears and the sprains and tears of the anterior cruciate ligament seen in ballet dancers are not significantly different from those seen in other athletes. As such, they will not be discussed further in this chapter.
On the other hand, anterior knee pain is quite common in ballet dancers; it is important to accurately diagnose the exact cause of the anterior knee pain in order to direct therapy and rehabilitation.
There are many types of anterior knee pain, among which the most common are tendinopathy (quadriceps or patella), patellofemoral maltracking, plica syndromes, and chondromalacia.
Tendinopathy of the quadriceps and/or patellar tendon is common in dancers and can be a source of chronic or recurrent pain. In skeletally immature dancers, the apophyseal insertion of the distal patellar tendon is a weak point and can result in “apophysitis” of the tibial tubercle. Clinically, this manifests as focal tenderness along the tibial tuberosity, also known as Osgood-Schlatter disease. Depending on the stage and severity, the imaging findings can range from minimal edema at the apophysis and synchondrosis to fragmentation and avulsion of the tibial tubercle apophysis. MRI can elegantly demonstrate the exact location and severity of the pathology (Fig. 24.12).
Fig. 24.12
Osgood-Schlatter disease. Sagittal proton density-weighted MRI without (a) and with (b) fat suppression demonstrate fragmentation and edema at the level of the apophysis of the tibial tubercle
Another common location of symptoms is along the inferior pole of the patella at the attachment site of the proximal patellar tendon. At this site, one can encounter tendinopathy and tendonitis, also referred to as jumper’s knee. In addition, in skeletally immature dancers, one may encounter a patellar sleeve avulsion. This refers to an avulsion of the periosteal sleeve of the inferior margin of the patella. Alternatively, with more chronic and recurrent injuries, one may get mild ossification or fragmentation and edema along the inferior pole of the patella, also known as Sinding-Larsen-Johansson disease. Some consider this as merely the pediatric version of jumper’s knee (Fig. 24.13) (Dupuis et al. 2009).
Fig. 24.13
Sinding-Larsen-Johansson syndrome. Sagittal proton density-weighted MRI without (a) and with (b) fat suppression demonstrate fragmentation and edema along the lower pole of the patella
Patellofemoral maltracking refers to abnormal tracking of the patella within the trochlear groove as the knee goes through flexion and extension. Although there may be underlying anatomical causes for such maltracking, such as trochlear dysplasia, oftentimes this form of maltracking in dancers is a result of tightness of the iliotibial band and/or weakness of the vastus medialis obliquus muscle (Reid et al. 1987). Both of these entities predispose the patella to move laterally and thus track asymmetrically within the trochlear groove. This can result in two common conditions. The first of these is patellar tendon lateral femoral condyle friction syndrome. As the name implies, the lateral tracking of the patella results in abnormal contact and friction between the patellar tendon and the lateral femoral condyle. This entity is easily and accurately diagnosed with MRI which demonstrates edema in the fat interposed between the proximal patellar tendon and the anterolateral margin of the lateral femoral condyle (Fig. 24.14). The second common condition associated with such maltracking is chondromalacia along the lateral facet of the patella and along the lateral portion of the trochlea. Again, MRI can elegantly demonstrate the exact location and grade of the cartilage damage in such cases (Fig. 24.15).
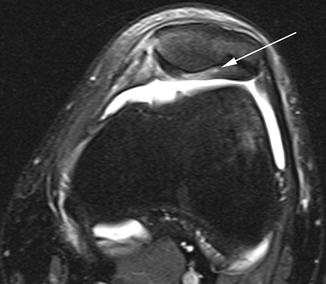
Fig. 24.14
Patellar tendon lateral femoral condyle friction. Axial (a) and sagittal (b) fat-suppressed intermediate-weighted MRI demonstrate edema (arrow) between the patellar tendon and the lateral femoral condyle due to friction
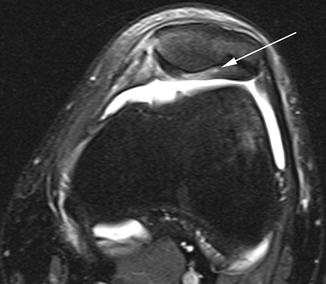
Fig. 24.15
Patellar chondromalacia. Axial fat-suppressed intermediate-weighted MRI demonstrates delamination of the cartilage of the patellar apex (arrow)
Finally, although somewhat controversial, some dancers complain of clicking or locking of the anterior knee as a result of entrapment of the medial plica of the knee between the patella and the medial femoral condyle. The imaging diagnosis of this entity is confounded by the fact that there may be no clear relationship between the imaging appearance of the medial plica and symptoms. However, in general, if on imaging one sees a prominent medial plica or plical shelf and it is associated with edema, one can suggest that the medial plica syndrome is a possible cause of the dancer’s anterior knee symptoms (Fig. 24.16).
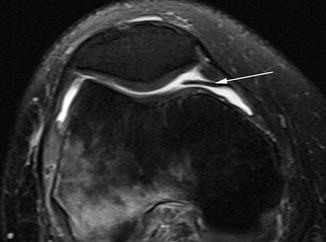
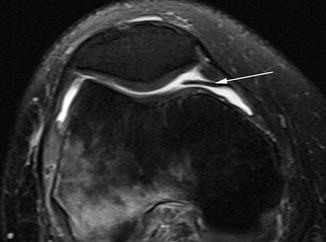
Fig. 24.16




Medial plical shelf. Axial fat-suppressed intermediate-weighted MRI demonstrates a prominent medial plical shelf interposed between the femur and patella (arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree