Fig. 12.1
Diagram illustrating the 6 phases of the throwing motion. The central highlighted area indicates the late cocking and acceleration phases during which maximal forces occur in the shoulder and elbow
As the arm is abducted and externally rotated, the humeral head experiences an anterior translational force on the glenoid that can equal half of the player’s body weight (Wilk et al. 2009). This is resisted by static stabilizers that include the glenoid labrum, glenohumeral ligaments, and anterior joint capsule, as well as dynamic stabilization through the rotator cuff and other muscles of the shoulder girdle and chest wall (Park et al. 2002a; Altchek and Dines 1995).
During the acceleration phase, humeral torque may reach levels that are higher than the torsional strength of the humerus as demonstrated in cadaver studies (Sabick and Torry 2004). The arm is decelerated after ball release by contraction of the posterior shoulder musculature resulting in distraction forces at the joint that may equal body weight (Wilk et al. 2009; Park et al. 2002b).
A tremendous valgus force also occurs at the elbow during these same phases of throwing. This results in distractive forces along the ulnar aspect of the joint that place medial side structures under tensile stress. These include the ulnar collateral ligament, common flexor tendon, and ulnar nerve (Gaskin et al. 2009). Over time, as the medial stabilizers begin to fail, the radiocapitellar joint is subjected to lateral-side compressive forces, and the posteromedial joint experiences shear forces, particularly the humeral-olecranon articulation (Fig. 12.2). This is referred to as the “valgus overload syndrome” and produces characteristic injuries within the thrower’s elbow (O’Holleran and Altchek 2006; Cain et al. 2003; Chen et al. 2001).
Fig. 12.2
Forces on the elbow during throwing. (a) Frontal and (b) posterior views of the elbow demonstrate the valgus force acting upon the elbow during throwing (red arrow) resulting in tensile forces along the medial joint (yellow arrow), compressive forces on the lateral joint (light blue arrows), and shear forces across the posterior joint (green arrow). Purple band ulnar collateral ligament
12.3 Imaging
12.3.1 Radiography
Shoulder
A standard radiographic examination of the shoulder should include anterior-posterior (usually with internal and external rotation of the humerus), scapular Y (outlet), and axillary views. West Point and Stryker notch views may also be considered (Wilk et al. 2009; Altchek and Dines 1995; Heyworth and Williams 2009; Rizio and Uribe 2001).
Elbow
A minimum of anterior-posterior, lateral, and oblique views should be obtained. Some also advocate the axial view (AP with the elbow flexed) for evaluating the olecranon and posterior joint (Cain et al. 2003; Lynch et al. 2008; Schwartz and Al-Zahrani 1996). Valgus stress views can be obtained to assess for medial instability. Widening of the medial joint of greater than 3 mm has been said to indicate instability; however since normal throwers often exhibit some degree of laxity, stress views of the opposite elbow are often obtained for comparison, and a side-to-side difference of 1–3 mm suggests an unstable joint (Lynch et al. 2008; Nassab and Schickendantz 2006).
12.3.2 MRI
Shoulder
The patient is scanned in the supine position with the arm at the side using a surface coil. The upper arm should be externally rotated such that the bicipital groove is directed anteriorly (at 12 o’clock on an axial image). Images are obtained in the axial, oblique coronal, and oblique sagittal planes with the oblique sequences oriented relative to the plane of the supraspinatus muscle.
For a standard MRI examination of the shoulder, T1-weighted and/or proton density sequences and T2-weighted sequences are typically obtained. Proton density-weighted and T2-weighted images are usually acquired using a fat saturation technique. Gradient echo (T2*-weighted) images are useful for labral evaluation. The exact choice of scanning parameters will vary according to the MR system and operator’s preferences.
Many centers prefer to assess the throwing athlete’s shoulder with MR arthrography. Much has been written about the advantages of this technique compared with standard MRI of the shoulder, including its specific benefits in overhead athletes with suspected internal derangement. These include superior sensitivity and specificity for diagnosing the most common abnormalities in overhead athletes including superior labrum anterior to posterior (SLAP) lesions, other types of labral tears, and partial-thickness undersurface tears of the rotator cuff tendons (Magee 2009; Magee et al. 2004; Tuite 2003).
The joint is typically distended with 12–15 cc of a dilute gadolinium solution prior to scanning (1:200 dilution of gadolinium in sterile saline). This is considered an “off-label” use of gadolinium by the Food and Drug Administration in the United States. The ABER position, in which the arm is held in abduction and external rotation, has been advocated as a useful adjunct to MR arthrography in the overhead athlete given its ability to better demonstrate undersurface cuff tears and because it places the anterior labrocapsular stabilizing structures under tension (Tirman et al. 1994a; Cvitanic et al. 1997; Choi et al. 2001; Cochet et al. 2010; Jung et al. 2010; Ito et al. 2005; Roger et al. 1999).
Elbow
The patient is scanned in a supine position using a surface coil, with the elbow at the side. If necessary, the patient can lay prone with the elbow positioned above the head, nearer to the center of the bore of the magnet. Images are obtained in axial, coronal, and sagittal planes. Coronal images are proscribed parallel to a line connecting the humeral epicondyles on an axial image. Sagittal images are oriented perpendicular to that axis. T1-weighted and/or proton density sequences and T2-weighted sequences are typically obtained. Proton density and T2-weighted images are usually acquired with a fat saturation technique. The use of high-resolution scanning parameters is mandatory for obtaining maximal diagnostic information (Carrino et al. 2001).
As with the shoulder, injection of a dilute gadolinium solution (1:200 dilution in sterile saline) results in excellent joint distention and has been shown to be especially helpful in depicting subtle partial-thickness tears of the ulnar collateral ligament, evaluating the stability of osteochondral lesions of the capitellum, and in demonstrating intra-articular loose bodies (Ouellett et al. 2008).
12.3.3 Significance of Imaging Findings
Numerous studies have documented varying rates of MRI abnormalities in the dominant arms of asymptomatic throwers (Lesniak et al. 2013; Connor et al. 2003; Miniaci et al. 2002). In a recent study of the dominant shoulders in 21 professional pitchers, nearly 50 % of the subjects were found to have rotator cuff tears (partial and full thickness), with about the same number demonstrating SLAP lesion and tears of the anterior and posterior portions of the labrum as well. Similarly, in a separate group of 16 asymptomatic professional players, more than 80 % were found to have MRI abnormalities of the ulnar collateral ligament and evidence of posteromedial impingement in their dominant elbows (Kooima et al. 2004). This emphasizes the complementary nature of imaging and clinical assessment of these patients.
12.4 Overuse Injuries
Overuse injuries are extremely common in baseball players and most often involve the shoulder and elbow. Pitchers are at the greatest risk, and it has been estimated that 73–79 % of all baseball injuries are related to pitching, with most of these affecting the shoulder and elbow (Oyama et al. 2013). Younger, skeletally immature throwers are especially vulnerable.
12.4.1 Shoulder: Rotator Cuff
12.4.1.1 Internal Impingement
Also known as posterosuperior impingement, the term refers to abutment of the greater tuberosity of the humerus against the posterosuperior aspect of the glenoid as the arm is abducted and externally rotated. A portion of the rotator cuff (the posterior fibers of the supraspinatus and anterior fibers of the infraspinatus tendons) may be entrapped between the bones, often along with the posterosuperior portion of the labrum (Fig. 12.3) (Park et al. 2002a; Meister 2000; Heyworth and Williams 2009). This contact can be seen in normal, asymptomatic throwers but may become symptomatic and produce a constellation of typical injuries (Heyworth and Williams 2009).
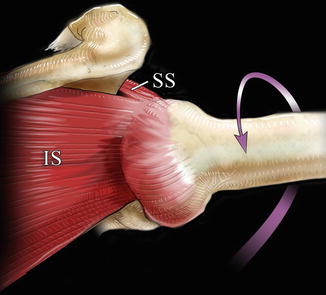
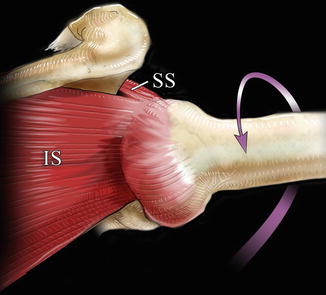
Fig. 12.3
Diagram illustrating internal impingement of the posterior cuff (posterior fibers of the supraspinatus (SS) and anterior fibers of the infraspinatus (IS) tendons) between the greater tuberosity and posterosuperior glenoid when the arm is abducted and externally rotated
Internal impingement has been thought to be secondary to microinstability that results from chronic stretching of the anterior capsular structures during the throwing motion (Heyworth and Williams 2009). Tightening of the posterior capsular tissues, also known as glenohumeral internal rotation deficit (GIRD), has also been implicated as a possible cause (Burkhart et al. 2003; Myers et al. 2006). This tightening leads to a loss of internal rotation, and, in an effort to maintain pitch velocity, the thrower develops an excessive degree of external rotation of the humerus. This excessive rotation leads to an anterior shift of the inferior glenohumeral ligament complex which then results in a posterosuperior shift of the axis of rotation of the humeral head on the glenoid, thereby worsening the osseous and soft tissue impingement along the posterosuperior aspect of the joint (Fig. 12.4).


Fig. 12.4
Diagram demonstrating the excessive external rotation (purple arrow) that occurs in throwers suffering from glenohumeral internal rotation deficit (GIRD). The result is an anterior shift of the inferior glenohumeral ligaments and axillary pouch (red ligaments in the upper drawing) relative to their normal inferior position (yellow). This shift produces a posterior/superior migration of the axis of the rotation of the humeral head relative to the glenoid (red circle) which is thought to contribute to the posterior superior labral and cuff pathology seen in the internal impingement syndrome
Associated injuries include superficial undersurface tears of the posterior cuff (posterior fibers of the supraspinatus, anterior fibers of the infraspinatus), fraying or tears of the posterior superior labrum, and subchondral cysts and/or sclerosis in the greater tuberosity or posterosuperior glenoid. Full-thickness rotator cuff tears are not common in this syndrome (Park et al. 2002a).
Radiographic findings that may be seen in patients with symptomatic internal impingement include sclerotic changes of the greater tuberosity, lytic “geodes” of the posterior humeral head, rounding of the posterior glenoid rim, and enthesopathy/exostosis of the posterior inferior glenoid rim (Bennett lesion) which is thought to be related to avulsive forces along the posterior capsule (Heyworth and Williams 2009).
The superficial undersurface cuff tears that occur with internal impingement are often very subtle and extremely difficult, if not impossible, to detect on MRI (Kaplan et al. 2004). MRI is the study of choice in these patients, and arthrography has been shown to be more sensitive than conventional MRI for detecting partial tears of the cuff (Fig. 12.5) (Magee et al. 2004; Tuite 2003). Scanning with the arm abducted and externally rotated (the “ABER” position) has also been advocated since it results in better separation of the cuff tendons from the humeral head, allowing improved visualization of the undersurface tears (Tuite 2003; Tirman et al. 1994b). Findings commonly associated with undersurface cuff tears include abnormalities of the posterior superior labrum and subchondral cystic foci in the greater tuberosity or superior glenoid. The presence of one or more of these imaging findings in an overhead athlete should suggest the diagnosis of internal impingement (Fig. 12.6) (Giaroli et al. 2005).
Fig. 12.5
An 18-year-old high school pitcher with history of glenohumeral internal rotation deficit (GIRD) and pain with throwing. (a) Sagittal fat-suppressed T2-weighted image from an MR arthrogram reveals a small partial-thickness undersurface tear in the infraspinatus tendon (arrow). Ant anterior. (b) Axial fat-suppressed T2-weighted MRI demonstrates tearing of the posterior superior labrum (arrow)
Fig. 12.6
A 46-year-old man with a long history of playing baseball (primarily pitching) presented with shoulder pain when throwing. (a) Coronal and (b) sagittal fat-suppressed T2-weighted images from an MR arthrogram reveal a small partial-thickness undersurface tear involving the posterior fibers of the supraspinatus tendon (arrows) as a consequence of internal impingement. Ant anterior. (c) Axial T1-weighted MR arthrogram shows tearing of the posterosuperior labrum (arrow)
12.4.1.2 External Impingement
Impingement of the supraspinatus tendon at the level of the coracoacromial arch (“outlet” of the shoulder) may be secondary to spurring along the anterior acromion or distal clavicle, a “hooklike” acromion, lateral downsloping of the acromion, or a thickened coracoacromial ligament. This type of impingement is the most common cause of cuff pathology in older patients, and while it may occur in older overhead athletes, it is rare in young throwers (Park et al. 2002a; Tuite 2003; Ouellette et al. 2008). The spectrum of cuff pathology ranges from tendinopathy to partial- or full-thickness tears.
Anatomic features that may lead to the development of impingement symptoms such as acromioclavicular joint spurring or abnormal acromial morphology may be evident on radiographs. These features are best demonstrated on MRI examinations in the oblique sagittal and oblique coronal planes (Fig. 12.7). Supraspinatus tendinopathy manifests as thickening of the tendon with diffuse, heterogeneous intrasubstance signal intensity on T1- and T2-weighted images. A partial-thickness tear is diagnosed when focal, fluid-equivalent signal intensity is identified along the articular or bursal surface of the tendon (Fig. 12.8). Fluid-equivalent signal intensity confined to the substance of the tendon indicates an interstitial tear. A full-thickness tear demonstrates fluid (or contrast) extending across the tendon. It is important to assess the dimensions of the tear, the degree of tendon retraction, and any associated atrophy within the muscles involved.
Fig. 12.7
A 42-year-old former baseball player with external impingement of the shoulder. The patient injured his arm while playing 12 years previously and recently developed increasing pain in that shoulder. (a) Oblique sagittal T1-weighted image from an MR arthrogram shows marked degeneration and hypertrophy of the acromioclavicular joint which slightly deforms the underlying supraspinatus tendon (arrow). A anterior acromion, C distal clavicle. (b) Oblique sagittal fat-suppressed T2-weighted MRI demonstrates a partial-thickness tear of the anterior fibers of the supraspinatus tendon (arrows). Ant anterior
Fig. 12.8
A 52-year-old man with external impingement of the shoulder. The patient has a long history of pitching and who now plays in an adult league presented with pain during throwing. (a) Oblique coronal and (b) oblique sagittal fat-suppressed T2-weighted images from an MR arthrogram demonstrate prominent partial-thickness undersurface tearing of the anterior fibers of the supraspinatus tendon (arrows). Ant anterior
12.4.1.3 Tensile Failure (“Rim-Rent”/“PASTA” Tears)
During the deceleration phase of the throwing motion, the muscles of the rotator cuff contract to slow the arm and, in so doing, place the cuff tendons under tension. These tensile forces can result in superficial undersurface tears involving the distal supraspinatus and infraspinatus tendons (Wilk et al. 2009; McConville and Iannotti 1999; Vinson et al. 2007). These lesions are known as “rim-rent” or “PASTA” (partial articular surface tendon avulsion) tears (Tuite et al. 1998) and are diagnosed on MRI when foci of fluid-equivalent signal intensity are noted on T2-weighted images along the undersurface of the distal supraspinatus and/or infraspinatus tendons very near their insertions (Fig. 12.9) (Vinson et al. 2007; Tuite et al. 1998; Ostlere and Marmery 2007). In some cases, retracted fibers can be identified along the undersurface of the tendon just proximal to the tear. These tears, however, can be very difficult to detect, especially if the arm is internally rotated (Vinson et al. 2007), and MR arthrography and scanning in the ABER position have been advocated for improved detection (Tirman et al. 1994b).
Fig. 12.9
Rim-rent tear. (a) Oblique coronal and (b) oblique sagittal fat-suppressed T2-weighted images from an MR arthrogram display a slit-like undersurface tear of the anterior fibers of the supraspinatus tendon (arrows) also known as a “rim-rent” tear. Ant anterior
12.4.1.4 Subscapularis Tendon
Injuries of the subscapularis tendon are much less common in the throwing athlete than are those involving the supraspinatus and infraspinatus tendons. Impingement of the undersurface of the subscapularis tendon against the anterior superior glenoid with flexion and internal rotation of the arm has been suggested as a cause of undersurface tears of the tendon in overhead athletes (Gerber and Sebesta 2000). Partial disruption of the distal fibers of the subscapularis allows for subluxation or dislocation of the long head of the biceps tendon from the bicipital groove and may be a source of anterior shoulder symptoms (Braun et al. 2009).
The subscapularis tendon is best evaluated on axial MRI as it courses anterior to the joint to insert on the lesser tuberosity. Tears of the distal subscapularis tendon may be quite subtle and only noticed because of associated medial subluxation of the biceps tendon (Fig. 12.10).
Fig. 12.10
A 47-year-old former pitcher with subscapularis tear with biceps subluxation, presented with a long history of shoulder pain that had worsened over the last 4–6 months. (a) Axial T1-weighted image from an MR arthrogram reveals a split tear of the distal subscapularis tendon (yellow arrow) with associated medial subluxation of the long head of the biceps tendon out of the bicipital groove (black arrow). Note also the posterior labral tear (white arrow). (b) Oblique coronal fat-suppressed T1-weighted image from an MR arthrogram shows additional severe tendinosis and partial tearing of the proximal biceps tendon within the joint (arrows)
12.4.2 Shoulder: Latissimus Dorsi and Teres Major
Although not a part of the rotator cuff complex, the latissimus dorsi plays an important and powerful role during the acceleration phase of throwing and is also active during the follow-through phase. The role of the teres major muscle in the throwing mechanism has not been delineated, but given its similar architecture and actions to the latissimus, these 2 muscles likely act synergistically during throwing. Injuries to these muscles are uncommon but have been seen in pitchers, with reports of both tendon avulsions and muscle strains (Fig. 12.11). Treatment is typically conservative with a long recovery period, but in the largest cohort to date, 15 of 16 affected pitchers were able to return to the same or higher level of play (Nagda et al. 2011).
Fig. 12.11
A 18-year-old active college pitcher with latissimus dorsi/teres major tears. The patient experienced significant shoulder pain during a recent drill. (a) Oblique coronal fat-suppressed T2-weighted image from an MR arthrogram reveals tearing of the latissimus dorsi and teres major tendons from their humeral attachment (black arrow) with some retraction of the muscle fibers (white arrow). (b) Axial fat-suppressed T2-weighted MRI confirms a complete tear with portions of the torn tendons still attached to the humerus (white arrows). Note the intact pectoralis tendon anteriorly (black arrow). (c) Oblique sagittal fat-suppressed T2-weighted MRI again shows the torn and retracted musculature with associated edema and fluid (white arrows) subjacent to the neurovascular structures within the quadrilateral space (black arrows). L/T latissimus/teres major muscle mass
12.4.3 Shoulder: Biceps Tendon
The long head of the biceps tendon assists with anterior stability during the late cocking phase by limiting anterior translation of the humeral head. It is subjected to stretching and traction forces, especially in the setting of anterior instability, in which case it has been found to be a more important stabilizer than the rotator cuff muscles (Park et al. 2002a). Pathology of the biceps tendon ranges from tendinopathy to partial or complete tears.
The vertical portion of the biceps tendon is best assessed on axial MRI as it courses within the bicipital groove. The horizontal portion of the tendon courses over the humeral head and is more difficult to evaluate, especially on non-arthrographic studies. It is best evaluated in the oblique sagittal and oblique coronal planes. Accurate assessment of the tendon is especially challenging where it curves to enter the bicipital groove since it is not orthogonal to the standard imaging planes and is susceptible to magic angle artifact at that site. Careful analysis of the few slices that cover that portion of the tendon should be performed in all 3 planes.
Biceps pathology can range from tendinopathy (an enlarged tendon displaying heterogeneous signal intensity) to partial or complete tears (Fig. 12.10). Focal pathology of the tendon at a level just proximal to the upper bicipital groove, described as a “groove entrance” lesion, is especially difficult to detect because of the curving morphology of the tendon at that site (Gaskin et al. 2009).
12.4.4 Shoulder: Labrum
12.4.4.1 SLAP Tear
Injuries to the superior labrum at the biceps-labral anchor (superior labrum anterior to posterior – “SLAP” – tears) are common in throwers. Chronic traction on the long head of the biceps tendon, primarily during the deceleration phase, has been implicated as a causative factor (Park et al. 2002b). SLAP tears in throwers may also result from a “peel-back” phenomenon in which the tendon assumes a more vertical and posterior orientation with abduction and external rotation of the arm. Simultaneous twisting of the tendon at its labral attachment acts to separate the posterosuperior labrum from the glenoid just posterior to the biceps-labral anchor (Fig. 12.12) (Park et al. 2002b; Bedi and Allen 2008).
Fig. 12.12
SLAP peel-back diagram. (a) Diagram demonstrating the biceps tendon (arrowhead) attaching to the biceps-labral anchor (arrow). H humeral head, G glenoid. (b) With external rotation of the humerus, the tendon twists (arrowhead) resulting in a “peel-back” tear of the superior labrum (SLAP tear) at its glenoid attachment (arrow)
Injuries of the superior labrum are best demonstrated on MRI in the oblique coronal plane. Fluid or contrast, extending between the labrum and superior glenoid, is diagnostic, although it can be difficult, if not impossible, to distinguish a true SLAP tear from a normal sublabral sulcus that occurs in that same region (Waldt et al. 2006; Tuite et al. 2005). Helpful MRI findings that support the diagnosis of a true SLAP tear include lateral extension of abnormal signal intensity into the substance of the labrum, irregularity of the labral margin, and extension of the signal into the proximal biceps tendon (Fig. 12.13) (Jin et al. 2006; Tuite et al. 2000). Scanning the patient in the ABER position has also been recommended in an attempt to provide a semi-dynamic assessment of stability of the biceps-labral anchor (Borrero et al. 2010).
Fig. 12.13
A 17-year-old baseball player with a SLAP tear, presenting with pain during throwing. (a, b) Oblique coronal fat-suppressed T1-weighted images from an MR arthrogram reveal an irregular tear of the superior labrum at the biceps-labral anchor (arrow). Note how the abnormal signal intensity extends laterally into the substance of the labrum in (b)
12.4.4.2 Posterior Superior Labrum (Internal Impingement)
As described above, impingement of the greater tuberosity of the humerus against the posterior superior glenoid is common in throwers and may become symptomatic. In addition to the superficial fraying and tears noted along the undersurface of the infraspinatus tendon, labral degeneration and tearing along the posterosuperior glenoid are also common associated findings (Kaplan et al. 2004). Other pathologic features include subchondral cysts in the posterior portion of the greater tuberosity, chondral abnormalities involving the humeral head, and subchondral cysts or sclerosis in the posterosuperior glenoid (Giaroli et al. 2005).
The posterosuperior labrum is best assessed on oblique coronal and axial images. An oblique axial scanning plane oriented perpendicular to the true long axis of the glenoid may provide a better assessment because it produces images more perpendicular to the oblique orientation of the labrum at this level. MR arthrography has also been advocated given its increased sensitivity for detecting labral pathology (Tuite 2003).
The labral findings in internal impingement may consist only of subtle fraying and irregularity of the posterosuperior labrum. Even so, the labral abnormalities may be more readily recognized on MRI than the associated superficial undersurface tears involving the posterior cuff tendons. High-signal subcortical marrow edema and cysts in the greater tuberosity or posterosuperior glenoid are most conspicuous on fat-saturated T2-weighted images and are also helpful secondary signs (Giaroli et al. 2005). Subchondral sclerosis, when present, is best identified on T1-weighted images since its low signal intensity contrasts sharply with the high signal intensity of the adjacent marrow fat.
12.4.4.3 Anterior/Posterior Labral Pathology
The anterior labrum and glenohumeral ligaments are placed under tension when the arm is abducted and externally rotated during the late cocking phase of the throwing motion. Over time the accumulation of microdamage in these structures may result in anterior instability (Park et al. 2002a). Similarly, during the deceleration phase, when the forward momentum of the arm is rapidly slowed by both eccentric posterior muscle contraction and static posterior labrocapsular structures, stretching of the posterior soft tissue restraints may result in posterior instability (Park et al. 2002b). Although frank labral avulsions are rare in throwers, other forms of anterior and/or posterior labral pathology may result.
Another potential source of posterior labral pathology occurs with the so-called “batter’s shoulder” in which there is transient posterior subluxation of the lead shoulder during the swing (Wanich et al. 2012). This uncommon injury is thought to be related to the posterior rotational forces that act upon that shoulder as the bat is accelerated through the swing. Patients present with posterior shoulder pain during batting, and most are found to have posterior labral tearing that often requires arthroscopic stabilization for the patient to be able to return to play (Wanich et al. 2012).
The anterior and posterior portions of the labrum are best evaluated on axial MRI. As with labral pathology at other sites, MR findings of a labral tear include abnormal signal within the labrum or interposed between the labrum and glenoid (Fig. 12.14). The morphology of the labrum can be quite variable, so a finding of labral “irregularity” is less specific. With posterior instability, the posterior joint recesses may appear capacious, but since that is a very subjective determination, a more specific finding is that of posterior capsular stripping along the posterior margin of the glenoid. In that region, the normal capsule attaches consistently along the base of the labrum at its junction with the osseous glenoid. Assessment of anterior capsular stripping is much more difficult because of the extreme variability of the normal capsular attachments along the anterior glenoid.
Fig. 12.14
A 17-year-old baseball player with posterior labral tear, presenting with shoulder pain that is aggravated with throwing. (a) Axial T1- and (b) fat-suppressed T2-weighted images from an MR arthrogram demonstrate posterior labral tearing (arrow, a) and associated posterior paralabral cysts (arrows, b)
12.4.5 Elbow: Medial
As described above, the valgus force that occurs at the elbow during the late cocking and acceleration phases of the throwing motion places the structures along the medial side of the joint under tension. This may result, over time, in attritional or stretch injuries to these tissues.
12.4.5.1 Ulnar Collateral Ligament
The ulnar collateral ligament (UCL) is composed of three bands: anterior, posterior, and transverse/oblique (Chen et al. 2001). The anterior band is the primary restraint against valgus force at the elbow during the throwing motion, while the posterior band plays a much less significant role. The transverse band plays no significant part in stabilizing the elbow (Chen et al. 2001; Lynch et al. 2008). Repetitive valgus stresses during throwing can cause the anterior band of the UCL to accumulate microdamage within its fibers leading to stretching and partial or complete tears of the ligament (Lynch et al. 2008).
The normal anterior band of the UCL is best seen on coronal and axial MRI as a low signal structure extending from the undersurface of the medial epicondyle to attach to the medial margin of the coronoid process of the ulna at the sublime tubercle. Its humeral attachment is relatively broad and often demonstrates slightly heterogeneous signal compared to the more distal fibers which taper toward their ulnar attachment. The anterior band is well demonstrated in cross section on axial images where the posterior band is also seen as a thin low signal structure forming the floor of the adjacent cubital tunnel.
Following ligamentous sprain, the anterior band appears somewhat thickened, typically with adjacent edema.
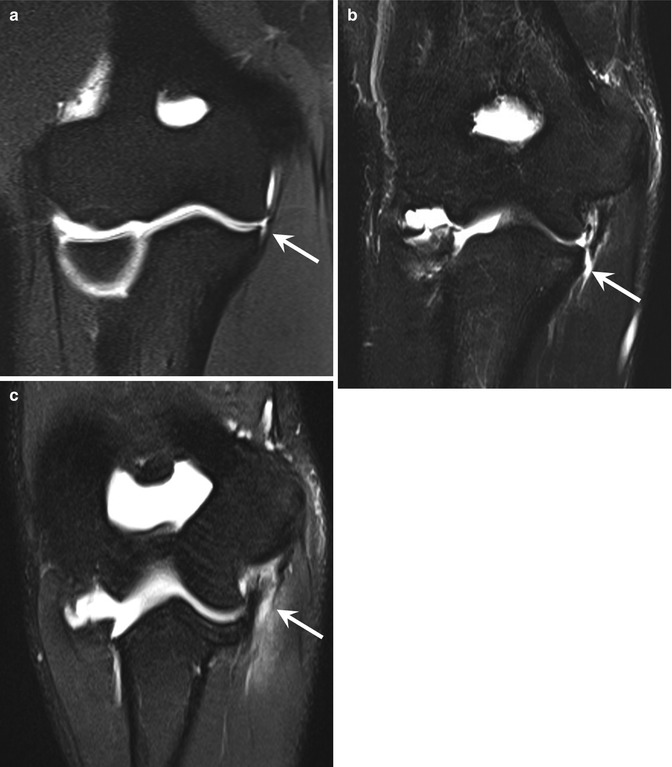
Partial tears may involve any portion of the ligament and result in some degree of fiber disruption. An especially subtle lesion involves partial stripping of the distal fibers at their ulnar attachment, often producing the “T” sign on routine or, more commonly, arthrographic MRI (Fig. 12.15) (Timmerman and Andrews 1994; Schwartz et al. 1995; Timmerman et al. 1994; Nakanishi et al. 1996). This may be difficult to differentiate from a reported normal variation of mild separation of the fibers from the sublime tubercle (Munshi et al. 2004); the distinction is usually based on the degree of separation of the ligament from the bone and the amount of fluid or contrast undercutting the ligament at that site. The normally heterogeneous signal within the proximal fibers of the ligament may be difficult to distinguish from a partial tear at its humeral attachment. A partial tear of the posterior bundle is much less common but may clinically mimic an anterior bundle injury. Such a tear is best demonstrated on axial images.