Fig. 18.1
Anteroposterior radiograph of the right clavicle (a) shows post-traumatic right non-displaced clavicular fracture in a professional rider (arrow). Anteroposterior (b) and lateral (c) radiographs in a second fall of the same professional rider on the same day show a secondary displaced clavicular fracture (arrows)
Fig. 18.2
Coronal gray-scale ultrasound images obtained at rest (a) and during stress (b) of the acromioclavicular joint show chronic instability of the joint. In (b) note the upward displacement (arrow) of the lateral end of the clavicle (clav). Acr acromion
Fig. 18.3
Coronal (a) and sagittal (b) color Doppler ultrasound images show bulging of the joint (arrows) associated with marked peripheral hypervascular changes (arrowheads) in an acute sprain of the acromioclavicular joint. Clav clavicle, Acr acromion
Fig. 18.4
Oblique coronal fat-suppressed proton density-weighted MRI shows hyperintense signal at the greater tuberosity reflecting post-traumatic edema (arrow)
18.3 Other Pathologies
18.3.1 Musculoskeletal Pathologies
Concerning musculoskeletal pathologies without acute trauma, the knee is the most frequently affected joint (Silberman 2013; Mellion 1991; Clarsen et al. 2010; Cosca and Navazio 2007; Maillot 2009). The clinician’s first reflex should be to ask about a recent change of equipment, not only the bicycle but also the outfit. Observing the cyclist during exercise on a home trainer is essential as this will often make it possible to identify inappropriate movement or equipment.
Pedaling is usually broken down into four phases (Fig. 18.5) (Maillot 2009; Nicolet and Jacob 2010):
Fig. 18.5
Drawing shows the pedaling phases. Phase 1: power phase from 20° to 145°. Phase 2: low transition from 145° to 215°. Phase 3: recovery/traction from 215° to 320°. Phase 4: high transition from 320° to 20°
Phase 1: Power phase from 20° to 145°
Phase 2: Low transition from 145° to 215°
Phase 3: Recovery/traction from 215° to 320°
Phase 4: High transition from 320° to 20°
During phase 1, there is active extension of the hip (45°), the knee (70°), and the foot (30°); the stabilizer muscles of the pelvis play an important role (quadratus lumborum, abdominal muscles).
During phase 2, there is plantar flexion of the ankle of 15° in which the hamstring muscles and the triceps surae play an essential role.
Phase 3 is the phase involving active flexion of the lower limb, with flexion of the hip of 35°, which brings into play the psoas, the sartorius, and the rectus abdominis muscles, and flexion of the knee of 55° which involves concentric hamstring contraction.
Phase 4 comprises brisk plantar flexion of the foot with low amplitudes at the hip and pelvis.
The knee is normally flexed at 10–15° when the pedal is at its lowest point and at 110–115° when it is at its highest point.
When pedaling, there is natural lateral rotation of the tibia estimated at a mean of 17° in extension; this rotation disappears at 30° of flexion.
Most tendinopathies are due to problems with pedaling.
18.3.1.1 Knee
During pedaling, the knee is subjected to repeated microtrauma: 100 km of cycling corresponds to 15,000–20,000 revolutions of the pedals (Maillot 2009).
18.3.1.2 Extensor Apparatus: Anterior Knee Pain (Patellofemoral Syndrome, Patellar Tendinopathy, Quadriceps Tendinopathy)
It is essential to look for incorrect positioning on the bicycle; it is often due to a saddle that is too low, a frame that is too short, cranks that are too long, or a position that is too far forward (Bini et al. 2011, 2014). In such cases, the cyclist is in a situation of knee hyperflexion. Pathologies of the extensor apparatus are often related to intense effort: the standing position, a sprint, or a cobblestone road.
Patellofemoral syndrome is frequent among cyclists (Silberman 2013; Cosca and Navazio 2007; Maillot 2009; Ericson and Nisell 1987). It appears as pain on pedaling. The pain may also occur when the person goes up- or downstairs and if the knee is bent for long periods, in the sitting position in particular (theater sign). The clinical examination sometimes reveals patellofemoral malalignment on contraction of the quadriceps, pain on palpation of the patellofemoral area, cracking with complete extension, and a positive J sign. It is important to make sure the saddle is not too high and look for excessive medial rotation of the foot or a gear ratio that is too high. As for imaging, standard radiography is essential: the axial view is useful to look for patellar and/or trochlear dysplasia and lateral subluxation of the patella. Nonetheless the x-ray examination is often normal. 3D fat-suppressed proton density-weighted and sagittal and axial T1-weighted MRI are used to visualize the cartilage in high-level athletes or in cases of persistent symptomatology (Fig. 18.6). Specific T2 mapping sequences can be used (Fig. 18.7). Arthrography with the intra-articular injection of an iodine contrast agent and 3D reconstruction is also very useful given the better spatial resolution. Management will involve studying the training program and checking the saddle height, the athlete’s position on the bicycle, and the foot-blocking system. Physiotherapy is often useful and in exceptional cases surgery may be necessary.
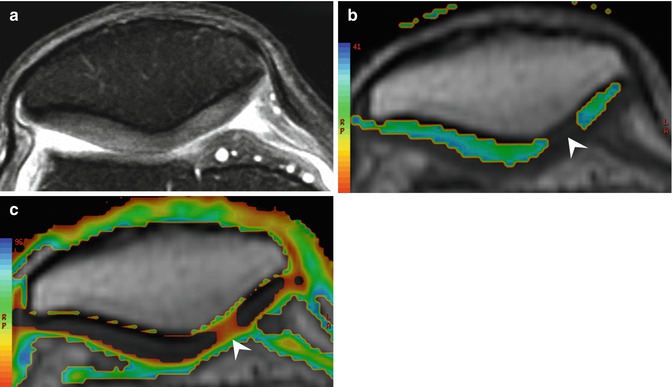
Fig. 18.6
Axial fat-suppressed proton density-weighted MRI of the knee shows cartilage defect (arrow) and loose body (arrowhead) consistent with patellar chondromalacia
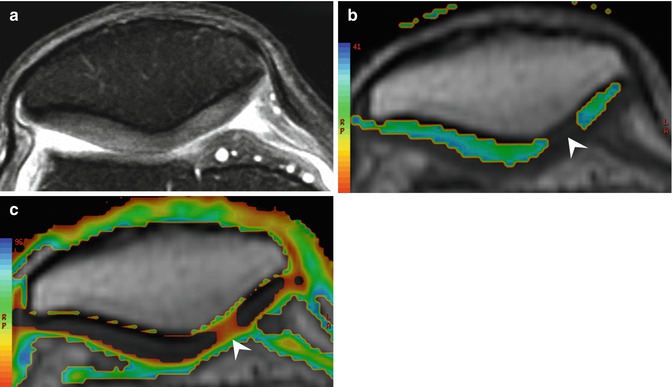
Fig. 18.7
Axial fat-suppressed proton density-weighted MRI of the knee (a) shows normal patellar cartilage. Axial T2 mapping (b, c) of the patellar cartilage at the same level detects early patellar cartilage chondromalacia (arrowheads)
Patellar tendinopathy concerns the proximal part of the patellar tendon. Repeated microtrauma and a long inferior patellar apex have been described as risk factors. This condition often occurs in sports that require contraction of the quadriceps and is referred to as “jumper’s knee” (Bianchi and Martinoli 2007).
Standard radiography is usually normal, though sometimes calcification can be seen at the insertion. The most helpful examination is high-resolution ultrasound, which can confirm the clinical diagnosis and show the extent and severity of the lesions (Bianchi and Martinoli 2007). Patellar tendinopathy is revealed by a hypoechoic aspect of the patellar tendon, typically in the deep and median portions. The central nodule explains why it is sometimes difficult to recognize these lesions on longitudinal views that are too lateral or too medial. Power Doppler is useful to show hyperemia, provided that the leg is straight so that the patellar tendon is relaxed (Figs. 18.8 and 18.9). If the leg is flexed during the examination, the hyperemia may not be visible with pulsed Doppler. Patellar tendons that have already been operated on retain a heterogeneous hypoechoic aspect, and in such cases, pulsed Doppler can be used to distinguish between active tendinopathy and the sequelae of earlier lesions. Ultrasound can also reveal partial ruptures, which are exceptional in cycling unless caused by direct trauma. It must be noted that in patients with a history of ligamentoplasty of the anterior cruciate ligament using the Kenneth-Jones technique, the tendon appears in the form of sagittal cords separated by a central hypoechoic band. There may also be a bone defect in the lower third of the patella and the tibial tuberosity.
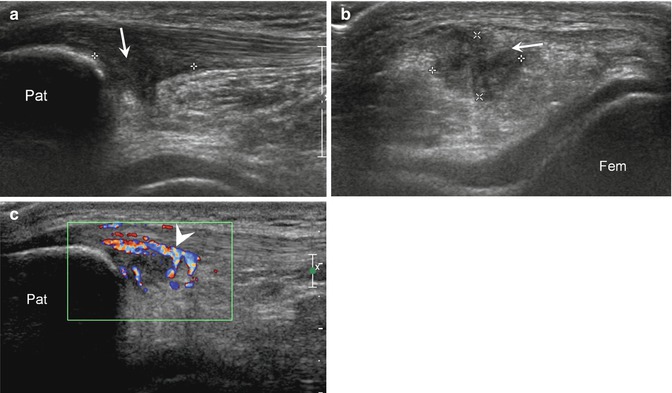
Fig. 18.8
Sagittal color Doppler ultrasound image (a) shows diffuse hyperemia (neovascularization) and proximal hypoechoic aspect of the proximal patellar tendon (arrow). Sagittal fat-suppressed proton density-weighted MRI (b) shows the corresponding hyperintensity signal at the proximal patellar tendon consistent with proximal patellar tendinitis
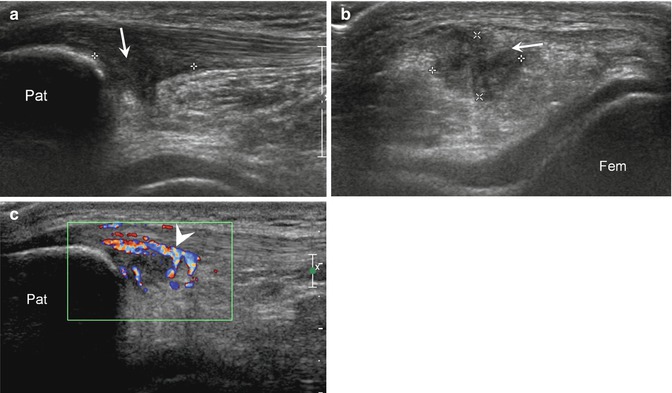
Fig. 18.9
Sagittal (a) and transverse (b) gray-scale and sagittal color Doppler ultrasound (c) images show a hypoechoic area of tendinopathy (arrows, calipers) located at the proximal part of the patellar tendon. Color Doppler shows local hyperemia (arrowhead) in keeping with proximal patellar tendinitis. Pat patella
Generally speaking, athletes and cyclists in particular are rarely affected by diffuse or distal tendinopathy (Bianchi and Martinoli 2007; Tuite 2010), though deep and superficial infrapatellar bursitis may be seen. MRI using sagittal T1-weighted and 3D fat-suppressed proton density-weighted imaging, associated with sequences with intravenous injection of gadolinium contrast agent, usually in the sagittal plane, will clearly show patellar tendinopathy. However, MRI is usually used only in cases when there are doubts about the diagnosis (Fig. 18.10). The treatment is based on rest, which should be complete or modulated depending on the sport practiced, and the duration must correspond to the severity of the lesions. Treatment with anti-inflammatory drugs for 4–6 weeks is useful and physicians must know how to use physiotherapy.
Fig. 18.10
Axial fat-suppressed proton density-weighted MRI of the knee shows the central hyperintense area within the tendon (arrow) consistent with proximal patellar central nodule tendinitis
Accidents causing tendon rupture are rare. It may occur in tendons inadvertently made fragile by intratendon sheath corticosteroid infusions (which as a general rule should be proscribed).
Physiotherapy (ultrasound, low-energy laser, radio frequency), mesotherapy, radial or focal shock waves, stretching, or low-speed and extremely submaximal eccentric exercise can be proposed. Steroid ultrasound-guided injections in the Hoffa fat pad are often helpful (Fig. 18.11). PRP (platelet-rich plasma) is an alternative in cases of intratendinous fissure. In rare cases, sclerotherapy or surgery may be necessary (Ferret 2010).
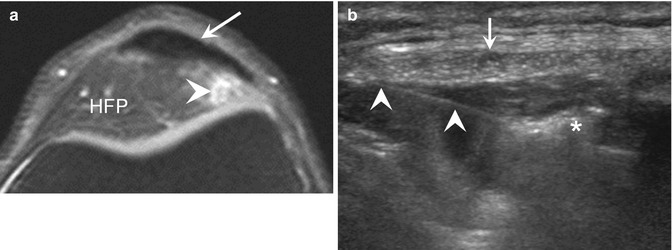
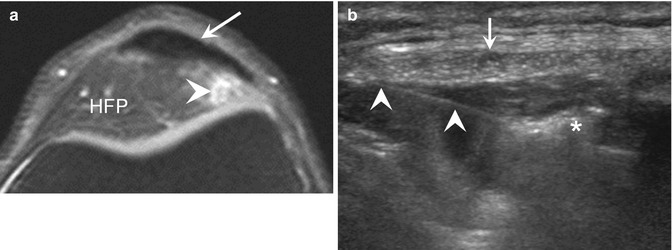
Fig. 18.11
Axial fat-suppressed proton density-weighted MRI of the knee (a) shows a hyperintense area (arrowhead) of the superolateral Hoffa fat pad (HFP) located between the patellar tendon (arrow) and the femur consistent with superolateral Hoffa impingement. Corresponding transverse ultrasound image (b) obtained during ultrasound-guided local injection shows the needle (white arrowheads) and the injected steroid-anesthetic mixture (asterisk)
Quadriceps tendinopathy is sometimes seen; it is less frequent than patellar tendinopathy (Bianchi and Martinoli 2007).
The clinical presentation consists of focal suprapatellar pain, corresponding to the distal portion of the tendon. The pain is exacerbated by extension of the knee against resistance. There is no intra-articular effusion. Standard radiography may show calcification at the insertion and thickening of the tendon. It will also show the relationships between the bones, notably the femur and patella. The examination of choice is ultrasound, which will confirm the diagnosis and indicate the severity of the lesions (Fig. 18.12). In the case of moderate disease, it will be possible to see a central or sagittal hypoechoic formation within the tendon. This will be clearly visible on axial and then sagittal slices. Doppler ultrasound will show hyperemia. More rarely, in cases with severe disease, the whole distal tendon is affected, with a globally hypoechoic aspect of the distal tendon, which has lost its distal fibrillar architecture and shows major diffuse hyperemia on Doppler ultrasound. If 6–12 months of medical treatment is ineffective, a presurgery ultrasound scan is necessary to map the pathological zones.
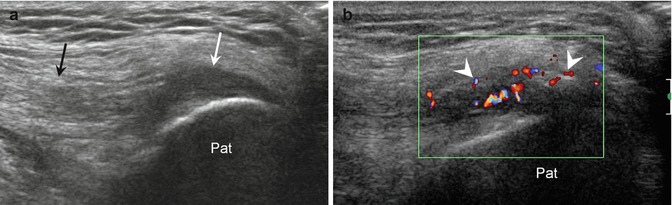
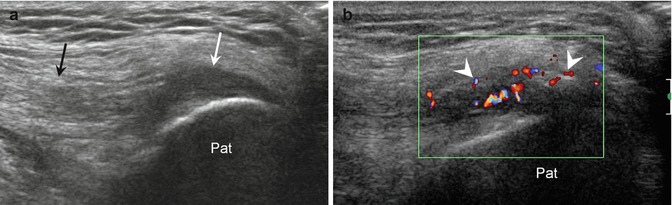
Fig. 18.12
Longitudinal gray-scale (a) and color Doppler (b) ultrasound images show hypoechoic appearance of the distal (white arrow) quadriceps tendon consistent with quadriceps tendinitis. The proximal tendon (black arrow) is normal. In (b) local hypervascular changes (arrowheads) due to neovascularization. Pat patella
MRI is also very useful in investigating quadriceps tendinopathy. T1-weighted, fat-suppressed proton density-weighted, and T1-weighted fat-suppressed contrast-enhanced MRI in the sagittal and axial planes can reveal lesions of the distal tendon, which show up as hypointense signals in T1- and hyperintense signals in T2-weighted fat-suppressed and T1-weighted fat-suppressed contrast-enhanced images. MRI shows the size and contours of the lesion and may reveal involvement of the cancellous interior of the patella and the existence of associated joint disease.
18.3.1.3 Iliotibial Band Syndrome
This is a frequent pathology among competition cyclists (Silberman 2013; Maillot 2009; Tuite 2010; Wanich et al. 2007; Deakon 2012; Spiker et al. 2012; Farrell et al. 2003). The band symptom, pain, is caused by excessive friction of the distal iliotibial band as it slides over the lateral femoral epicondyle, resulting in bursitis. The chronic pain is exacerbated by pedaling or running and occurs about 2 cm above the joint line. The Ober test is positive, with pain occurring on adduction of the hip and leg, with the knee fixed, the patient lying on the non-symptomatic side. In general, it is related to inappropriate saddle height (too high), incorrect adjustment of the pedals, or an inappropriate position on the bicycle. Careful examination of the cyclist in action will make it possible to correct these problems. The diagnosis is often clinical, but imaging can be useful (Maillot 2009). Standard radiography must always be done, even though it is usually normal. High-resolution ultrasound is the examination of choice as, in general, it reveals a fluid-filled bursa sac. Doppler ultrasound may show hyperemia, associated with thickening of the distal iliotibial band. Dynamic ultrasound involving flexion-extension of the knee causes pain and shows the contact between the inflamed tissue and the lateral femoral epicondyle. One advantage of ultrasound is that it can rule out lesions of the popliteus tendon or the femoral biceps tendon in difficult cases. Coronal 3D T1-weighted and fat-suppressed proton density-weighted MRI also show the bursitis as a hyperintensity and thickening of the distal iliotibial band. In severe forms, there is sometimes edema in the cancellous bone adjacent to the lateral femoral epicondyle (Figs. 18.13 and 18.14). Treatment is based on correction of the problems concerning the equipment or the position of the cyclist or the use of ice packs and nonsteroidal anti-inflammatory drugs. Physiotherapy may be proposed. In cases of persistent pain, injections of synthetic cortisone, preferably ultrasound-guided, often lead to rapid recovery (Fig. 18.15).

Fig. 18.13
Anteroposterior radiograph of the left knee (a) shows tibia vara. Axial fat-suppressed proton density-weighted MRI (b) shows a hyperintense area (arrowheads) located between the iliotibial band (arrow) and the femur in keeping with iliotibial band syndrome

Fig. 18.14
Coronal fat-suppressed proton density-weighted MRI of the right knee shows hyperintense area (arrow) between the iliotibial band (arrowheads) and lateral femoral epicondyle consistent with iliotibial band syndrome
Fig. 18.15
Coronal ultrasound image of the left knee (a) shows a hypoechoic thickening (arrowheads) of the soft tissues located between the iliotibial band (arrows) and the femur consistent with iliotibial band syndrome. Corresponding ultrasound images obtained during ultrasound-guided injection (b, c) show accurate local steroid injection. White arrowheads needle, asterisks injected steroid-anesthetic mixture. Fem femur
18.3.1.4 Pes Anserine Tendinitis
Clinically, there is pain in the area of the superomedial tibia, at the insertion of the pes anserine tendons; the pain often has a progressive onset. Make sure that the saddle is not too high, that the external rotation of the forefoot is not excessive, and that the pedal axis is not misaligned or worn on the underside. The muscles concerned are active in phase 3 (traction phase) of pedaling (Silberman 2013; Maillot 2009). Radiography is essential though generally normal. Ultrasound is the most revealing examination in the exploration of the pes anserine tendons: the tendons of the gracilis, the semitendinosus, and the sartorius muscles are clearly visible from the anteromedial aspect of the head of the tibia to about 5–6 cm above the femorotibial joint line. The inferior genicular artery is visible on Doppler ultrasound. Look for pain at the insertion of the pes anserine tendons, a hypoechoic aspect of the tendons, and in particular classical pes anserine bursitis. Ultrasound can also be used to make treatment safer by guiding injections to treat the bursitis. Of course, MRI can also show pes anserine tendinopathy, notably by hypersignals on fat-suppressed proton density-weighted and fat-suppressed T1-weighted contrast-enhanced images of the tendon sheaths, and, if present, the bursitis (Fig. 18.16). Coronal slices are essential, and it is necessary to make sure that the axial slices are sufficiently low to examine the insertions in detail. MRI can also reveal edema of the cancellous bone of the tibia and possible associated intra-articular disease.


Fig. 18.16
Coronal (a) and axial (b) fat-suppressed proton density-weighted MRI show focal medial hyperintense area located on the distal aspect of the pes anserine tendons (arrows) in keeping with pes anserine bursitis
18.3.1.5 Biceps Femoris Tendinopathy
There will be lateral pain on flexion of the knee against resistance, on stretching in extension, and on palpation of the fibula head. There is sometimes a “trigger” phenomenon of the distal biceps femoris tendon (Maillot 2009). Make sure that the pedal axis is not misaligned or worn on the topside and check for a short calcaneal tendon court, stiffness of the tibiotarsal region, and excessive medial rotation of the forefoot. Ultrasound, after an often normal standard radiography examination, will clearly show the insertion of the biceps femoris tendon at the fibula. As usual, investigation involving the axial and coronal planes is necessary. The myotendinous junction must be explored, since there may be possible disinsertion of the aponeuroses. On axial slices, it is possible to distinguish between the distal biceps femoris tendon and the lateral collateral ligament. It is also possible to see the common fibular nerve. One should look for a loss of the fibrous architecture, hypoechoic thickening, and hyperemia on Doppler ultrasound (Bianchi and Martinoli 2007). MRI is rarely necessary, although coronal T1-weighted and 3D fat-suppressed proton density-weighted sequences in the axial plane at a level that is sufficiently low enable exploration of the upper region of the fibula. It will reveal thickening of the enthesis of the biceps femoris, edema of the tendon and bone, and possible compressive structures of the proximal tibia-fibula joint line. Distal disinsertion of the aponeurosis, if present, will be clearly visible.
18.3.2 Other Tendinopathies
18.3.2.1 Achilles Tendinopathy
Achilles (or calcaneal) tendinopathy is also reported in both amateur and professional cyclists (Silberman 2013; Tuite 2010; Wanich et al. 2007; Deakon 2012). It is, however, less frequent than tendinopathies of the knee. The clinical examination will look for painful swelling of the calcaneal tendon and for possible tendon tear using the Thompson test. Standard radiography will reveal the morphology of the posterior calcaneal tuberosity (possible Haglund’s deformity) and rule out focal bone lesions. It will also show calcifications of the Achilles tendon. It will also be possible to assess swelling in the posterior soft tissues. Ultrasound is also particularly useful in examining the Achilles tendon to localize the tendinopathy, which may be fusiform (Fig. 18.17) or at the enthesis (Fig. 18.18). The Doppler ultrasound scan should be done in plantar flexion to show hyperemia, which is a key factor in the diagnosis, and areas of partial rupture should be sought. Ultrasound will also show the whole length of the plantar tendon, when present, and any possible abnormal aspects. It will also be easy to see an accessory muscle, if present (Bianchi and Martinoli 2007). In pathological areas, the Achilles tendon loses its usual echogenic fibrillar structure and becomes globally hypoechoic. Retrocalcaneal or retroachilles bursitis will be easily identifiable (Fig. 18.19), and ultrasound can be used to guide injections, though cortisone injections are not recommended in isolated Achilles tendinopathy because of the increased risk of tendon rupture. In cases of intratendinous tears, ultrasound-guided PRP injections are an alternative therapy. Certain teams use the sclerosing agent polidocanol, which is also injected into hyperemic areas under ultrasound guidance, to allow painless rehabilitation (Alfredson and Ohberg 2005; Montagnon et al. 2013). Axial and sagittal MRI in T1-weighted, fat-suppressed T2-weighted, and fat-suppressed T1-weighted contrast-enhanced sequences will clearly show thickening of the Achilles tendon, areas of partial rupture, and posterior retrocalcaneal bursitis. Any associated joint disease or posterior impingement syndrome will also be visible. MRI is done only in cases of chronic disease or in cases of discordant investigations.
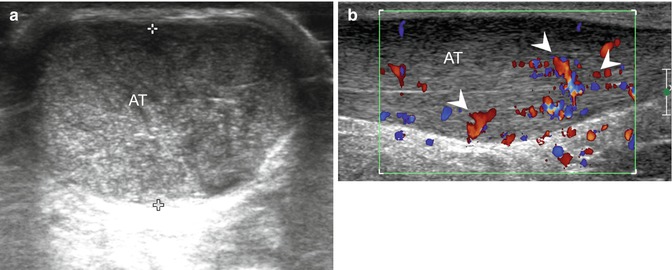
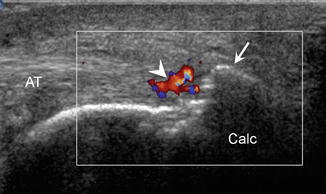
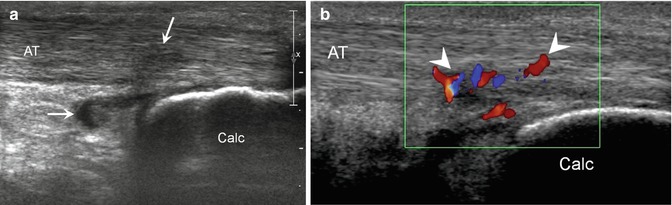
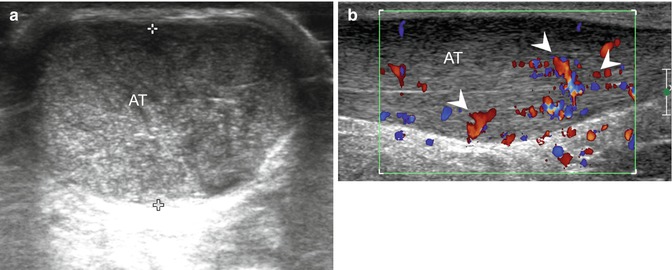
Fig. 18.17
Transverse gray-scale (a) and sagittal color Doppler (b) ultrasound images show a fusiform enlargement and hypoechoic appearance (black arrow) of the Achilles tendon (AT) consistent with tendinopathy of the Achilles tendon. Color Doppler ultrasound shows severe local neovascularization (arrowheads)
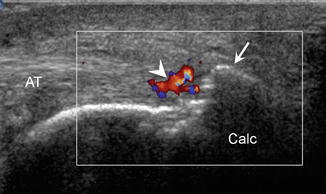
Fig. 18.18
Sagittal color Doppler ultrasound image shows focal hyperemia (arrowhead) and local calcification (arrow) of the enthesis of the Achilles tendon (AT) in keeping with enthesitis of the Achilles tendon
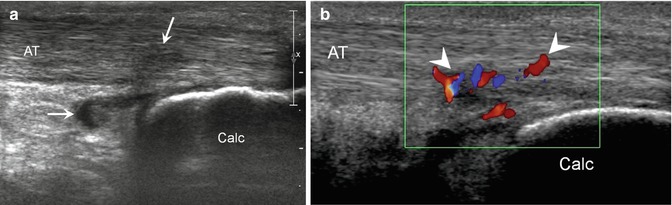
Fig. 18.19
Sagittal gray-scale (a) and color Doppler (b) ultrasound images show a focal hypoechoic appearance (black arrow) of the Achilles tendon (AT) as well as thickening (white arrow) of the retrocalcaneal synovial bursa consistent with distal tendinopathy of the Achilles tendon with retrocalcaneal bursitis. In (b) note local hyperemia (arrowheads)
18.3.2.2 Wrist Tendinopathy
These tendinopathies are rather rare in road cycling, and more often described in off-road cycling, but are sometimes reported in the former (Ferret 2010). The position of the hands on the handlebar must be assessed. On the dorsal aspect, tendinopathy may be seen in the extensor carpi ulnaris, the extensor pollicis longus, or the extensor carpi radialis longus. On the palmar aspect, tendinopathy of the flexor carpi ulnaris and radialis may be seen. The symptomatology is often typical with pain on palpation and stretching. After the systematic plain x-ray, which is often normal, high-resolution static and dynamic ultrasound will reveal any loss of the fibrillar architecture and focal thickening of the tendons, effusion within the sheaths, and hyperemia on Doppler ultrasound. Ultrasound can be used to assess the retinacula and guide injections if necessary. Local compressive structures, such as synovial cysts, will be easy to identify. As with other tendinopathies, MRI is only used in cases where there are doubts about the diagnosis or when the evolution is unusual. Fat-suppressed T1-weighted and T2-weighted images are necessary, as well as intravenous injection of gadolinium. The signs of these tendinopathies consist of thickening of the tendons concerned; effusion within the sheath, which is clearly visible in fat-suppressed T2-weighted images; and the stigmata of tenosynovitis which will be revealed following the intravenous injection of a contrast agent. Any joint disease will be clearly visible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree