Chapter 15 IMAGING OF MUSCLE
MODALITIES
Magnetic Resonance Imaging
MRI is often considered the imaging modality of choice in the evaluation of a suspected muscle abnormality. This is primarily because of its superior soft tissue contrast, superb spatial resolution, and reproducibility. The standard MRI protocol includes a combination of axial and long axis T1- and T2-weighted images through the area of concern. This combination provides for excellent visualization of both normal compartmental muscle anatomy and for detection of pathologic processes within the muscles. Fat is bright on T1-weighted images, allowing for excellent contrast and depiction of the fat planes against the intermediate signal intensity of normal muscle. T2-weighted images clearly depict the increased water content of most muscle abnormalities, including muscle strain or tear and most soft tissue masses. Fat-saturation techniques or the use of intravenous gadolinium typically increase the conspicuity of lesions.
ANATOMIC VARIATIONS
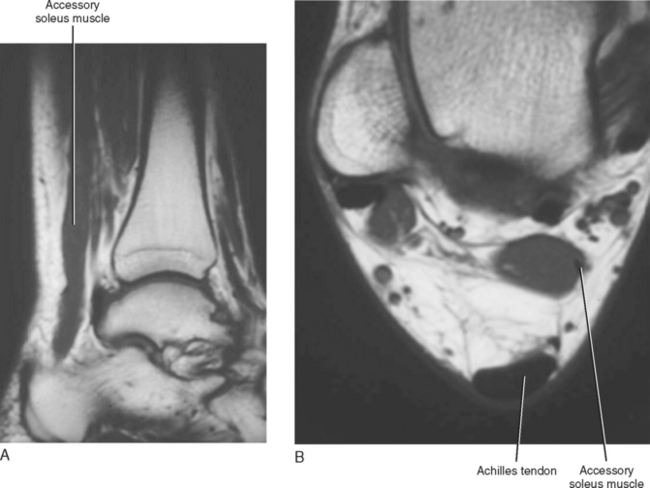
Anatomic variations of muscle are common and range from complete absence of a specific muscle to hypertrophy and even an accessory muscle. It is also common to identify variations in the attachment, course, and size of a particular muscle. Although these variations are not of themselves pathologic, they occasionally manifest with symptoms such as neurovascular entrapment or post-exercise pain, or even a palpable abnormality mimicking a mass (Fig. 15-1). MRI is particularly well suited to identifying variations in muscular anatomy and can depict the course, size, and shape of a muscle. Accessory muscles can be clearly differentiated from a soft tissue mass and can also be identified as the potential source of neurovascular entrapment (Box 15-1).
BOX 15-1 ANATOMIC VARIATIONS OF MUSCLES
Upper Extremity Entrapment Syndromes
Lower Extremity Entrapment Syndromes
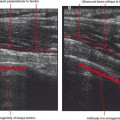
MUSCLE INJURY
Delayed Onset of Muscle Soreness
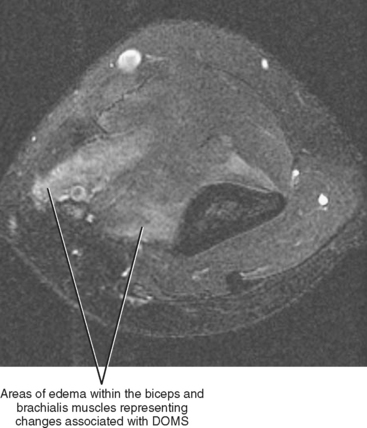
Delayed onset of muscle soreness (DOMS) describes a condition of muscle pain or soreness that occurs after acute muscle overuse (e.g., weight-lifting or aerobic exercise) and is usually self-limiting. The soreness typically begins within 2 to 3 hours of the activity and peaks at 2 to 3 days. The pain is centered at the myotendinous junction, and the muscle damage is at the ultra-structural level and is reversible. Although it is unusual to image a person because of DOMS, it is possible that a person may demonstrate MR findings associated with DOMS while being imaged for other reasons. The MR findings of DOMS are nonspecific and show areas of increased T2 signal within the involved musculature, occasionally mimicking a low-grade muscle strain (Fig. 15-2). Abnormal T2 signal has been shown to persist for up to 3 weeks after resolution of symptoms, and differentiation between DOMS and a grade I muscle strain requires close correlation with the clinical history and presentation.
Acute Myotendinous Injury
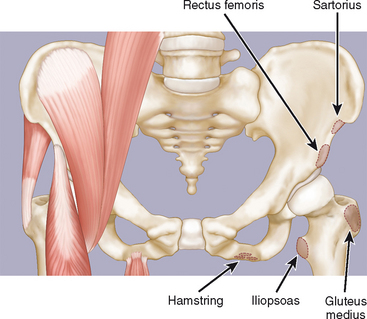
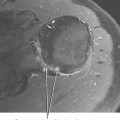
Acute myotendinous injuries occur when the load placed on the myotendinous unit exceeds the tensile strength of the unit. Injury typically occurs during eccentric contraction (contraction that occurs while the muscle is lengthening) and often involves a muscle that crosses two joints, such as the rectus femoris, gastrocnemius, and sartorius. Onset of pain is acute at the time of activity (unlike DOMS, in which the pain begins 2 to 3 hours after the activity). The location of injury within the myotendinous unit is age-related, with the “weak link” of the unit changing as an individual ages (Box 15-2).
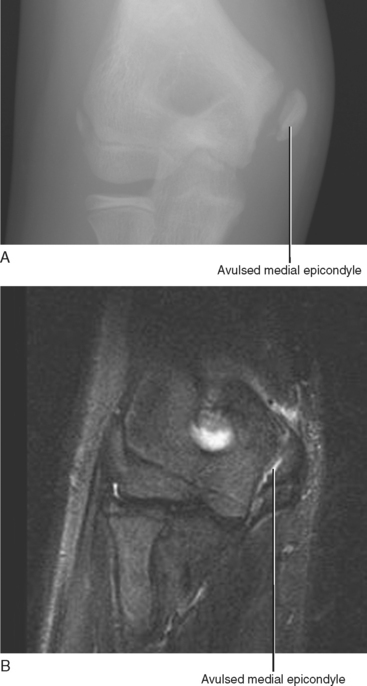
Apophyseal avulsion injuries typically occur in adolescent athletes (e.g., sprinters, long jumpers, cheerleaders, hurdlers, gymnasts) and result from violent muscular contractions. They are equivalent to a muscle pull in the mature athlete and most commonly occur in locations about the pelvis (Fig. 15-3). The elbow is another common location of apophyseal injury, often occurring in adolescent throwers (Fig. 15-4). Radiographs are usually sufficient to establish the diagnosis of an apophyseal avulsion injury when a cortical bone fragment is avulsed along with the tendon (Fig. 15-5). Occasionally, the tendon may avulse without an associated bone fragment, in which case MRI or ultrasound may be required to fully assess the extent of injury (Fig. 15-6; see also Fig. 15-4B). On MR imaging, a cortical avulsion fragment appears as a low-signal curvilinear structure on both T1- and T2-weighted images. Detection of the cortical avulsion fragment may be difficult because it is attached to the avulsed tendon, which also demonstrates low signal. A gradient-echo sequence or T1 sequence without fat saturation may be the most useful in detecting a small cortical avulsion fragment. After a complete avulsion, retraction of the torn tendon and adjacent osseous and soft tissue edema are often present. Although avulsion injuries can occur at nearly any location where a tendon attaches to bone, most apophyseal avulsion injuries in the adolescent patient occur in the pelvis, and knowledge of the specific attachment sites of various tendons can help establish the correct diagnosis (Table 15-1).