Key Facts
- •
Imaging findings in rheumatoid arthritis (RA) reflect the pathophysiology of the disease.
- •
Early radiographic findings include fusiform soft tissue swelling and juxtaarticular osteoporosis.
- •
Later radiographic findings include malalignment, uniform cartilage space narrowing, and bone erosions. Erosions begin near the joint margins (“bare areas”) and usually show no repair. Ankylosis is a late finding.
- •
Cervical spine alignment abnormalities are common and characteristic features of RA and may cause spinal cord compression. The most frequent cervical spine malalignment is anterior subluxation of C1 on C2.
- •
Computed tomography (CT) is generally reserved for special circumstances, such as evaluation of the skull base and cervical spine, several of the extraskeletal manifestations of the disease, or when magnetic resonance imaging (MRI) is contraindicated.
- •
MRI and ultrasound are sensitive methods for detecting synovitis, tendon damage, and bone erosion. MRI and ultrasound demonstrate soft tissues better than radiographs or CT.
Rheumatoid arthritis (RA) is a systemic inflammatory disease of unknown etiology that predominantly affects the musculoskeletal system. Identification of the disease and evaluation of its activity are essential in the routine clinical management of patients with this disorder. Imaging plays an important role.
Different facets of RA may be identified and monitored depending on the selected imaging modality. Currently, radiographs, computed tomography (CT), scintigraphy, magnetic resonance imaging (MRI), and ultrasound are the imaging tools available for the clinician who treats patients with RA. Radiographs continue to be the mainstay; however, advanced imaging techniques improve early diagnosis and more accurately monitor therapy and disease progression.
The conventional monitoring of disease activity in RA is assessed with the combination of clinical examination (e.g., joint swelling, tenderness) and measurement of biochemical surrogate markers (e.g., serum C-reactive protein). The need for better strategies, such as imaging, for early detection and disease monitoring has become even more necessary with the current revolution in treatment options for RA. Early aggressive therapy with disease-modifying drugs is now recognized as critical in order to optimize long-term functional outcome and reduce morbidity. With the need for early and aggressive therapy, imaging strategies are being developed and adopted that emphasize early diagnosis and accurate monitoring.
Patients with polyarthritis, minimal physical exam findings, and normal radiographs are candidates for MRI for early diagnosis.
Given the array of imaging tools available, it is important to understand how each modality may help in the diagnosis and management of patients with RA.
An understanding of the way imaging may help in the management of extraarticular complications of RA is equally important. Imaging may also differentiate other conditions from RA. This chapter describes the current and emerging roles of imaging in the management of patients with RA. Suggestions on clinical use for each imaging modality are provided.
GENERAL IMAGING CONSIDERATIONS
Radiographic Findings
Imaging depicts joint derangement and mirrors the pathophysiology of RA. Imaging findings separate the disease into early, classical, and late stages. In the early stage, the nonspecific radiographic findings of periarticular edema, synovial joint distension (due to synovitis and joint effusion), and periarticular osteopenia may be seen. These early stage findings often result from inflammation in and adjacent to the thickened synovium that is infiltrated with inflammatory cells and granulation tissue (pannus).
Pannus means “blanket” and refers to the invasive hyperplastic synovium that develops in RA.
Pannus is a hallmark of RA and contributes to cartilage loss and bone erosions.
As the disease progresses, classic findings include a combination of cartilage space narrowing, erosions, and additional soft tissue thickening in specific joint locations. This combination is characteristic of RA, although mixed connective tissue disease and overlap syndromes may occasionally produce similar findings.
Classic imaging findings represent precise pathologic changes in the joint. The joint space narrowing signifies cartilage loss.
The term cartilage space rather than joint space is used in this text to emphasize that cartilage is responsible for most of the thickness of the space between bony articulations, although joint fluid and synovitis may also contribute to this “space.”
Erosions are generally irreversible focal and irregular defects in cortical and trabecular bone. The late stages of joint derangement mark a progression of these processes from erosions and cartilage loss to ankylosis or joint subluxation/dislocation and generalized joint destruction. Usually, once the late stages of joint derangement have occurred, the diagnosis of RA is well known.
Other Imaging Modalities
Each imaging modality characterizes certain facets of the underlying joint derangement. This modality-dependent characterization depends on the stage of the disease and the joint structures and pathophysiology best characterized by the imaging technique. There are strengths and limitations to each modality. Although radiographs provide a rapid assessment of global and regional joint involvement by RA, ultrasound and MRI have advantages in characterizing soft tissue structures including synovitis and joint effusion. These are phenomena that tend to occur early in the disease and are not as well demonstrated on radiographs.
OSTEOARTICULAR IMAGING FEATURES (GENERAL AND SPECIFIC JOINTS)
Radiography
Radiography is the initial imaging modality of choice for the workup and monitoring of patients with RA. Radiography is the traditional gold standard for assessment of joint damage. As part of the initial evaluation, radiographic findings may confirm the clinical suspicion of RA or may suggest other diagnostic possibilities. Characteristic radiographic findings are part of the American College of Rheumatology (ACR) classification criteria for RA ( Box 20-1 ).

The advantages of radiography include low cost, high availability, possibility of standardization and blinded centralized reading, validated assessment methods, and reasonable reproducibility. Radiography may be used to characterize multiple joints rapidly, and experience with radiography for evaluating rheumatoid patients is well developed. Because of its exquisite resolution and depiction of bony structures, radiography is very good at detecting erosions. Bone demineralization (osteopenia/osteoporosis) may be seen on radiography but not ultrasound or MRI.
Radiographs are often sufficient to provide a global assessment of regional arthritis damage. However, their projectional nature limits three-dimensional (3D) visualization of bony structures and soft tissues. Other disadvantages of radiography include its relative insensitivity to early joint damage and limited assessment of soft tissue abnormalities.
Conventional radiography may help differentiate RA from other joint pathologic entities such as osteoarthritis (OA), psoriatic arthritis, and neoplasms. Also, it may help identify a secondary process affecting the joint of patients with known RA, such as osteomyelitis, septic arthritis, pathologic or stress fractures, and amyloidosis. As noted previously, the radiographic abnormalities of the appendicular joints may be separated into early, classic, and late findings.
Early Radiographic Findings
The early radiographic findings are nonspecific periarticular soft tissue swelling with a fusiform configuration and periarticular osteopenia ( Figure 20-1 ). Soft tissue swelling occurs from a combination of joint effusion, edema, synovial enlargement (pannus formation), and/or tenosynovitis. Osteopenia typically becomes more generalized as the disease progresses. Initially, the small joints may widen as a result of effusion; however, as cartilage becomes eroded, the cartilage spaces narrow.

Classic Radiographic Findings
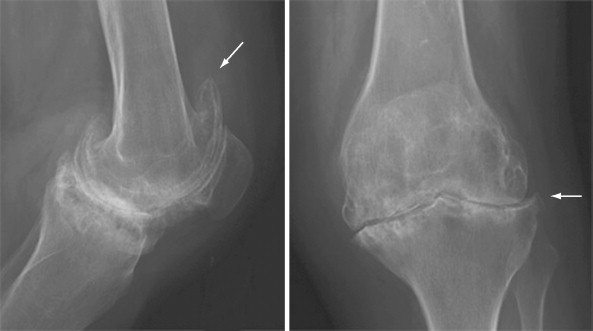
Marginal erosions herald classic findings of RA. Erosions usually begin at the intracapsular articular margins—a region of exposed bone between the joint capsule and the start of the cartilage surface. This area of uncovered bone is termed the bare area ( Figure 20-2 ).

The “bare areas” of the joint—areas within the joint capsule that are not covered by thick cartilage—are the earliest sites of erosion in RA.
The mechanism that produces marginal erosions is thought to be a combination of direct mechanical action of the pannus and the action of soluble factors liberated by the pannus that may stimulate bone loss. Surface resorption may be present along areas of bone that are adjacent to inflamed tissue, such as adjacent to tenosynovitis.
Cartilage loss in RA tends to involve the joint uniformly, instead of along weight-bearing portions of the joint as in OA. For example, axial migration of the femoral head with uniform joint space narrowing is more typical of RA than is superior migration, which is typical of OA ( Figure 20-3 ).

Hypertrophic bone formation, increase in bone mineral density, or repair of erosions is occasionally present in RA and may suggest a favorable treatment effect.
Treatment may result in erosions developing sclerotic margins due to repair.
However, periosteal new bone is uncommon, being more frequent in psoriasis, Reiter’s disease, and juvenile RA. Osteophyte formation is one hallmark of OA that is generally easy to distinguish from RA.
Late Radiographic Findings
Continued synovial inflammation coupled with abnormal biomechanics eventually result in significant alteration in joints. Subluxations from ligament, tendon, and joint capsule laxity become more pronounced and may lead to frank dislocations. Once RA progresses to cartilage loss, the altered mechanics predispose to pressure erosions at sites of bone-on-bone rather than cartilage-on-cartilage interfaces.
Progressive loss and obliteration of the cartilage space spreads throughout the joint. This pancompartmental distribution in such joints as the wrist and knee is characteristic of RA and helps differentiate RA from selective compartmental changes encountered in a variety of other articular disease process. Fibroosseous fusion of joints (ankylosis) is a late complication that may occur after complete cartilage loss. The wrist and midfoot bones are the most common locations for fusion. However, ankylosis is a more common feature of juvenile RA than adult RA.
Another late consequence of altered biomechanics in joints affected with RA is secondary OA. Persistent use of a joint with the predisposing anatomic abnormalities of RA may cause the joint to develop osteophyte formation, subchondral sclerosis, and subchondral cysts ( Figure 20-4 ). The result is a mixed picture on radiographs of both the initial and persistent arthritic changes from RA and the subsequent secondary changes from OA.
Distribution of Articular Involvement
Radiographs provide a global assessment of regional arthritis involvement. Although the distribution of radiographic abnormalities in RA is somewhat variable, it is generally symmetrical and polyarticular. RA targets synovial joints; thus the distribution of involvement will correlate with the locations of synovial joints and the synovial lining in the joint. There is a predilection for symmetric involvement of the distal extremities, hands, wrists, and feet, but the elbows, knees, shoulders, and hips are often affected. In the axial skeleton, imaging abnormalities in the articulations of the cervical spine are more often encountered than are changes in the thoracolumbar spine or sacroiliac joints.
Radiographic Appearance in Specific Joints
Hands
Alterations in the hands by RA are well described. These target characteristic locations within certain joints and display characteristic patterns of joint distribution. Soft tissue swelling and periarticular osteoporosis emerge early in the disease and are the indirect signs of synovitis and joint effusion. The index and middle finger metacarpophalangeal (MCP) joints are usually the earliest and most often affected.
The index and middle finger MCP joints show the earliest features of RA.
As the disease progresses, marginal erosions and concentric loss of the joint space develop and may eventually progress to malalignment and joint ankylosis.
Soft Tissues
Both the character and distribution of soft tissue swelling/effusion in the hands are important in identifying early RA. Although soft tissue abnormalities are better detected with MRI or ultrasound, localization of soft tissue swelling to the proximal interphalangeal (PIP) joints and MCP joints is suggestive of RA even in the absence of bone abnormalities (see Figure 20-1 ). Fusiform swelling of the PIP joints is characteristic of RA, whereas swelling secondary to OA is often asymmetric, located most often at the distal interphalangeal (DIP) joints, and usually accompanied by osteophytosis. MCP soft tissue swelling/joint effusion may be demonstrated by widening of the MCP joint, bulging of the web spaces, or increased convexity of the marginal soft tissues adjacent to the MCP joints of the thumb, index, and fifth fingers.
Erosions
The joints of the hands affected by soft tissue swelling are also the joints that may be involved by erosions. The earliest bone changes are demonstrated at the bare areas of the radial aspects of the MCP joints where the normal smooth cortex is visible (see Figure 20-2 ). Bare areas are located at the margins of the joint where bone cortex is relatively unprotected by overlying articular cartilage. This bare area is the region of bone cortex between the thick overlying articular cartilage and the joint capsule. Early marginal erosions are seen on magnification radiographs as localized cortical thinning and a dot-and-dash pattern of cortical disruption. More advanced marginal erosions show loss of cortex with or without preservation of underlying trabeculation.
In addition to marginal erosions, compressive (pressure) and superficial surface resorption may occur in the hands. The mechanism of compressive erosion is the collapse of osteoporotic bone as muscular forces pull the articular surfaces together, typically at the MCP joints. Surface resorption occurs at regions of bone adjacent to inflamed tendons, such as at the distal ulna ( Table 20-1 ).
Ankylosis
As destruction of cartilage and bone progresses, the joint space may be destroyed completely. Ankylosis is a fibroosseous fusion of joints after complete cartilage loss and represents the chronic, end-stage sequela of RA.
Ankylosis is a fibroosseous fusion of joints after complete cartilage loss. It most often affects the carpals and tarsals.
In the hands, ankylosis may occur at the MCP and PIP joints, but fusion is more frequent in the carpal and tarsal bones.
Malalignment
Alignment abnormalities of the hand are common and classic in RA and are attributed to the direct effect of the disease on the articulations, tendons, and ligaments. Common and classic alignment abnormalities include swan-neck, boutonnière and windswept deformities, and flexion/hyperextension-subluxation/dislocations at the thumb.
Swan-neck deformity consists of hyperextension at the PIP joint and flexion at the DIP joint. This deformity results primarily from synovitis of the flexor tendon sheath. With flexion limited at the PIP joint, hyperextension ensues from intrinsic muscle pull. The DIP joint is held in flexion from pull of the flexor profundus tendon.
Boutonnière deformity is a combination of flexion at the proximal interphalangeal and extension at the DIP joints. In patients with the boutonnière deformity, the normal balance between the tendon mechanism and ligamentous restriction is disrupted. Extension is ineffective due to lengthening of the central extensor tendon from capsular distension. The lateral extensor tendon slips fall volar to the axis of motion of the PIP joint and act as flexors of this joint. The extensor tendon slips also produce hyperextension at the DIP joint from increased pull.
Windswept deformity represents one of a variety of MCP and PIP joint deformities. Patients with windswept deformity have symmetric ulnar subluxations and dislocations of the MCP and PIP joints. The windswept deformity affects patients with systemic lupus erythematosus and Jaccoud’s arthropathy as well, but these patients lack the characteristic erosions of RA. In hands affected by RA, ulnar deviation and palmar subluxations are common, being found in 25% to 65% and 20% to 68%, respectively.
New Bone Formation
Increased amounts of endosteal bone may form in the distal phalanges. This condition, called terminal phalangeal sclerosis or acral sclerosis , occurs significantly more frequently in women with RA. Although it may be found in normal individuals, terminal phalangeal sclerosis may also be more frequent in systemic lupus erythematosus (SLE), dermatomyositis, and psoriatic arthritis.
Sclerosis of the distal phalanges may be seen in RA, SLE, and sarcoidosis but may be a normal finding.
Rarely, repair of erosions may occur and bone density may increase, especially in patients treated with methotrexate or with an anti–tumor necrosis factor antibody.
Wrists
As in the hands, alterations in the wrists due to RA include soft tissue swelling, erosions, joint space narrowing, alignment abnormalities, and ankylosis. These abnormalities also tend to affect particular locations in the joints and tend to be distributed in specific joints that are characteristic for RA. Abnormalities in the wrist are frequently accompanied by involvement in the fingers, either concomitantly or following carpal dominant rheumatoid disease.
Soft Tissues
Soft tissue swelling/edema is depicted on radiographs by obliteration of the fat lines and thickening and increased density of the soft tissues. Soft tissue swelling may be present at any of the compartments of the wrist due to synovial enlargement and/or joint effusion. Intercarpal, carpometacarpal, and radiocarpal joints; overlying tendons; and/or the ligamentous structures may be affected. Soft tissue swelling at the medial aspect of the ulnar styloid is a characteristic early finding in RA and is produced by tenosynovitis of the extensor carpi ulnaris tendon. The normal fat lines around the extensor carpi ulnaris on the ulnar side of the wrist and the fat outlining the extensor pollicis brevis and abductor pollicis longus tendons on the radial side may be obscured by soft tissue swelling.
Infiltration of fat by inflammatory changes obliterates the normal fat lines seen along tendons such as the extensor carpi ulnaris.
Rheumatoid involvement of the tendons coursing through the carpal tunnel may produce carpal tunnel syndrome. Although masses involving the carpal tunnel are better characterized by MRI or ultrasound, radiographs may suggest RA involvement by demonstrating displacement and distortion of the pronator fat line that normally parallels the volar side of the distal radius.
Erosions
Erosions usually involve the intercarpal and radiocarpal articulations symmetrically. As with other joints, bare areas and bony locations adjacent to synovitis are more likely to develop erosions. The ulnar styloid is a particularly common site for erosion.
The ulnar styloid is a common site for early erosion in RA.
Erosions of the triquetrum and pisiform bones are common in early RA, although the disease can involve any carpal bone. Synovial inflammation at the radiocarpal compartment will erode the radial styloid process and adjacent scaphoid bone. However, there is a normal mild degree of notching at the radial aspect of the scaphoid that must be distinguished from true erosive change.
Ankylosis
Disease progression may lead to pancompartmental changes in the wrist with obliteration of the joint spaces, large osseous erosions, and bony ankylosis. This pancompartmental distribution is characteristic of RA and is extremely unlikely to be the result of other disease processes that are more likely to involve only selected compartments.
Malalignment
Wrist malalignment and deformity generally fall into several well-described patterns of radiocarpal, intercarpal, and radioulnar/distal ulnar malalignment ; however, given the intricate relationships and number of ligaments, tendons, and bones at the wrist, the classification of wrist malalignment and deformity should serve primarily as a guide, as there is overlap among the different types. Radiocarpal malalignment appears as ulnar and palmar deviation of the proximal carpal row as the carpus slides off the inclined articular surface of the distal radius. Prevalence of radiocarpal malalignment may be as high as 70% of patients with RA. Intercarpal malalignment may occur in dorsal or volar directions. Dorsal intercalated segment instability (DISI) results in an increased scapholunate angle (normal, 45 degrees) on lateral radiographs as the scaphoid rotates into a more volar flexed position and the lunate tilts dorsally. The scapholunate angle is reduced in volar intercalated segment instability (VISI) as the lunate rotates into volar flexion and there is volar shift of the capitate. Inferior radioulnar and distal ulnar malalignment include dorsal subluxation of the distal ulna and diastasis of the inferior radioulnar compartment. With the end of the ulna subluxed dorsally, patients are predisposed to mechanical rubbing and tenosynovitis of the adjacent extensor compartments and eventual rupture of these tendons. Scapholunate advanced collapse (SLAC) is also seen in RA. With SLAC wrist, the capitate migrates proximally after complete tear of the scapholunate ligament (see Figure 20-2 ) ( Table 20-2 ).
Feet and Ankles
The radiographic features of soft tissue swelling, erosions, joint space narrowing, alignment abnormalities, and ankylosis found in the hands and wrists are also seen in the feet and ankles. The characteristic and common abnormalities tend to be symmetric, usually affect particular locations in the joints, and distribute among specific joints that are predisposed to synovitis. The metatarsophalangeal (MTP) joints are among the first to be affected by RA.
The MTP joints are the first sites of involvement in up to 20% of RA patients.
Ten percent to twenty percent of RA patients have the initial manifestation of the disease in the MTP joints.
A classic soft tissue abnormality in the heel is soft tissue thickening in the pre-Achilles’ bursa ( Figure 20-5 ). The enlarged pre-Achilles’ bursa can be identified as a soft tissue mass located between the posterior superior surface of the calcaneus and the anterior aspect of the distal Achilles’ tendon. The soft tissue swelling generally precedes erosions at the posterior superior calcaneus adjacent to the Achilles’ insertion. Identical findings may be present in ankylosing spondylitis and reactive arthritis (Reiter’s disease), but RA is the most common cause of these findings. Plantar calcaneal erosions mimic those seen with psoriasis. Rheumatoid nodules adjacent to the Achilles’ and other tendons are better demonstrated with ultrasound or MRI than radiography.

Rheumatoid erosions in the foot and ankle involve similar joints as in the hand and wrist, including the PIP, MTP, intertarsal, and tibiotalar joints. The earliest cortical changes are best demonstrated in the medial aspects of the first through fourth metatarsal heads and the medial and lateral aspects of the fifth metatarsal head bare areas.
Erosion may occur first at the fifth MTP joint.
At the ankle, uniform cartilage loss with resultant joint space narrowing at the tibiotalar joint has its corollary with the radiocarpal joint. Fibular notch erosion at the distal tibiofibular joint is characteristic for RA ( Figure 20-6 ).

Large Appendicular Joints
Large appendicular joints—the knee, hip, elbow, and shoulder—involved by RA share many radiographic features. The predominant feature of RA in large appendicular joints is uniform and severe cartilage space loss (see Figure 20-4 ). Progressive destruction of the chondral surface leads to diffuse loss of the cartilage space. Erosions, subchondral cystic lesions, and subchondral sclerosis are often present in the large appendicular joints, but these features are present to a lesser extent than the uniform loss of cartilage space.
Interosseous cystic lesions (or geodes) may occur in the large joints involved by RA. These geodes appear on radiographs as lucencies of varying shape and size. Mechanisms for these lesions include intrusion of granulation tissue from the joint through a defect in the cortical bone or formation of rheumatoid nodules within the bone.
Knee
The knee is frequently affected in RA and is often affected early in the disease course. Soft tissue swelling is the most common, but unfortunately nonspecific, finding. Up to 80% of positive knee radiographs in patients with RA may have soft tissue swelling/effusion as the only abnormality.
Effusion will be visible as a soft tissue density in the suprapatellar region on the lateral knee radiograph. Other findings of knee effusion include anterior displacement of the patella on the lateral view and soft tissue density adjacent to the femoral condyles on the anterior view. Synovial enlargement or the combination of synovial enlargement with effusion have similar findings on radiographs ( Table 20-3 ) .
No distinction can be made between joint effusion and pannus on radiographs.
In addition, RA may enlarge popliteal cysts producing soft tissue masses in the posterior aspect of the knee. These cysts may rupture into the calf and cause pseudophlebitis syndrome.
Rupture of a popliteal cyst in a patient with RA may produce symptoms mimicking phlebitis.
Popliteal cysts can become very large palpable masses that may dissect down the calf and may be confirmed by ultrasound or MRI ( Figure 20-7 ).

As the disease progresses, small erosions on the medial, lateral, and posterior margins of the femoral condyles and tibial plateaus may be observed. Uniform bicompartmental (medial and lateral tibiofemoral) or uniform tricompartmental (including the patellofemoral compartment) joint space narrowing occurs as a consequence of cartilage loss (see Figure 20-4 ).
The uniform cartilage loss in RA is in contrast to the asymmetric involvement of knee compartments in OA.
Subchondral erosions and geodes may also develop. As with the hip, superimposed OA may complicate the classical findings of RA in the knee.
Hip
Abnormalities at the hip are much less common than the peripheral joints and tend to be present in patients with long-standing and severe forms of RA. Although soft tissue swelling/joint effusion may be present on radiographs as expansion and increased density of the soft tissues around the femoral neck with obscuration or displacement of the adjacent fat planes or as effacement of the obturator internus muscle fat plane medial to the acetabulum, these findings are unreliable and have been shown to have no value in the detection of joint effusion in adults. The one reliable finding of hip effusion on radiographs is an increase in the tear drop distance ( Table 20-4 ).
The distance between the lateral aspect of the acetabular teardrop shadow on the anteroposterior radiograph and the medial femoral head should be symmetric; differences of only 1 mm between the sides suggest hip joint effusion on the side with the greater measurement ( Table 20-4 ).
Uniform loss of the cartilage space is typically bilateral and symmetric. With uniform loss of the articular cartilage, the femoral head moves along the axis of the femoral neck (termed axial migration ). Axial migration helps distinguish RA from OA, which tends to cause superior migration with joint space narrowing at the superior weight-bearing portion of the joint. At times it may be difficult to separate RA from OA when features of both conditions are present. Secondary OA in RA occurs, and sometimes OA will develop axial migration; however, the findings in OA tend to be more asymmetric in comparison with the contralateral joint.
With complete obliteration of the hip cartilage space, the femoral head and acetabulum will protrude into the pelvis (see Figure 20-3 ). This acetabular protrusion (acetabular protrusio) is generally defined as displacement of the femoral head medial to the acetabular ilioischial line. Severe instances of RA of the hip may lead to fibrous ankylosis.
Patients with RA are at increased risk of osteonecrosis of the femoral head, particularly those patients who are treated with corticosteroids. Several staging systems have been developed that rely on imaging abnormalities to grade severity of osteonecrosis and direct patients for different therapies. Radiographic abnormalities in osteonecrosis include cysts and sclerosis, subchondral lucency due to a subchondral fracture (the crescent sign), flattening of the femoral head, cartilage space narrowing with or without acetabular involvement, and finally advanced degenerative changes. When osteonecrosis of the femoral head is suspected but the radiographs are normal or nondiagnostic, MRI or bone scan may indicate osteonecrosis before it is visible radiographically.
Elbow
Abnormalities at the elbow are common in RA and, although symmetric, may preferentially affect the dominant arm. A classic radiographic finding that indicates an elbow joint effusion/soft tissue swelling is the fat pad sign ( Figure 20-8 ). On the lateral radiographic view of a normal elbow obtained with the arm flexed at 90 degrees, overlying bony structures obscure fat hidden in the olecranon fossa.

An intracapsular, extrasynovial fat pad is present both anteriorly and posteriorly along the elbow joint. When this fat pad is visible, joint distension is likely.
When an effusion and/or synovial thickening are present, the fat in the olecranon fossa is displaced dorsally and produces the fat pad sign: abnormal radiolucency (fat) posterior to the distal humerus. The supinator fat (superficial to the supinator muscle) may also be displaced when severe swelling is present. More advanced radiographic changes at the elbow include uniform joint space narrowing, marginal erosions, and eventual osteolysis of large portions of the distal humerus and proximal radius and ulna, often mimicking neuropathic changes.
Shoulder
The primary structures affected by RA in the shoulder include the glenohumeral joint, rotator cuff, and distal end of the clavicle. Progressive cartilage destruction at the glenoid fossa and humeral head leads to diffuse and uniform loss of the glenohumeral joint space ( Figure 20-9 ). Erosions and pseudocysts tend to be located at the superolateral aspect of the humeral head adjacent to the greater tuberosity. Large pressure erosions may develop on the medial aspect of the surgical neck of the humerus from the rubbing and possibly inflammatory change at the adjacent glenoid margin and inferior glenohumeral capsule.











