Fig. 19.1
Schematic drawing of the different stages of motion during a tennis serve. (a) Windup (knee flexion, trunk rotation), (b) early cocking, (c) late cocking (maximal abduction-external rotation), (d) acceleration, (e) deceleration, (f) follow-through
19.2.1 Rotator Cuff Disease
19.2.1.1 Internal Impingement
This type of impingement is most frequent in young elite tennis players. Not all patients are symptomatic. It is thought to be secondary to microinstability, resulting from stretching of the anterior capsular structures while throwing (Anderson and Alford 2010). This position occurs during the late cocking phase of throwing. Posterior capsular thickening and ossification (Bennett lesion) may also occur under these circumstances. Capsular tightening leads to loss of internal rotation (glenohumeral internal rotation deficit or GIRD) and a posterosuperior shift of the axis of rotation of the humeral head on the glenoid, thereby causing repetitive impaction of the greater tuberosity of the humerus against the posterosuperior aspect of the glenoid as the arm is abducted and externally rotated. This may result in degeneration and partial cuff tears, particularly infraspinatus and posterior supraspinatus, fraying of the posterosuperior labrum and subcortical cystic changes of the humeral head at the posterior greater tuberosity. MR arthrography may demonstrate these findings (Fig. 19.2). Scanning in abduction and external rotation (ABER) position is more sensitive to subtle findings (Anderson and Alford 2010).
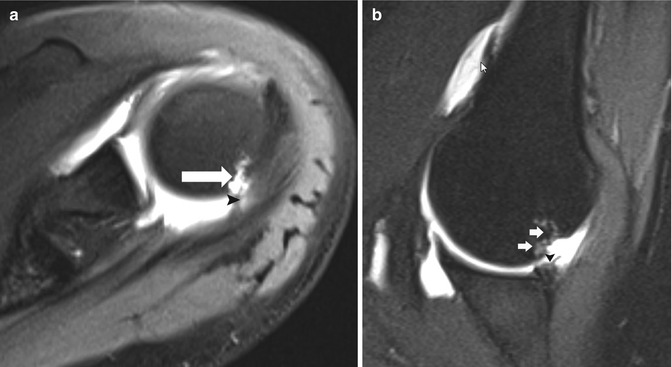
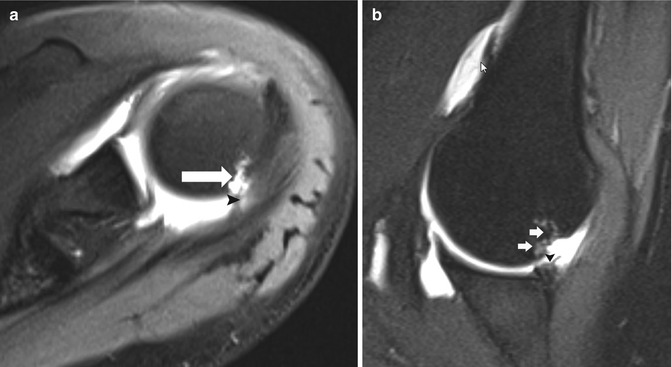
Fig. 19.2
Shoulder posterosuperior impingement in a tennis player. (a) Axial fat-suppressed T1-weighted MR arthrography demonstrates a small articular tear of the infraspinatus tendon (arrowhead). Note also the cystic changes in the greater tuberosity (arrow). (b) Oblique axial fat-suppressed T1-weighted MR arthrography in abduction-external rotation (ABER) position shows cystic changes in the greater tuberosity (arrows) and irregular delineation of the posterosuperior labrum (arrowhead)
19.2.1.2 External Impingement
This type of impingement occurs most often in older recreational tennis players. Although rotator cuff degeneration and tearing may be due to intrinsic factors, such as diminished vascularity and overuse, it has been proposed that the vast majority of cuff tears are secondary to chronic impingement between the humeral head and coracoacromial arch. The shape of the undersurface of the anterolateral acromion can be classified as flat (I), curved (II), anteriorly hooked (III), or convex (IV). Types II and III in particular are associated with higher incidence of impingement and rotator cuff abnormalities. Downsloping of the acromion and a thickened coracoacromial ligament may also result in narrowing of the outlet and impingement of the distal part of the supraspinatus tendon. The spectrum of rotator cuff pathology ranges from tendinopathy to partial and full-thickness tears, which can be demonstrated on both ultrasound and MRI (Figs. 19.3, 19.4, 19.5, 19.6, and 19.7).
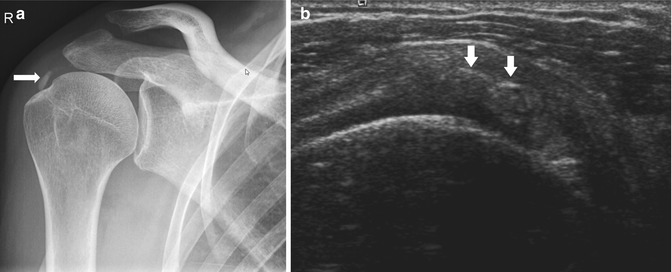
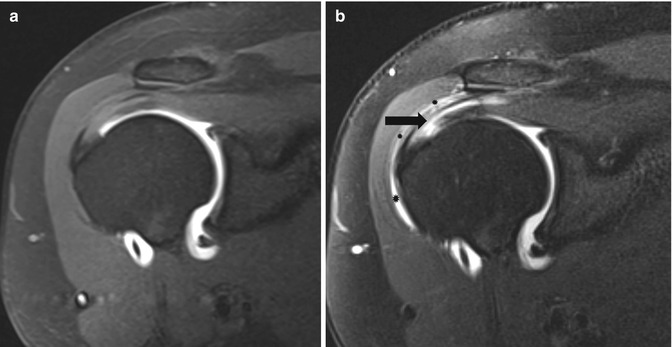
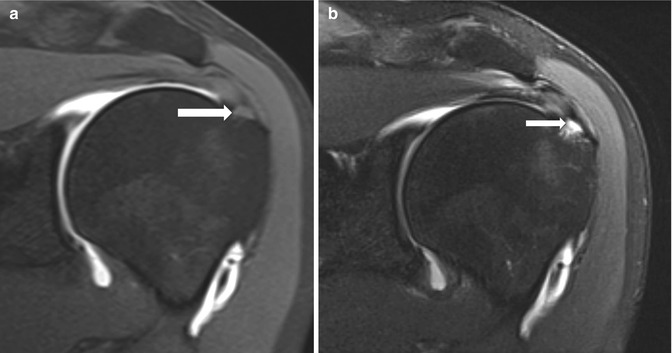
Fig. 19.3
A 28-year-old female tennis player with subacromial bursitis, presenting with shoulder pain. Sagittal ultrasound image shows focal thickening of the subacromial bursa (calipers)
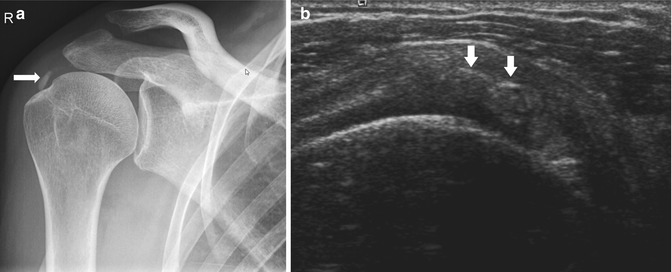
Fig. 19.4
A 35-year-old tennis player with calcifying tendinopathy, presenting with shoulder pain. (a) Plain radiograph shows calcifications at the greater tuberosity (arrow). (b) Axial ultrasound shows intratendinous hyperechoic reflections with retro-acoustic shadowing (arrows)
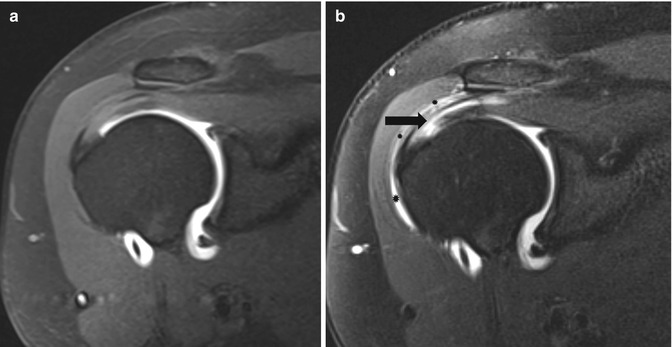
Fig. 19.5
A 38-year-old tennis player with a partial-thickness supraspinatus tear at the bursal side. (a) Oblique coronal fat-suppressed T1-weighted MR arthrography shows normal delineation of the articular side of the supraspinatus tendon. (b) Oblique coronal fat-suppressed T2-weighted MRI shows an intratendinous fluid cleft (arrows) with subtle extension to the subacromial bursa (stars)
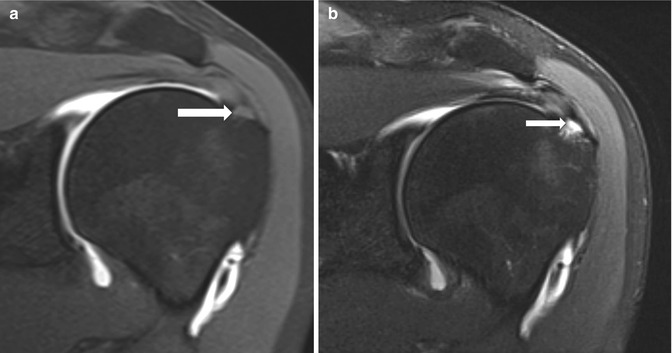
Fig. 19.6
A 61-year-old tennis player with a small intratendinous supraspinatus tear. (a) Oblique coronal fat-suppressed T1-weighted MR arthrography demonstrates normal delineation of the articular side of the supraspinatus tendon. There is a subtle area of intermediate signal in the distal supraspinatus tendon (arrow), not corresponding to contrast infiltration into the tendon. (b) Oblique coronal fat-suppressed T2-weighted MRI shows a small intratendinous fluid cleft (arrow)
Fig. 19.7
A 64-year-old recreational tennis player with a full-thickness supraspinatus tear. Oblique coronal fat-suppressed T1-weighted MR arthrography shows gadolinium contrast extending into the subacromial bursa through a defect in the supraspinatus tendon (asterisk). There is a hooked acromion impinging on the supraspinatus tendon (arrow)
19.2.1.3 Tensile Failure
During the deceleration phase of the throwing motion, the muscles of the rotator cuff contract to slow the arm and place the cuff under tension. These tensile forces can result in undersurface tears of the supraspinatus or infraspinatus, aka “rim rent” or “partial articular surface tendon avulsion” (PASTA) tears. MR arthrography with scanning in ABER position is recommended to demonstrate these often subtle tears, which may be missed if the arm is internally rotated (Fig. 19.8) (Anderson and Alford 2010).
Fig. 19.8
Small rim rent tear. Oblique coronal fat-suppressed T1-weighted MR arthrography shows a small partial-thickness articular surface tendon avulsion (PASTA) of the anterior fibers of the supraspinatus tendon near its insertion at the greater tuberosity (arrow)
19.2.1.4 Subscapularis Tears and Lesions of the Long Head of the Biceps Tendon
Impingement of the undersurface of the subscapularis tendon against the anterosuperior glenoid may occur in a position of flexion and internal rotation in tennis players. This may cause partial articular tears of the subscapularis tendon. Medial subluxation of the biceps tendon may occur. Stretching and traction forces of the long head of the biceps may result in a spectrum of pathologic conditions, including tendinopathy and partial or complete tendon tears. On MR arthrography, the subscapularis and the vertical portion of the biceps tendon are best evaluated on axial images (Fig. 19.9), whereas the horizontal portion is better evaluated in the oblique sagittal and oblique coronal planes (Anderson and Alford 2010).
Fig. 19.9
Subscapularis tear and biceps tendon dislocation. Axial fat-suppressed T1-weighted MR arthrography demonstrates a partial tear of the subscapularis tendon (arrowhead) with medial intrasubstance dislocation of the long head of the biceps tendon (arrow)
19.2.2 Capsulolabral Pathology
19.2.2.1 SLAP Tear
Injuries to the superior labrum at the biceps-labral anchor (superior labrum anterior to posterior or SLAP tears) are common in tennis players due to chronic traction on the long head of the biceps during the deceleration phase (Anderson and Alford 2010).
The MRI findings of a SLAP tear include the extension of contrast between the labrum and the glenoid (Fig. 19.10). Care should be taken not to confuse normal variants with a tear. If contrast material under the cuff extends laterally, it should be called a tear. Contrast material undercutting the labrum obliquely toward the patient’s head is a normal finding in a sublabral sulcus, unless the contrast then extends medial to the perpendicular superior surface of the glenoid. If the labrum is absent or small involving the anterior-superior location only, one should consider a large Medial Glenohumeral Ligament (MGL) and the Buford complex; if the labrum appears to be separated only at the anterior-superior portion of the glenoid, the diagnosis should be a sublabral foramen. A posterior labral tear may result in the formation of a cyst at the superior scapular notch or spinoglenoid notch (Fig. 19.11), similar to the mechanism found in a meniscal cyst associated with a meniscal tear.

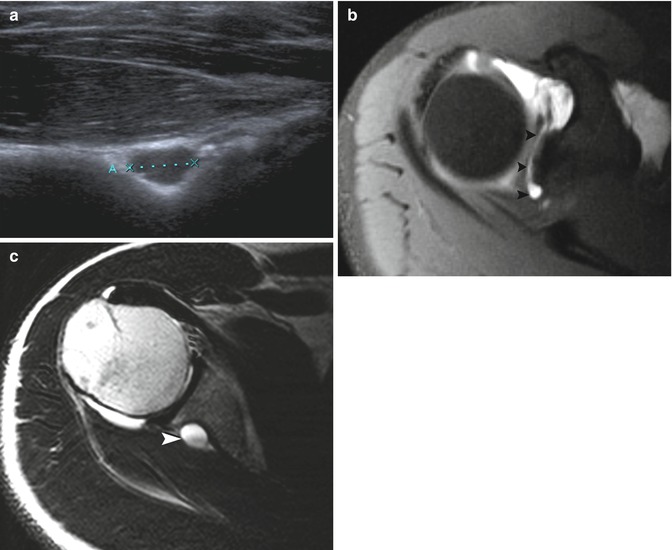

Fig. 19.10
SLAP lesion. Oblique coronal fat-suppressed T1-weighted MR arthrography shows lateral extension of contrast between the labrum and the proximal insertion of the long head of the biceps tendon (arrowhead)
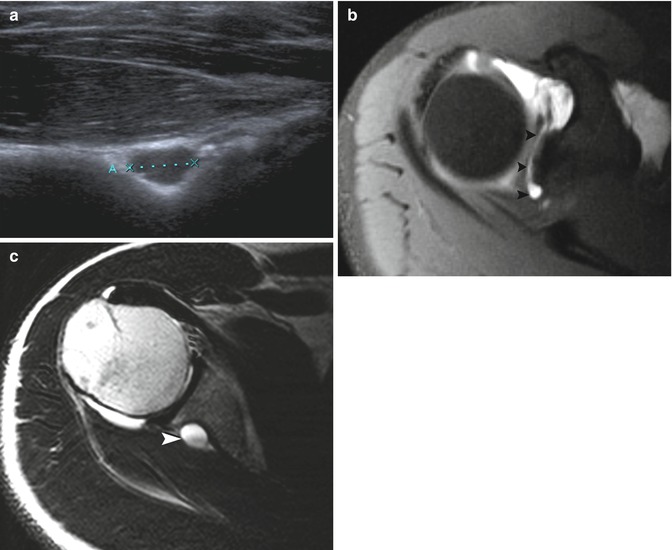
Fig. 19.11
A 30-year-old tennis player with a spinoglenoid cyst. (a) Transverse ultrasound image shows a cystic lesion within the spinoglenoid notch (calipers). (b) Axial fat-suppressed T1-weighted MR arthrography demonstrates contrast infiltration between the superior labrum and the glenoid bone, extending from anterior to posterior (SLAP) (arrowheads). (c) Axial T2-weighted MRI at a lower level shows a cystic lesion at the spinoglenoid notch (arrowhead)
19.2.2.2 Tear of the Anterior/Posterior Labrum
The anterior labrum and glenohumeral ligaments are repetitively stretched when the arm is abducted and externally rotated during the late cocking phase, whereas the posterior capsulolabral structures may be submitted to tensile forces when the arm is slowed during the deceleration phase. On MR arthrography, either anterior (Fig. 19.12) or posterior labral tears (Fig. 19.13), present as contrast infiltration within the labrum or between the labrum and glenoid. In normal circumstances, the normal capsule attaches directly along the base of the labrum at its junction with the osseous glenoid. Damage to the posterior capsulolabral system may cause posterior capsular stripping along the posterior margin of the glenoid (Fig. 19.14).
Fig. 19.12
An 18-year-old tennis player with an anterior labrum tear. Axial fat-suppressed T1-weighted MR arthrography demonstrates contrast infiltration within the anterior labrum and associated capsular stripping (arrowhead)
Fig. 19.13
Posterior labrum tear. Axial fat-suppressed T1-weighted MR arthrography demonstrates contrast infiltration between the posterior labrum and posterior glenoid (arrowhead)
Fig. 19.14
Posterior capsular stripping. Axial fat-suppressed T1-weighted MR arthrography demonstrates contrast infiltration along the posterior border of the glenoid (arrow)
19.2.3 Special Considerations in Children and Adolescents
As the physis constitutes the weakest link in the muscle-tendon-bone complex in the immature athlete, repetitive stress may lead to an ingrowth of cartilage from the physis into the metaphysis, appearing as widening of the physis on plain radiographs. If this occurs at the growth plate of the proximal humerus, it is known as Little Leaguer’s shoulder.
MRI may demonstrate widening of the physis and associated bone marrow edema. The widened growth plate is hypointense on T1-weighted images and hyperintense on T2-weighted images (Anderson and Alford 2010).
19.2.4 Stress Reactions of the Humerus
Stress reactions of the middle and distal humerus have been rarely reported in tennis players. This portion of the arm is susceptible to rotational stress, which occurs during the acceleration phase of the service motion, when the arm moves into internal rotation (Silva et al. 2007; Maquirriain and Ghisi 2006a). MRI is the imaging technique of choice for early detection, by demonstrating bone marrow edema and periosteal edema.
19.3 Elbow
19.3.1 Radial Side Lesions
Lateral epicondylitis is the most frequently encountered tendon lesion in the elbow. Even though the lesion is frequent in middle-aged nonathletes, due to its high prevalence in racquet sport players (Wenzke 2013), it has been designated as “tennis elbow.” It represents a chronic overuse injury, resulting from repetitive microtrauma to the extensor tendons at their insertion at the lateral epicondyle during supination, dorsiflexion, and radial deviation (Wenzke 2013). The extensor carpi radialis brevis is most frequently involved, followed by the extensor digitorum communis, the extensor carpi radialis longus, and extensor carpi ulnaris (ECU) (Frick and Murthy 2010; Walz et al. 2010).
Clinically, patients complain of pain at the lateral elbow radiating into the forearm, exacerbated by wrist extension and focal pressure tenderness at the lateral epicondyle (Kotnis et al. 2012).
Although imaging (ultrasound and MRI) is useful for evaluation of lateral epicondylitis, imaging abnormalities do not always correlate with the severity of the symptoms (Chourasia et al. 2013; Walton et al. 2011). Ultrasound has a reported sensitivity of approximately 80 % but a specificity of only approximately 50 % and a high false-positive rate (Levin et al. 2005). Therefore, ultrasound should be used only to evaluate the extent of disease in patients with typical clinical findings (Kotnis et al. 2012). Grayscale imaging may detect structural changes such as tendon thickening, hypoechogenicity, fibrillar disruption, partial tearing (Fig. 19.15), intratendinous calcification, and cortical irregularities. Power Doppler may be useful to assess hyperemia (Fig. 19.15). Some authors propose using an ultrasound scoring system (Table 19.1) to quantify structural changes (4-point scale) and hyperemia (5-point scale) (Poltawski et al. 2012).
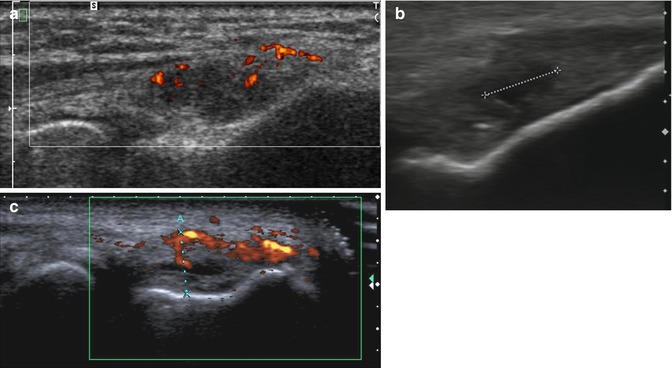
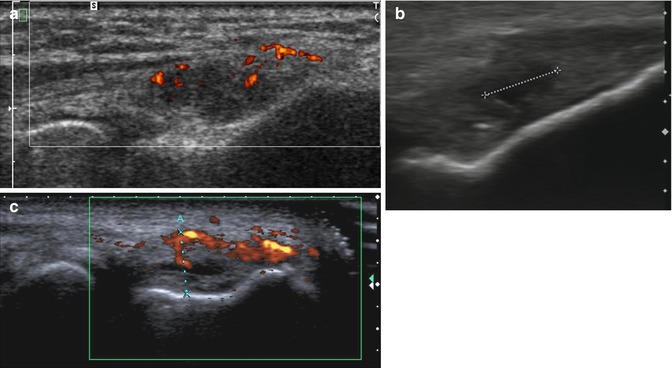
Fig. 19.15
Lateral epicondylitis in three different patients. Longitudinal ultrasound images show (a) thickening, hypoechogenicity, and increased power Doppler signal in the proximal extensor tendons; (b) partial tear presenting as a hypoechoic cleft (calipers) within the proximal extensor tendon; and (c) increased vascularity in the extensor tendons with a small intralesional hypoechoic cleft (corresponding to a partial tear)
Table 19.1
Ultrasound scoring system for quantification of lateral epicondylitis
Grade | Structural tendinous changes | Power Doppler changes |
|---|---|---|
0 | Normal | No signal |
1 | Minor | Single small signal |
2 | Less than 50 % involved | Less than 33 % signal increase |
3 | More than 50 % involved | 33–67 % signal increase |
4 | Not applicable | More than 67 % signal increase |
MRI shows areas of increased signal on T1- and T2-weighted images associated with tendon thickening or thinning (partial tears) (Fig. 19.16), or tendon discontinuity with a high-signal fluid-filled gap (full-thickness tears) (Kotnis et al. 2012; Walz et al. 2010). Large tears may be associated with tears of the lateral collateral ligament (Fig. 19.17). Axial FS T2-weighted images are particularly helpful for assessing the degree and extent of the tear and the presence of reactive bone marrow edema in the underlying lateral epicondyle.

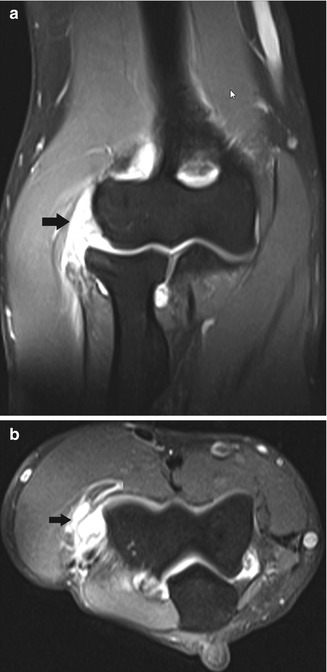

Fig. 19.16
Lateral epicondylitis. (a) Coronal T1-weighted MRI shows thickening and intermediate signal of the common extensor tendon and extensor carpi radialis brevis tendon origin (arrow). (b) Coronal fat-suppressed T2-weighted MRI shows an intratendinous focus of fluid signal in keeping with a partial tear (arrow)
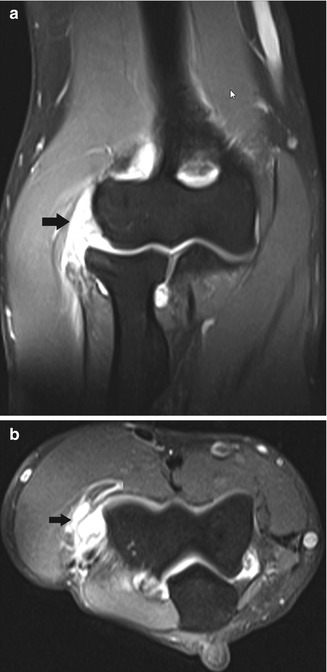
Fig. 19.17
Complete tear of the proximal insertion of the extensor tendons. (a) Coronal and (b) axial fat-suppressed T2-weighted MRI shows tendon discontinuity, as well as associated tearing of the lateral collateral ligament (arrow)
According to Sasaki et al., CT arthrography has a better sensitivity compared to MRI for evaluation of a capsular tear at the undersurface of the extensor carpi radialis brevis tendon in chronic tennis elbow (Sasaki et al. 2011).
In the absence of typical imaging features of lateral epicondylitis, the clinician should rule out an alternative etiology of lateral elbow pain. The differential diagnosis includes lateral collateral ligament injury, lateral fringe syndrome, occult radius fracture, osteochondrosis dissecans of the capitellum, Panner disease (Fig. 19.18), posterolateral rotatory instability, osteoarthritis, synovitis of the radiohumeral joint, and nerve entrapment syndromes such as radial tunnel syndrome (Fig. 19.19) (Naam and Nemani 2012; Walz et al. 2010; Kotnis et al. 2012). These entities are not specific to tennis players, and therefore further discussion is beyond the scope of this chapter.
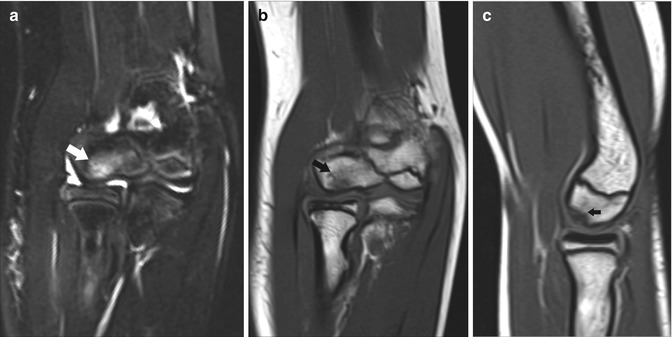
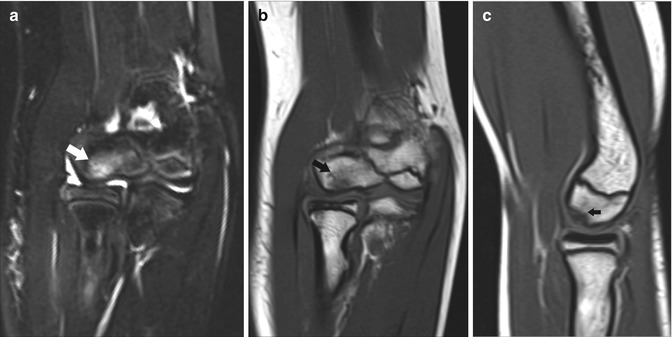
Fig. 19.18
A 10-year-old tennis player with Panner disease. (a) Coronal fat-suppressed T2-weighted MRI shows increased signal within the capitellum (arrow). (b) Coronal and (c) sagittal T1-weighted MRI demonstrates that the lesion within the capitellum is hypointense (arrow). The overlying cartilage remains intact
Fig. 19.19
Radial tunnel syndrome in a 32-year-old female tennis player. Axial FS T2-WI demonstrates high signal edema within the supinator muscle, in keeping with denervation edema (black arrow)
19.3.2 Medial Side Lesions
Medial epicondylitis is far less common than lateral epicondylitis. The disorder has been designated as “golfer’s elbow” but may be seen in other throwing and racquet sports, resulting in a chronic valgus overuse. It also occurs in the nonathletic population.
Patients typically present with medial elbow pain radiating into the forearm and a focal pressure tenderness 5–10 mm anterior and distal to the midportion of the medial epicondyle over the pronator teres and flexor carpi radialis (Frick and Murthy 2010).
The disorder usually involves the musculotendinous junctions of the flexor carpi radialis and pronator teres, but the other tendons of the flexor-pronator group including flexor carpi ulnaris, flexor digitorum superficialis, and palmaris longus may be involved in extensive lesions. Extensive disease may be associated with injury of the medial collateral ligament, particularly the anterior band (Frick and Murthy 2010; Park et al. 2008).
Imaging is not always essential in the initial evaluation of medial epicondylitis, but is particularly recommended when the clinical picture is unclear or with refractory cases (Walz et al. 2010).
Ultrasound and MRI characteristics are very similar to tendon disease at the lateral compartment. Ultrasound has a reported sensitivity of 95 % and specificity of 92 % for clinical medial epicondylitis (Park et al. 2008).
In the skeletally immature athlete, the medial epicondyle physis is weaker than the anterior band of the medial collateral ligament. Therefore, in youth tennis players presenting with medial elbow pain, one should consider a physeal injury, also known as “Little Leaguer’s elbow” (Fig. 19.20). MRI demonstrates physeal widening and surrounding edema (Frick and Murthy 2010).
Fig. 19.20
A young tennis player with an apophyseal avulsion fracture. Frontal radiograph of bilateral elbows shows avulsion of the apophysis of the medial epiphysis (white arrows) on the left side. The normal right side is shown for comparison (black arrow)
Other differential diagnoses of medial elbow pain in tennis players include medial collateral ligament injury (Fig. 19.21), occult fracture, osteochondrosis dissecans, osteoarthritis, flexor-pronator strain, and ulnar neuropathy (neuritis or entrapment). If there are signs of ulnar neuritis and medial instability, MRI is the preferred modality to detect nerve thickening, fascicular distortion, and increased fluid within the ulnar nerve at the cubital tunnel (Walz et al. 2010).


Fig. 19.21
A female tennis player with ulnar collateral ligament tear. Coronal fat-suppressed T2-weighted MRI shows discontinuity of the proximal insertion of the ulnar collateral ligament (arrow)
19.3.3 Anteriorly Located Lesions
19.3.3.1 Injuries to the Distal Biceps Tendon
Distal biceps tendinosis and rupture is relatively rare in athletes (Wenzke 2013).
The distal biceps tendon is anatomically complex and consists of a double bifurcated distal tendon insertion on the radial tuberosity and a third medial structure (lacertus fibrosus), which inserts onto the superficial aponeurosis of the flexor muscles (Tagliafico et al. 2010; Brasseur 2012).
Tendinosis is associated with chronic pain with insidious onset and progressive course.
Clinically, tendon tears often present with sharp pain, a popping sensation, bruising, and a prominence of the biceps muscle belly (“Popeye arm”).
Ultrasound examination of the distal biceps tendon is difficult owing to the curved course of the distal segment of the tendon. Various ultrasound approaches have been reported to overcome this problem (Brasseur 2012).
Tendinosis is characterized by tendon thickening, hypoechogenicity, and fibrillar disruption.
Tendon rupture can be complete (involving both tendon bundles) or partial (involving only one of the bundles). The degree of retraction depends on the integrity of the lacertus fibrosus. Even when complete rupture occurs, retraction does not occur if the lacertus fibrous is intact. The tendon stumps are enclosed in a sheath and appear swollen (Brasseur 2012). The reported sensitivity, specificity, and accuracy for differentiating full versus partial ruptures are 95 %, 71 %, and 91 %, respectively. The presence of posterior acoustic shadowing can be helpful by indicating a complete tear (Lobo Lda et al. 2013).
Tendinosis on MRI presents as tendon thickening and intermediate signal within the tendon on fluid-sensitive sequences (Fig. 19.22). In partial tears, peritendinous edema and intratendinous areas of high T2 signal are seen. In a complete tendon tear with associated lacertus fibrosus rupture, retraction occurs with intervening fluid between the retracted stump and the radial tuberosity (Wenzke 2013). To evaluate the distal biceps tendon, imaging with flexed elbow, abducted shoulder, and supinated forearm (FABS) may be particularly helpful (Figs. 19.23 and 19.24).
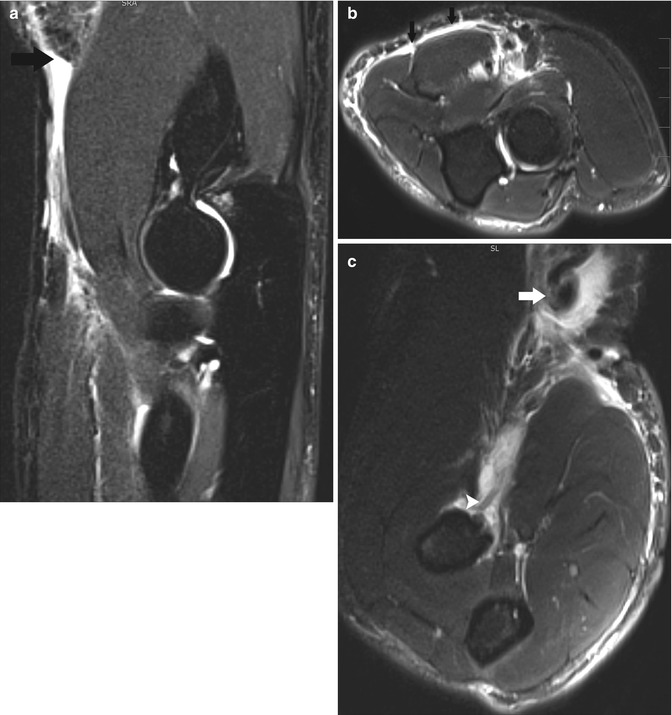
Fig. 19.22
A female recreational tennis player with distal biceps tendinosis. Axial fat-suppressed T2-weighted MRI shows thickening and intermediate signal within the distal biceps tendon (arrow)
Fig. 19.23
Partial tear of the distal biceps tendon. Fat-suppressed T2-weighted MRI in flexed abducted supinated (FABS) position shows marked thinning of the distal biceps tendon. There is still partial attachment of the tendon at the radial tuberosity (arrow)
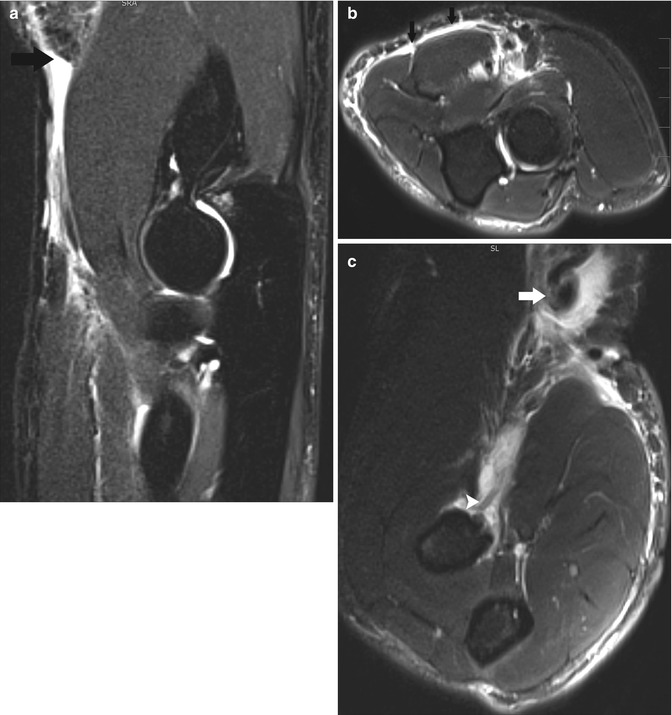
Fig. 19.24
A 35-year-old tennis player with a complete rupture of the distal biceps tendon. (a) Sagittal fat-suppressed T2-weighted MRI shows complete rupture of the distal biceps with marked retraction of the proximal tendon above the level of the elbow joint (black arrow). (b) Axial fat-suppressed T2-weighted MRI shows disruption of the lacertus fibrosus (arrows). (c) Fat-suppressed T2-weighted MRI in flexed abducted supinated (FABS) position confirms marked tendon retraction (arrow) and full-thickness tendon rupture. There is a small residual tendon stump at the radial tuberosity (arrowhead)
19.3.3.2 Bicipitoradial Bursitis
The bicipitoradial bursa lies posterior to the distal biceps tendon and anterior to the cortex of the radial tuberosity. Distention of the bursa frequently results from chronic repetitive trauma and may accompany tendinosis and tearing. Both ultrasound and MRI may be used to assess fluid accumulation into the bursa (Brasseur 2012; Wenzke 2013). After administration of contrast, there is enhancement of the synovial wall of the bursa (Fig. 19.25).
Fig. 19.25
A 55-year-old female recreational tennis player with bicipitoradial bursitis. Axial fat-suppressed contrast-enhanced T1-weighted MRI depicts distention of the bicipitoradial bursa with enhancement of its wall due to inflammation (arrow). The biceps tendon is indicated by an arrowhead
19.3.4 Posteriorly Located Lesions
19.3.4.1 Valgus Extension Overload Syndrome with Posterior Olecranon Impingement
Medial distraction and lateral compression in combination with elbow extension may lead to valgus overload syndrome. Repetitive rotatory forces at the olecranon may lead to olecranon osteophyte formation, which may ultimately fracture and result in intra-articular loose bodies (Ouellette et al. 2010).
19.3.4.2 Posterolateral Rotatory Instability
Tears of the ulnar band of the lateral collateral ligament may result in posterolateral rotatory instability. Posterior subluxation of the radial head may occur.
Clinically, patients present with pain, clicking, and apprehension when the elbow is in extension. MRI may show discontinuity and high T2 signal at the lateral ulnar collateral ligament in acute lesions, whereas diffuse thickening of the ligament and elongation and deformity of the sublime tubercle are seen in chronic lesions (Ouellette et al. 2010).
19.3.4.3 Triceps Tendon Rupture and Olecranon Bursitis, Stress Fractures of the Olecranon
Olecranon bursitis may occur in isolation or in association with distal triceps tears. Neither lesion is specific to tennis. Distal triceps tendon rupture is rare and may occur due to a fall on outstretched hand, a direct blow, or forced flexion during active extension.
Ultrasound is a quick and cost-effective technique for evaluation of fluid distention within the olecranon bursa (Fig. 19.26). On MRI, sagittal and axial fluid-sensitive sequences are best suited for evaluation of these lesions (Wenzke 2013). Olecranon stress fracture may be seen in tennis and is readily assessed on MRI as a hypointense line with surrounding bone marrow edema (Fig. 19.27) (Wenzke 2013).

Fig. 19.26
Olecranon bursitis. Transverse ultrasound image shows focal distention of the olecranon bursa (calipers and arrows) superficial to the olecranon (asterisk)

Fig. 19.27
Stress fracture of the olecranon. Sagittal T1-weighted MRI shows a hypointense fracture line (black arrow) at the olecranon
19.3.5 Cartilage Lesions and Osteochondral Lesions (OCL)
Repetitive compressive and valgus forces may cause cartilage lesions and osteochondral lesions (OCLs). These lesions may be seen in tennis but are more frequent in other (throwing) sports, such as baseball. OCLs occur usually at the capitellum but may rarely occur in the radial head or trochlea. MRI is the preferred imaging technique to evaluate subchondral bone marrow edema, bony fragmentation, chondral defects, and signs of instability. Fluid along the osteochondral fragment and the underlying defect may indicate instability. If there is absence of native joint fluid, CT or MR arthrography may be needed to demonstrate contrast extension deep to the osteochondral fragment (Wenzke 2013). In skeletally immature tennis players, repeated valgus and compressive force stress may compromise the blood supply to the capitellum, resulting in Panner disease. Radiographs show subchondral radiolucency in the capitellum. On MRI, there are bone marrow changes in the capitellum, but chondral defects are absent (Fig. 19.18) (Wenzke 2013).
19.4 Wrist and Hand
19.4.1 Lesions at the Ulnar Side of the Wrist
19.4.1.1 Extensor Carpi Ulnaris Lesions
Lesions of the extensor carpi ulnaris (ECU) tendon are the most frequent tendon lesions of the wrist encountered in tennis (Montalvan et al. 2006; Guerini et al. 2010).
Particularly in elite tennis players, ulnar wrist pain may be related to the increased use of the wrist to create top spin and double-handed backhand. In addition, higher string tension in professional racquets may increase the effect when the ball hits the racquet (Montalvan et al. 2006). ECU instability is not specific to tennis and may be seen in golfers (during downswing), in weight lifters, and in high-impact contact sports such as rugby.
Anatomically, the distal ECU tendon passes through a small osteofibrous tunnel, lying in an osseous groove between the head of the ulna and its articular process. The tendon inserts at the fifth metacarpal base.
The ECU is stabilized within the sixth extensor compartment by a duplication of the deep antebrachial fascia (ECU subsheath), which inserts on the osseous groove of the ulna. The dorsal (or extensor) retinaculum of the other five dorsal wrist compartments passes above this subsheath (Fig. 19.28). The dorsal retinaculum has no attachment to the ulna but inserts on the triquetrum and pisiform, allowing both pronation and supination (Montalvan et al. 2006). Due to this anatomical organization, the ECU moves less freely than the other extensor tendons and is prone to stress during pronation and supination. During pronation, the ECU lies on the inner surface of the distal ulna and has a direct course, distant from the extensor digiti minimi. During supination, the gap between the ECU and extensor digiti minimi narrows, and the ECU courses at an angle of approximately 30° to reach the fifth metacarpal and is submitted to maximal traction forces. During tennis play, the angle of the wrist constantly changes, predisposing to a high risk for trauma to the ECU subsheath. Once this stabilizing osteofibrous tunnel is ruptured or detached, ECU subluxation underneath the intact dorsal retinaculum may occur (Montalvan et al. 2006).
Fig. 19.28
Drawing shows the anatomy of the extensor carpi ulnaris (ECU). The ECU is stabilized within the sixth compartment by a subsheath (green), which inserts on the margins of the osseous groove of the ulna. The dorsal or extensor retinaculum of the other five dorsal wrist compartments passes above this subsheath (blue)
ECU lesions may be subdivided into three clinical entities, each with different imaging features.
Get Clinical Tree app for offline access

(a)
Traumatic ECU instability
This entity has a sudden onset, due to detachment or rupture of the ECU subsheath. In case of complete rupture, the tendon may leave its sheath, whereas in detachment, the tendon leaves the sheath during supination and recovers its normal position during pronation (Fig. 19.29).
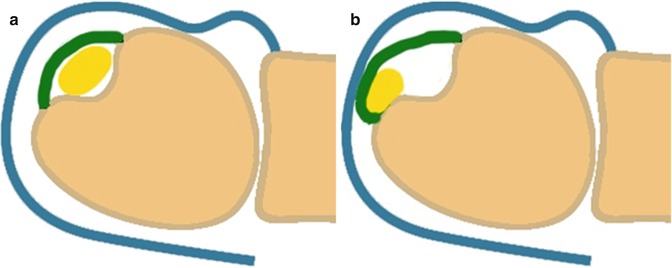
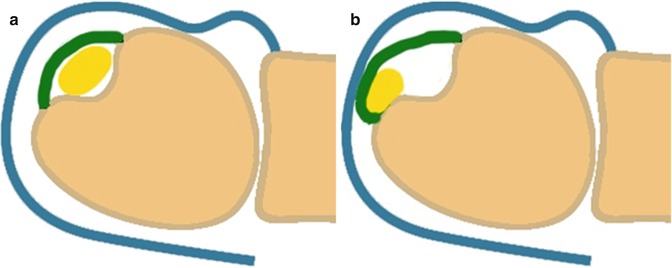
Fig. 19.29
Drawing shows traumatic instability due to detachment of the extensor carpi ulnaris (ECU) subsheath (green). (a) Normal position of the ECU tendon (yellow) in pronation. (b) During supination, medial subluxation of the ECU tendon (yellow) occurs underneath the subsheath (green)
Dynamic ultrasound is the preferred imaging technique to assess instability during pronation and supination. Detachment may be seen on ultrasound as a hypoechogenic pocket adjacent to the medial border of the ulna (Fig. 19.30).
Fig. 19.30
Traumatic extensor carpi ulnaris (ECU) instability due to detachment of the ECU subsheath. Transverse ultrasound image in supination shows medial subluxation of the ECU (arrow) out of the ulnar groove (asterisk). The ECU subsheath is thickened and there is a hypoechogenic pocket adjacent to the ECU tendon (arrowheads)
On MRI, this pocket of detachment is hyperintense on fat-suppressed T2-weighted images and enhances after administration of gadolinium contrast. Direct rupture of the ECU subsheath is more difficult to assess (Fig. 19.31).