Chapter 8 IMAGING OF THE ELBOW
MODALITIES
Ultrasound
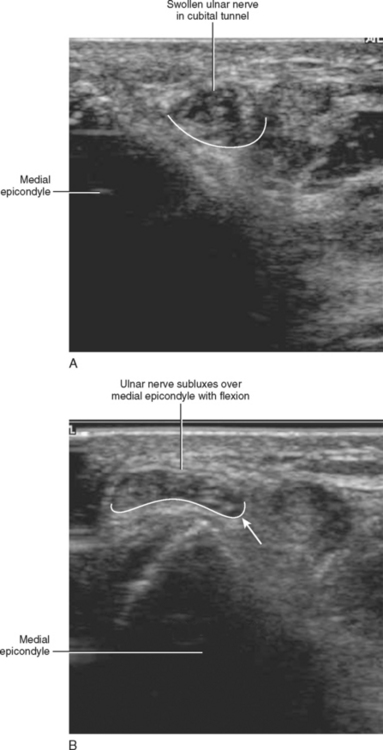
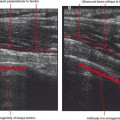
Ultrasound evaluation of the elbow is best used as a targeted examination to answer a particular question about a specific anatomic structure. The major advantage of ultrasound is that it can be used real-time to evaluate the dynamic status of anatomic structures such as subluxation of a tendon or nerve (Fig. 8-1) or in evaluating the severity of tendon or ligamentous injury. Major disadvantages include difficulty in evaluating the deeper structures of the elbow and inability to adequately assess the osseous structures. Also, it can be difficult for those who did not perform the examination to determine whether the study is accurate and complete.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is the most versatile and robust of imaging modalities available for the evaluation of the elbow and is capable of accurately depicting both soft tissue and osseous abnormalities. For instance, MRI can accurately depict the extent of soft tissue injury in a suspected biceps or triceps tendon rupture or tendinosis. It can also accurately depict the extent of tendon and ligamentous injury in a patient with signs of medial or lateral epicondylitis. MR imaging accurately depicts osseous abnormalities such as radiographically occult fractures and osteochondral injuries of the capitellum or the radial head. It can also accurately delineate intra-articular abnormalities, including synovial-based processes and intra-articular bodies.
Standard elbow imaging protocols typically include T2-weighted sequences with fat saturation in the axial, sagittal, and coronal imaging planes and short echo time sequences in both the sagittal and coronal planes. The anterior and posterior compartment structures are best evaluated using the sagittal and axial images, whereas the medial and lateral elbow structures are best depicted on coronal and axial images. The osseous structures should be evaluated using all available imaging planes to look for areas of marrow edema and cortical disruption. Direct or indirect MR arthrography is useful in grading osteochondral injuries and in depicting the presence of loose intra-articular bodies. MR arthrography may also be of some value in the evaluation of ligamentous structures of the elbow, particularly in depicting subtle partial-thickness articular-sided tears of the ulnar collateral ligament.
ANTERIOR COMPARTMENT ANATOMY AND INJURY PATTERNS
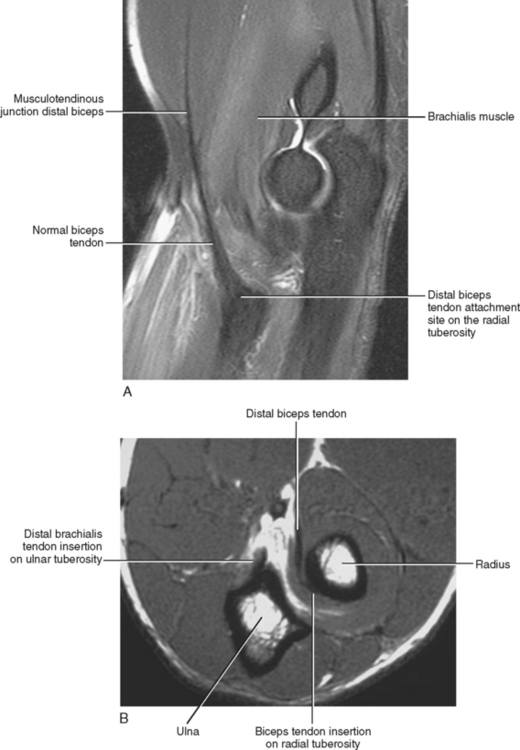
The biceps brachii and the brachialis are the two muscles located within the anterior compartment at the level of the elbow and are the main flexors of the elbow. The biceps brachii is composed of two separate heads. The short head originates on the coracoid process, and the long head originates on the superior glenoid tubercle. The two heads sit closely applied in the anterior compartment of the upper arm and do not merge but rather give rise to a common tendon at a level approximately 7 cm above the distal attachment on the radial tuberosity (Fig. 8-2). The bicipitoradial bursa separates the distal tendon from the adjacent radial tuberosity, and a broad medial expansion of the distal tendon referred to as the bicipital aponeurosis or lacertus fibrosus arises from the distal tendon and descends medially to cross the brachial artery and blend with the deep fascial layer that covers the origin of the common flexor muscle group. The brachialis muscle sits deep to the biceps brachii, originating along the distal aspect of the anterior surface of the humeral shaft. Distally, the brachialis muscle gives rise to a short thick tendon that inserts on the ulnar tuberosity.
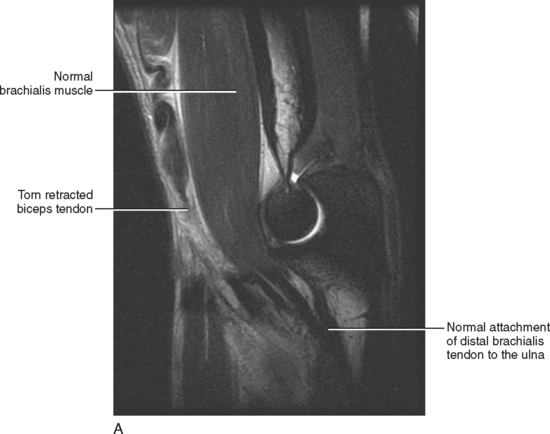
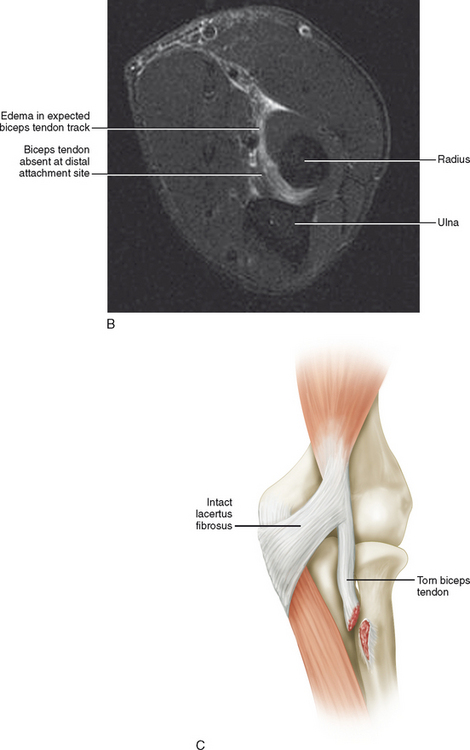
The individual usually describes a popping or tearing sensation and develops pain and ecchymosis in the region of the antecubital fossa. A complete tear leads to retraction of the musculotendinous junction of the biceps tendon, and on physical examination the distal biceps tendon is no longer palpable in the region of the antecubital fossa. The biceps muscle appears “bunched up” following retraction into the upper arm. The patient can still flex and supinate the arm because the brachialis and supinator muscles usually remain intact; however, both strength and endurance are markedly diminished. The lacertus fibrosus often remains partially or completely intact, thus preventing complete retraction of the distal biceps tendon. An intact lacertus fibrosus may help to mask the classic physical exam findings of a retracted muscle and tendon (Table 8-1).
Table 8-1 Distal Biceps Tendon Injuries
| Demographics | |
| Mechanism of injury | Axial loading with elbow flexed 90° |
| Tendon’s distal attachment site | Radial tuberosity |
| Injury pattern | Complete tear most common |
| MR evaluation | |
| T2 axial images | Complete versus incomplete tear |
| T2 sagittal images | Measure extent of tendon retraction |
| Pitfalls | |
| Lacertus fibrosus | May prevent retraction of torn tendon mimicking an incomplete tear |
| Bicipitoradial bursitis | Mimic of tendon pathology |
Radiography plays little to no role in the evaluation of a suspected distal biceps tendon tear or avulsion because there is usually no associated osseous avulsion fragment. Evaluation of the distal biceps tendon is best performed on sagittal and axial T2-weighted MR images through the elbow with fat saturation. A common problem that occurs is the ordering of an MRI of the upper arm (level of the humerus) to evaluate for a biceps tear, rather than correctly ordering an MRI of the elbow. Imaging through the level of the upper arm may not include the distal attachment site of the biceps tendon below the level of the elbow on the radial tuberosity.
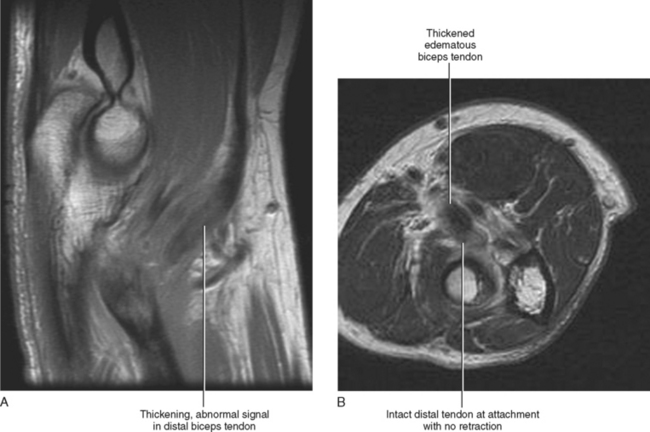
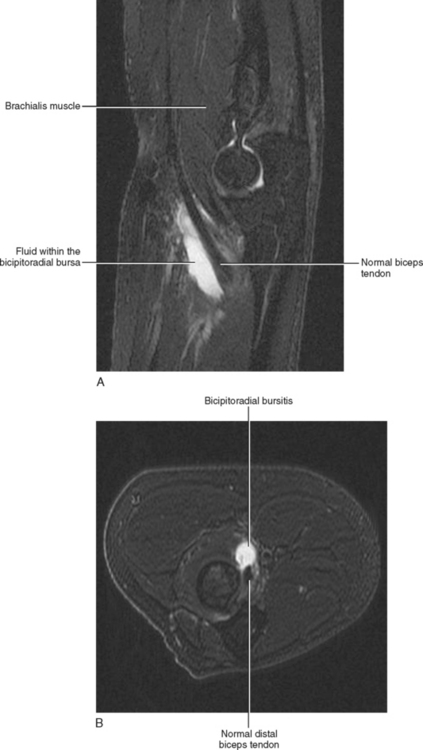
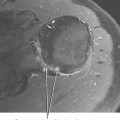
The role of MR imaging is to confirm the clinical suspicion of biceps tendon tear and to differentiate partial from complete disruption as well as to determine the extent of retraction of the torn tendon (see Table 8-1). Axial images are best suited for demonstrating complete disruption or avulsion at the level of the distal attachment, whereas sagittal images demonstrates the extent of musculotendinous retraction (Fig. 8-3). An intact lacertus fibrosus prevents proximal retraction of the disrupted biceps tendon, potentially masking a biceps tendon tear on physical examination and mimicking a partial-thickness tear on MRI. The key is to evaluate the distal insertion site of the biceps tendon using axial images to determine whether the distal tendon is completely avulsed or whether a portion of the distal tendon remains attached to the radial tuberosity. A partial-thickness tear is usually manifested on MR images as thickening or attenuation of the distal tendon with intrinsic signal alteration (Fig. 8-4), whereas a complete disruption with an intact lacertus fibrosus demonstrates a complete tear/avulsion distally with minimal or no significant retraction of the torn tendon. Bicipitoradial bursitis is often seen in association with pathology of the distal biceps tendon, and on MR imaging is manifested as an oval and somewhat lobulated fluid collection within the bursa immediately adjacent to the distal biceps tendon attachment site (Fig. 8-5). Fluid within the bursa should not be misinterpreted as a tear of the distal biceps tendon. However, bicipitoradial bursitis is often associated with a tear of the distal tendon, and fluid within the bursa should prompt a thorough evaluation of the distal tendon.
The brachialis tendon usually remains intact when the distal biceps tendon is torn; however, the distal brachialis muscle may occasionally demonstrate evidence of a mild (grade 1) muscle strain associated with a biceps tendon injury. Isolated injury of the brachialis muscle or tendon is uncommon; when injury or disruption of the brachialis muscle or tendon does occur, it is usually associated with a posterior or posterolateral dislocation of the elbow. After a posterior dislocation of the elbow, brachialis tendon injury may be seen in conjunction with the other soft tissue injuries including disruption of the posterior capsule, tear of the lateral ulnar collateral ligament, and injuries of both the common flexor and extensor tendons and muscle groups.
POSTERIOR COMPARTMENT ANATOMY AND INJURY PATTERNS
Tendinosis of the triceps tendon can occur as an isolated entity or in association with lateral epicondylitis or chronic olecranon bursitis. Isolated tendinitis usually occurs as the result of repeated forced extension of the elbow and is occasionally seen in weight-lifters. Full-thickness tears are very uncommon and usually result from eccentric overload during a fall on an outstretched hand. Direct trauma to the tendon or laceration is another potential source of disruption. Minimal trauma can lead to a tear when there is underlying weakening of the tendon from exogenous steroid use or in association with a collagen vascular disease. Tendinosis is usually treated with conservative measures and does not require surgery unless there is an associated extensive partial-thickness tear. Full-thickness disruption or avulsion of the triceps tendon is typically treated with a primary repair of the tendon and may require an allograft if there is extensive retraction or damage to the tendon (Table 8-2).
Table 8-2 Triceps Tendon Injury
| Demographics | |
| Mechanism of injury | |
| Injury pattern | |
| MR evaluation | T2 Sagittal and axial images |
| Pitfalls |
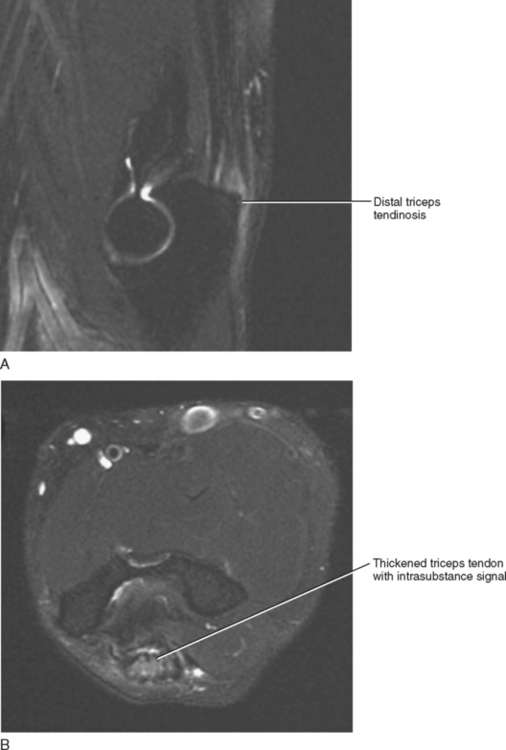
The triceps tendon is best evaluated on T2-weighted sagittal images, whereas T2-weighted axial images are complementary. The normal tendon demonstrates a striated appearance with longitudinal streaks of fibrofatty tissue interposed between the various tendon slips at the level of attachment to the posterior olecranon. MR evaluation of the elbow is typically accomplished with the elbow in full extension, and this may result in laxity or redundancy of the distal triceps tendon in turn resulting in a wavy appearance on sagittal images. These changes should not be misinterpreted as pathology of the distal tendon (Fig. 8-6). On MR imaging, tendinitis appears as thickening and increased signal within the distal triceps tendon, and there may be associated enthesiophyte formation and subcortical marrow edema at the distal attachment site on the olecranon (Fig. 8-7). Adjacent reactive soft tissue edema and occasionally fluid within the olecranon bursa may also accompany changes seen within the distal tendon.
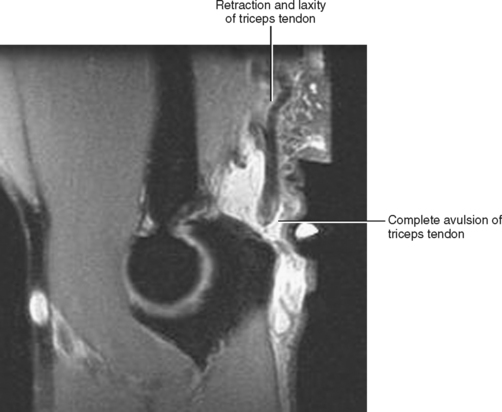
A partial-thickness tear demonstrates fluid signal within the expected location of the tendon, partial retraction, and thinning or attenuation of the tendon. A full-thickness tear shows complete disruption with a fluid-filled gap and retraction of the torn tendon end (Fig. 8-8). For purposes of surgical planning, it is important to describe the extent of retraction and the appearance or quality of the torn tendon end.
MEDIAL ELBOW ANATOMY AND INJURY PATTERNS
The flexor-pronator muscle group of the forearm has a common attachment on the medial epicondyle, which is typically referred to as the common flexor tendon. The ulnar collateral ligament (UCL) sits deep to the common flexor muscle group and consists of three separate components: the anterior, posterior, and transverse bundles. The anterior bundle of the UCL is the most important with regard to stability, protecting the elbow against excessive valgus load (Fig. 8-9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree