Chapter 14 IMAGING OF THE FOREFOOT AND MIDFOOT
MODALITIES
Ultrasound
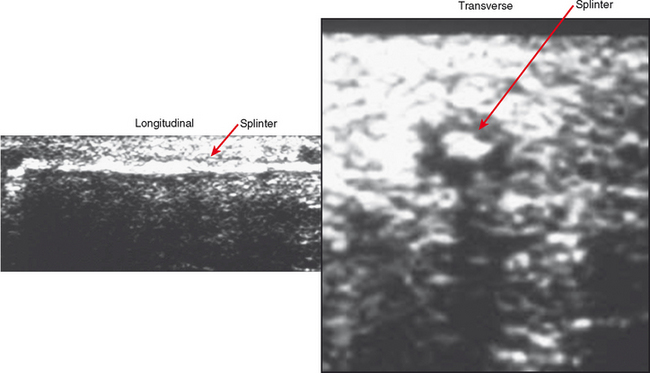
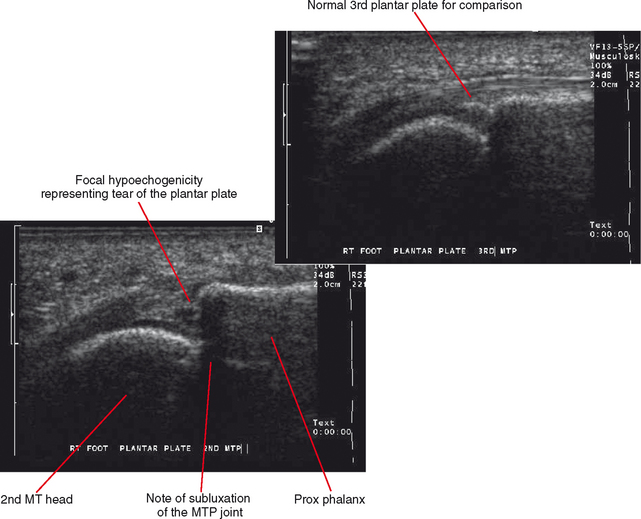
Ultrasound is excellent for answering specific clinical questions in many circumstances, especially regarding tendinopathy, foreign body localization (Fig. 14-1), ganglion and bursitis evaluation, Morton neuroma (Fig. 14-2), and ligament/plantar plate injury (Fig. 14-3). A distinct advantage of ultrasound is its ability to image while dynamically stressing a structure. Comparison can be made with adjacent normal regions or the contralateral side.
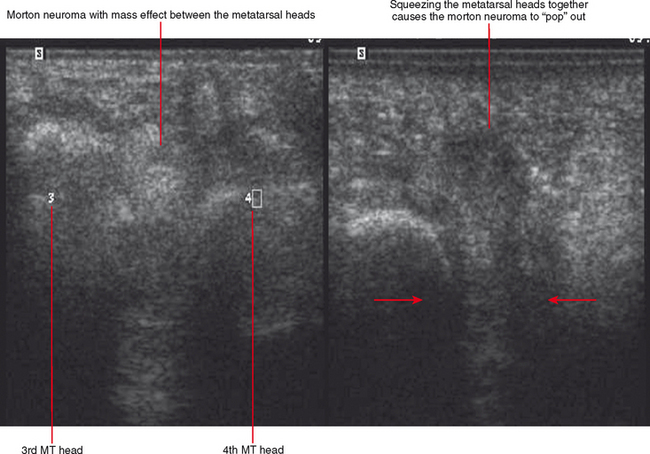
Figure 14-2 Morton neuroma in the third intermetatarsal space between the third and fourth metatarsal (MT) heads.
Magnetic Resonance Imaging
MRI is versatile and can be used to answer specific questions, such as ruling out plantar plate injury, or it can be used as a survey exam when the clinical picture is more nebulous. However, it is important to note that the ankle, midfoot, and forefoot are separate MRI exams, and unless there is a global problem such as extensive infection or reflex sympathetic dystrophy, these foot and ankle regions should not be mixed into one exam. Even a very experienced musculoskeletal radiologist can miss findings if the foot and ankle are imaged together with a large field of view.
MIDFOOT
Anatomy and Mechanics
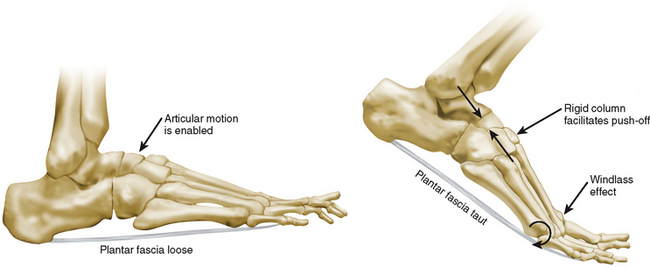
The midfoot is superbly constructed for ambulation. The tarsal bone articulations have capability of motion that allows for twisting of the foot and pronation/supination. However, during the push-off phase of walking, a stable midfoot column is more important than flexibility. This goal is achieved via the “windlass mechanism” (Fig. 14-4). A windlass is a mechanism commonly used on boats. It is a cylinder, which, when cranked, tightens a rope attached to a sail, anchor, and so on. The plantar fascia acts as a windlass of the foot. It is connected to the calcaneus and the digits. During the push-off phase of ambulation, dorsiflexion of the toes causes the plantar fascia to wrap around the metatarsal heads (i.e., the cylinder), which tightens the fascia, pulling the tarsal bones together and creating a stable column across the midfoot. Deformity of the arch or plantar fascia disruption, prevents this from working and can lead to pain with walking.
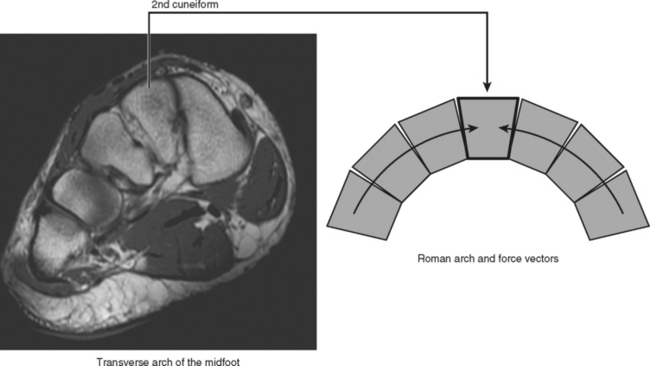
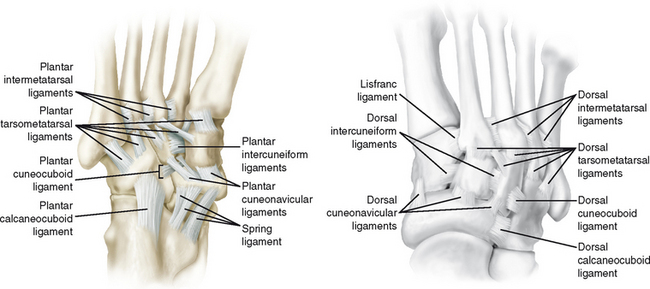
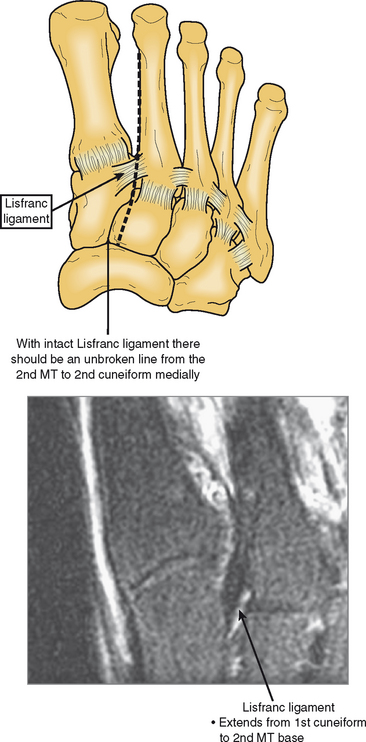
The Lisfranc joint is very important in stabilization of the midfoot and longitudinal arch. The second metatarsal base is inset compared with the other tarsometatarsal joints, and this and the middle cuneiform are shaped like a keystone in the coronal plane (Fig. 14-5). The Lisfranc joint is shaped like a Roman arch, which is well known for its stability. Lisfranc disruption may be seen after acute injury or in the setting of neuropathic disease. In either case, there is usually superior migration of the metatarsal bases and inferior excursion of the tarsal bones. This can create a rocker-bottom deformity with reversal of the longitudinal arch curvature (Fig. 14-6). Intercuneiform and intermetarsal ligaments exist in the midfoot (Figs. 14-7 and 14-8); however, the Lisfranc ligament, running obliquely from the medial cuneiform to the second metatarsal base (Fig. 14-9), is the main structure keeping the midfoot congruent—it is the cement of the Roman arch. There is no intermetatarsal ligament between the first and second metatarsals. Therefore, fracture of the second metatarsal base or disruption of the Lisfranc ligament creates instability of the entire tarsometatarsal axis, destabilizes the midfoot, and results in collapse of the longitudinal arch.
PATHOLOGY
Lisfranc Injury and Associated Pathology
Lisfranc injuries occur from twisting at the midfoot. The classic mechanism of falling from a horse with the foot twisted in the stirrup is not seen frequently. More commonly, the patient twists the foot in a pothole or lands wrong after a jump. More extensive injuries are associated with multitrauma patients as well. Lisfranc injuries are common in athletes and may be seen in sports that require pivoting, or when another player steps on their foot immobilizing the forefoot as the body rotates around the midfoot. Clinically, the injury is very painful and patients cannot bear weight on the affected extremity. Therefore, the diagnosis is usually suspected before imaging. If imaging is indeterminate, patients may undergo examination under anesthesia to demonstrate abnormal motion at the Lisfranc joint and widening of the ligament interval under stress.
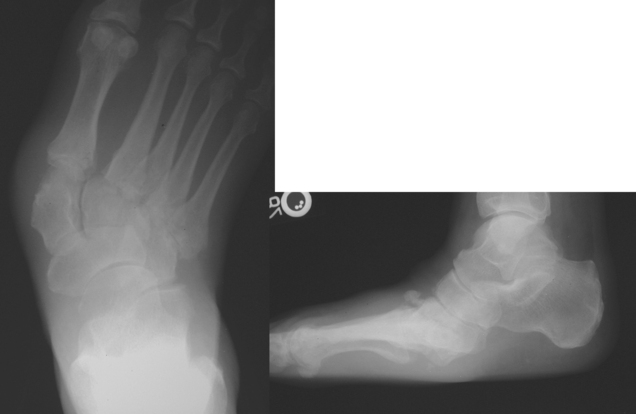
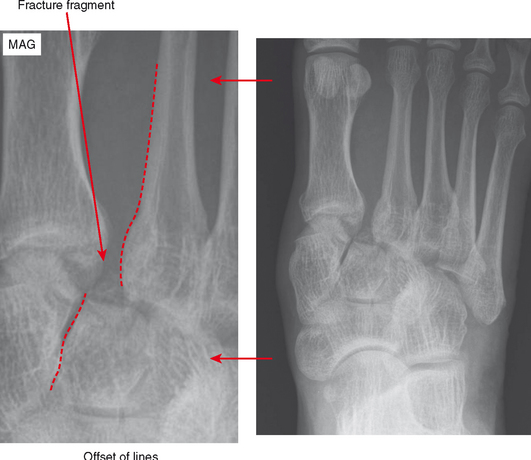
When Lisfranc injury is suspected, radiographs are the best initial examination. On the anteroposterior view of the foot, the medial margin of the second metatarsal should line up exactly with the second cuneiform (Fig. 14-10). The first tarsometatarsal joint should also be congruent. Distance between the first and second metatarsal bases is of less importance, and can vary; widening can occur in the presence of an os intermetatarseum, and can result in a false-positive diagnosis. Unlike true Lisfranc ligament avulsions, this ossicle is rounded and projects superiorly on the lateral view. Avulsions are very thin, linear, and positioned between the first cuneiform and the second metatarsal base. CT may be needed to confirm the finding (Fig. 14-11). If an injury is detected radiographically, CT is typically required to evaluate the extent of fractures, which is characteristically underestimated on radiographs. MRI is an excellent test to directly evaluate the Lisfranc ligament and other ligaments of the midfoot as well as to diagnose associated fractures and bone bruises, often obviating the need for examination under anesthesia. The best plane is axial (long axis); the best sequence is T2-weighted with fat suppression.
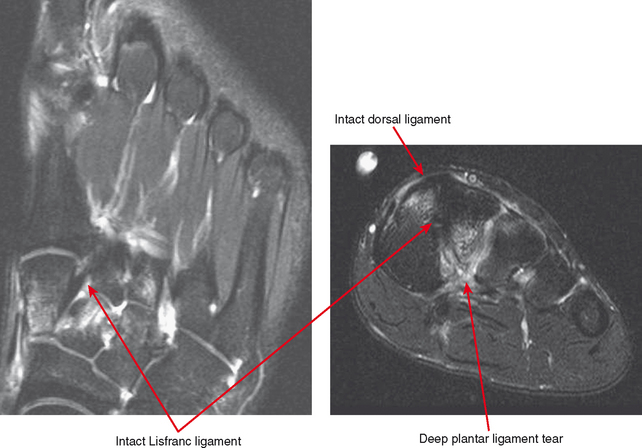
An important concept in interpreting an MRI of suspected Lisfranc ligament injury is that a ligament with a mechanically significant injury may still appear intact on MRI. First, small avulsions can be very hard to detect on MRI; second, the ligament may be stretched and insufficient without appearing discontinuous. In the setting of injury, any edema in or around the ligament should be considered suspicious for a significant injury. Secondary signs are also very useful. A very common association is bone bruise or fracture of the inferior aspect of the middle cuneiform or second metatarsal base (Fig. 14-12). In more severe injuries, bone bruises or fractures are also observed in various other tarsal bones and metatarsal bases. Another secondary sign is soft tissue edema extending distally along the second metatarsal shaft, frequently with strain of the first interosseous muscle between the first and second metatarsals (Fig. 14-13). Resultant feathery edema in the muscle is not significant by itself but is a sign of traumatic separation of the metatarsals. It is helpful to surgeons to identify other ligaments that are injured, such as the intercuneiform ligaments, the intermetatarsal ligaments, and the deep plantar ligaments of the midfoot. The intercuneiform ligaments and intermetatarsal ligaments are somewhat variable and are best evaluated on axial (long-axis) images but are not consistently seen on routine MRI (see Fig. 14-8). The deep plantar ligaments are best seen on coronal (short-axis) images (Fig. 14-14), just inferior to the tarsal bones and just deep to the peroneus longus tendon as it courses toward the first metatarsal base. However, prominent veins in this region make it difficult to detect soft tissue edema.
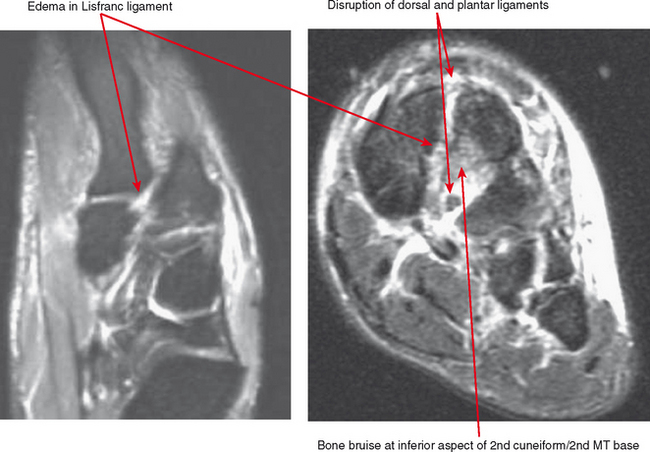
Figure 14-12 Lisfranc ligament tear. Classic signs on MRI; axial and coronal T2-weighted fat-suppressed images.
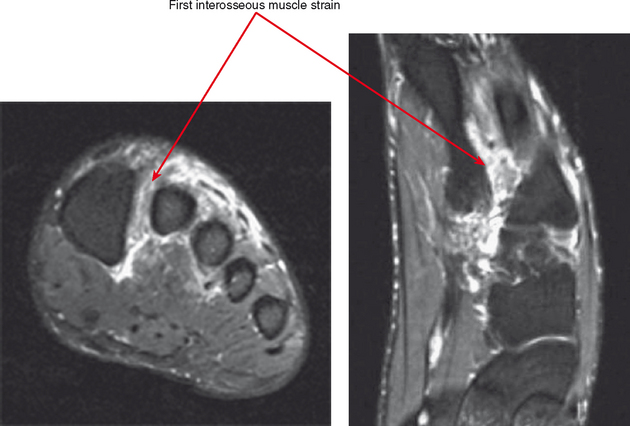
Figure 14-13 Lisfranc injury on MRI. First interosseous muscle strain is another common association.
FOREFOOT
Anatomy
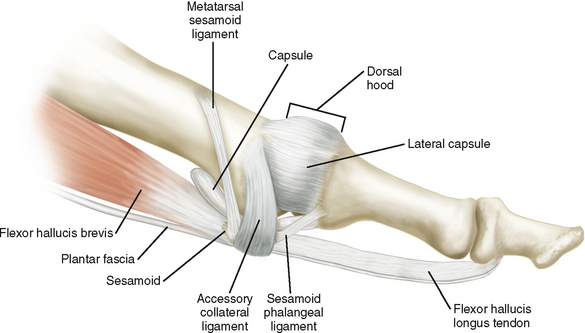
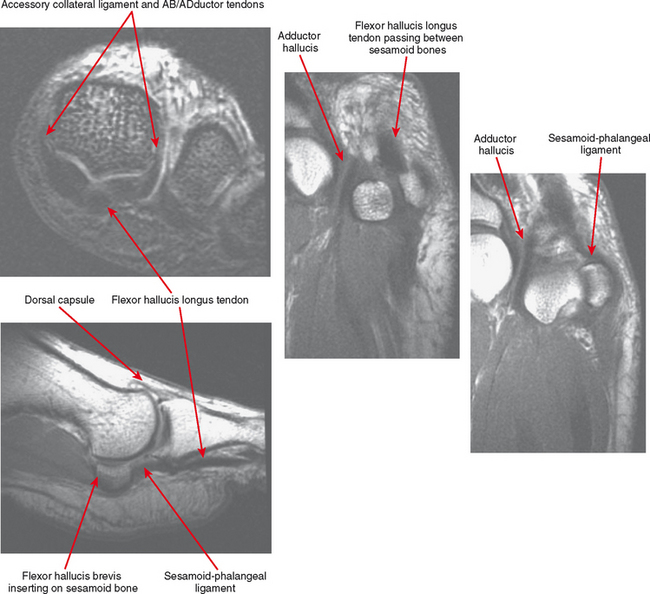
The medial (tibial) and lateral (fibular) sesamoid bones articulate on facets at the inferior aspect of the first metatarsal head. Facets are separated by a bony prominence called the “crista” (Figs. 14-15 and Figs. 14-16). Articular cartilage is present on the metatarsal head and the sesamoids (the metatarsal-sesamoid, or MTS joint), and synovial fluid communicates with the rest of the first metatarsophalangeal (MTP) joint. Processes that alter the position or tracking of the sesamoids or that result in cartilage loss can cause pain and secondary osteoarthritis. Any articular disease affecting the first MTP joint also affects the MTS joint. The sesamoid bones are stabilized by their capsular location and metatarsal articulation. Additional stabilization is provided by an intersesamoid ligament that extends between them as well as sesamoid-phalangeal ligaments distally. However, this stable position under the first metatarsal head also makes the sesamoid bones—especially the tibial sesamoid—susceptible to compressive force. Loss or migration of the plantar fat pad from callus, from diseases such as rheumatoid arthritis and diabetes, or from excessive dorsiflexion (i.e., high-heeled shoes) can leave the sesamoid bones relatively unprotected. The sesamoid bones are also part of the flexor complex of the first ray. The flexor hallucis longus tendon passes between the sesamoids, superficial to the intersesamoid ligament. Separate slips of the flexor hallucis brevis tendon insert on the tibial and fibular sesamoid bones. The sesamoid bones are also intimately associated with the capsule near the attachment of the tendons of the abductor hallucis (adjacent to the tibial sesamoid) and the adductor hallucis (adjacent to the fibular sesamoid).
The structures just described make up the plantar plate of the first MTP joint. The lesser MTP joints (second through fifth) also have plantar plates, composed of thickening of the inferior joint capsule. This thickened, fibrous capsule makes a dark U-shaped structure on coronal (short-axis) MR images when intact (Fig. 14-17). Flexor and extensor tendons pass by the MTP joints inferiorly and superiorly, on course to insert onto the phalanges. Between the metatarsal heads there is an anatomic bursa called the intermetarsal bursa, which can fill with fluid. On coronal T2-weighted images, it is seen as a third line of fluid between the bones (joint, bursa, joint), separated by the adjacent joint capsules (see Fig. 14-17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree