Chapter 10 IMAGING OF THE HAND AND FINGERS
SOFT TISSUE ANATOMY AND INJURY PATTERNS
Metacarpophalangeal Joint
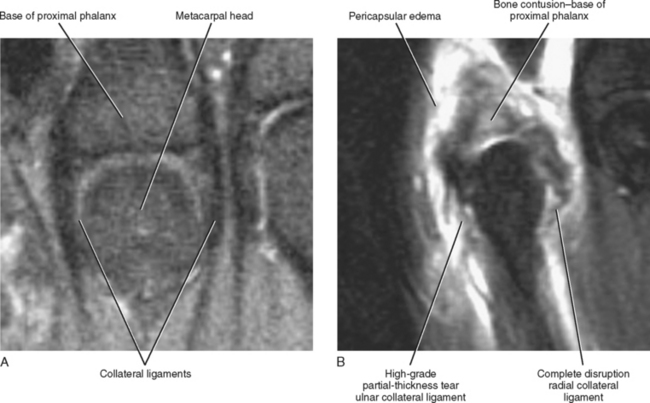
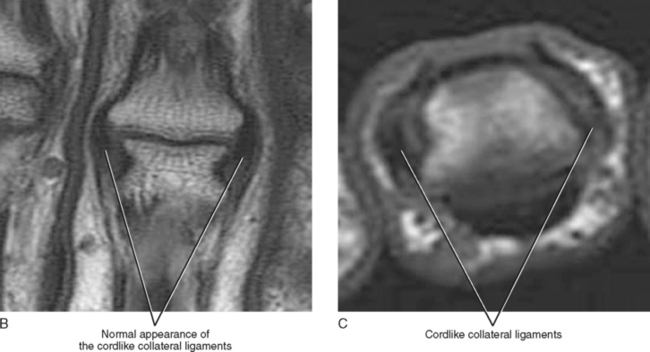
The metacarpophalangeal joints each have a strong fibrous capsule that is composed of two cord-like collateral ligaments and a thickened volar component referred to as the volar plate (Fig. 10-1A). The second through fifth metacarpal heads are also stabilized in the coronal plane by deep transverse metacarpal ligaments. These ligaments extend along the volar aspect of the metacarpophalangeal joints connecting the volar plates of adjacent metacarpophalangeal joints and have also been referred to as the “intervolar plate ligaments.” The dorsal aspect of the joint is stabilized primarily by the extensor “hood” and the extensor tendon. This complex capsular anatomy provides tremendous stability at the level of the second through fifth metacarpophalangeal joints, and, as a result, complete dislocation at this level is uncommon.
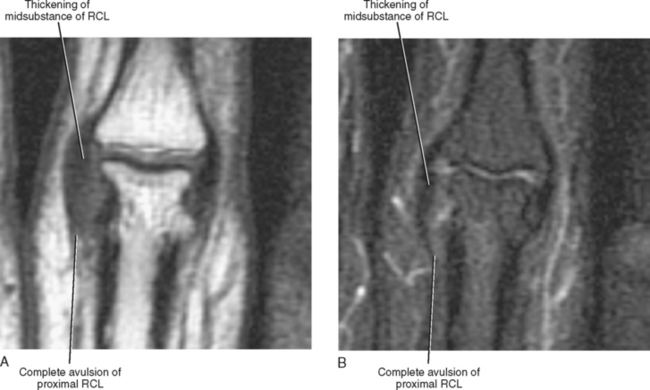
Although full-blown medial or lateral dislocation of the metacarpophalangeal joint only rarely occurs, valgus or varus stress injuries can result in a sprain or disruption of the collateral ligaments. Injuries to the collateral ligaments are described either as a sprain (thickening of the collateral ligament with adjacent soft tissue edema) or as a partial- or full-thickness disruption (Fig. 10-1B). Acute injuries show extensive pericapsular soft tissue edema, whereas chronic injuries demonstrate thickening but lack the associated soft tissue edema. Bone contusions are often seen accompanying capsular injuries and usually result from the impaction of two bones at the time of injury. They may indicate subluxation or dislocation at the time of injury. Contusions may be accompanied by small cortical avulsion fractures, which occur at the level of attachment of the collateral ligament. Bone contusions are best depicted on fat-suppressed T2-weighted images, whereas avulsion fractures are best seen on T1-weighted images without fat saturation or gradient-echo images and may require evaluation with radiographs for detection.
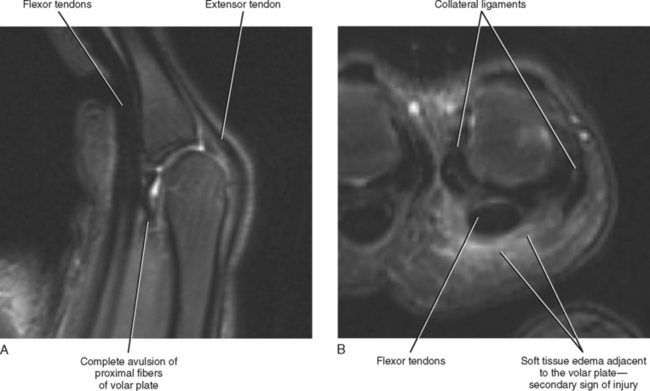
Volar plate injury can result from a significant hyperextension injury or from either a dorsal or volar dislocation of the metacarpophalangeal joint. After reduction, MRI can accurately delineate the status of the volar plate, which usually remains intact at its distal attachment site, with most injuries occurring near the proximal attachment site (Fig. 10-2). Injuries range from a mild sprain to complete disruption or avulsion, and the volar plate may become entrapped within the metacarpophalangeal joint, resulting in an incomplete reduction or preventing full range of motion after reduction. Volar plate injuries are described as either a partial or complete disruption. Intra-articular entrapment of a portion of the volar plate should also be noted. Volar plate injuries of the metacarpophalangeal joint are often accompanied by a fracture of the volar aspect involving the articular surface at the base of the proximal phalanx, which typically occurs at the time of dorsal dislocation. The size of the fragment and the congruence of the articular surface should be described. A fracture that involves more than 50% of the articular surface or demonstrates significant articular surface step-off usually requires open reduction and fixation.
Interphalangeal Joint
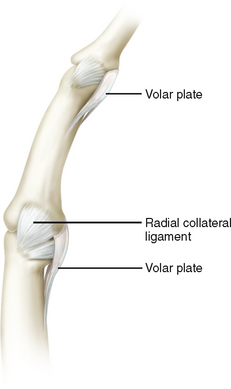
The capsular anatomy of the interphalangeal joint is very similar to that of the metacarpophalangeal joint. There is a strong fibrous capsule that is composed of medial and lateral collateral ligaments and a strong thickened volar component referred to as the volar plate (Figs. 10-3 and 10-4). The extensor apparatus including the extensor tendon and its numerous attachments provides the major support along the dorsal aspect of the interphalangeal joint.
Collateral ligament injuries result from excessive valgus or varus force and are described as a sprain, seen as capsular thickening and adjacent edema, or as a partial- or full-thickness tear or avulsion. Small avulsion fractures can occur at either the proximal or the distal attachment site (Fig. 10-5).
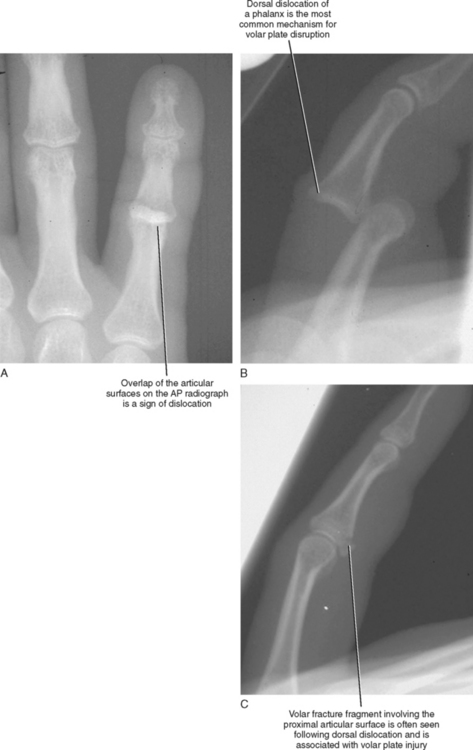
Dorsal dislocation of an interphalangeal joint is such a common injury across the entire array of athletic pursuits that it has been referred to as “coach’s finger.” Dorsal dislocations occur most commonly at the level of the proximal interphalangeal joint but also occur at the distal interphalangeal joint (Fig. 10-6). Dorsal dislocation can result in an injury to the volar plate and is often associated with a fracture of the volar aspect of the base of the dislocated phalanx (Fig. 10-6C). Fractures/dislocations are usually treated with dorsal splinting, with the interphalangeal joint in mild flexion to allow healing of the fracture and injured soft tissue structures. Fractures that involve more than 50% of the articular surface of the base of the dislocated phalanx are considered unstable and require open fixation.
Flexor Tendons and Pulley System
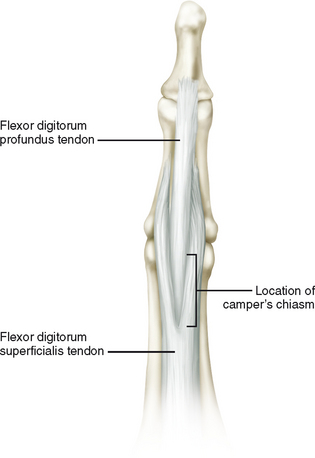
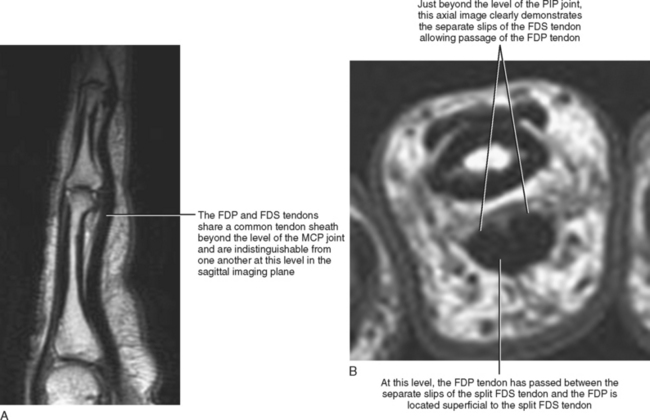
Flexion of the second through fifth digits is accomplished by the combined action of two tendons, the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP). The two flexor tendons travel together with the FDP tendon located just deep to the FDS tendon as they exit the carpal tunnel at the level of the wrist and enter the hand. The tendons then enter a common digital flexor tendon sheath at the level of the metacarpophalangeal joint. Prior to the level of the proximal interphalangeal joint, the flexor superficialis tendon splits into two slips and allows passage of the flexor profundus tendon, which becomes superficial at this level. The separate tendon slips of the superficialis tendon then reunite deep to the profundus and insert as radial and ulnar slips onto the palmar aspect of the base of the middle phalanx. This normal splitting and reuniting or decussation of the FDS tendon to allow passage of the FDP tendon has been referred to as the camper’s chiasm (Fig. 10-7). After passing through the decussation, the FDP tendon continues distally to attach on the base of the distal phalanx. This anatomic configuration allows the FDS tendon to control flexion of the proximal interphalangeal joint, while the FDP tendon controls flexion at the level of the distal interphalangeal joint (Fig. 10-8).
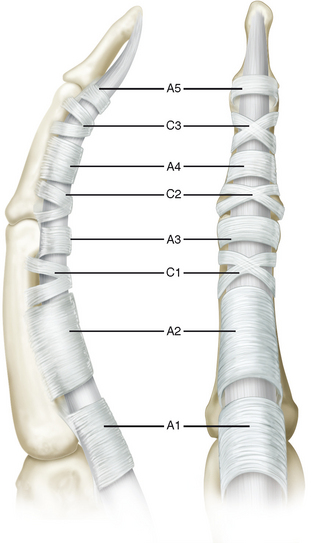
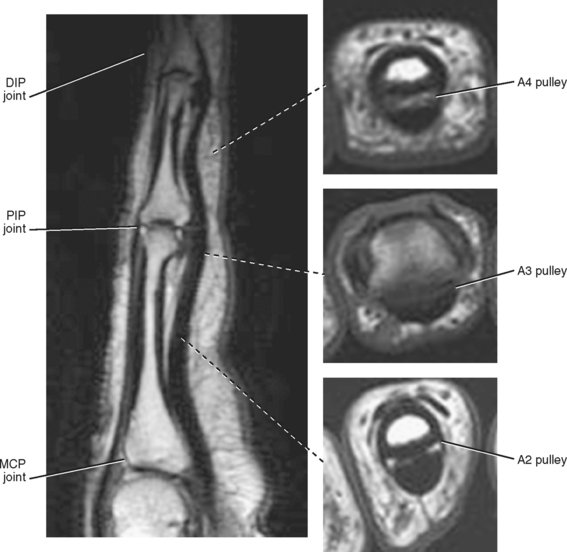
A complex system of fibrous bands or retinacular sheaths, referred to as “pulleys” is responsible for maintaining the proper position of the flexor tendons firmly against the volar aspect of the phalanges and prevents “bowstringing” of the tendons during flexion of the finger. The pulley system is composed of five annular and three cruciate pulleys. The annular pulleys (primarily A2 and A4) are vital for normal digital function (Fig. 10-9). They prevent tendon bowstringing and also ensure optimal joint flexion for a given amount of tendon excursion. The cruciate pulleys are primarily responsible for maintaining the proper flexibility of the tendon sheath, thus allowing the sheath to conform to the various shapes required for normal digital flexion. The cruciate pulleys also allow access of the digital arteries, which provide the tendon blood supply (Fig. 10-10).
The range of abnormalities involving the flexor tendons includes tenosynovitis of the tendon sheath, which may be sterile or infectious. Sterile tenosynovitis often results from repetitive trauma or can be associated with inflammatory arthropathies such as rheumatoid arthritis. Infectious tenosynovitis is most commonly bacterial in origin but may result from an atypical infectious agent such as mycobacterium. Infectious tenosynovitis is most often associated with a history of penetrating trauma, usually a punch to the mouth. Tendinopathy represents a degenerative process of the tendon that may be age-related or may result from repetitive trauma. Finally, a partial- or full-thickness tear of the tendon may occur. Flexor tendon tears most commonly result from a laceration. Closed tears, though less common, have been shown to be associated with rheumatoid arthritis, osteoarthritis, scaphoid nonunion, Kienböck disease, hook-of-the-hamate fracture, and carpal dislocation. Closed flexor tendon injuries can also result from sudden extension of a flexed joint, and these injuries are commonly seen in rugby and football participants.
On MRI, tenosynovitis manifests as fluid contained within the tendon sheath and a peritendinous edema of the involved tendon, and it is best demonstrated on axial T2-weighted images (Fig. 10-11). The tendon maintains normal morphology and intrinsic signal. Tenosynovitis may involve a single or multiple adjacent tendon sheaths and is typically graded as mild, moderate, or severe based on the quantity of fluid within the sheath. Ultrasound also demonstrates thickening of the sheath and fluid within the sheath, and power Doppler demonstrates increased flow and hyperemia of the surrounding soft tissues (Fig. 10-12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree