Chapter 9 IMAGING OF THE WRIST
MODALITIES
Ultrasound
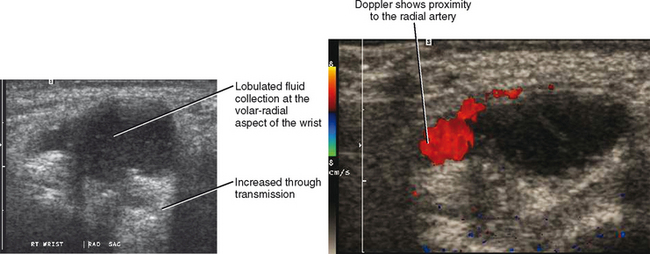
Ultrasound evaluation of the wrist is primarily reserved for special targeted exams to answer a specific question. This includes but is not limited to the evaluation of masses such as ganglia, aneurysms, foreign body localization, and other soft tissue masses (Fig. 9-1). Abnormalities of the tendon including tenosynovitis, tendinopathy, and partial- or fullthickness tears can also be depicted with ultrasound. Dynamic imaging can also depict subluxation of tendons.
TENDONS
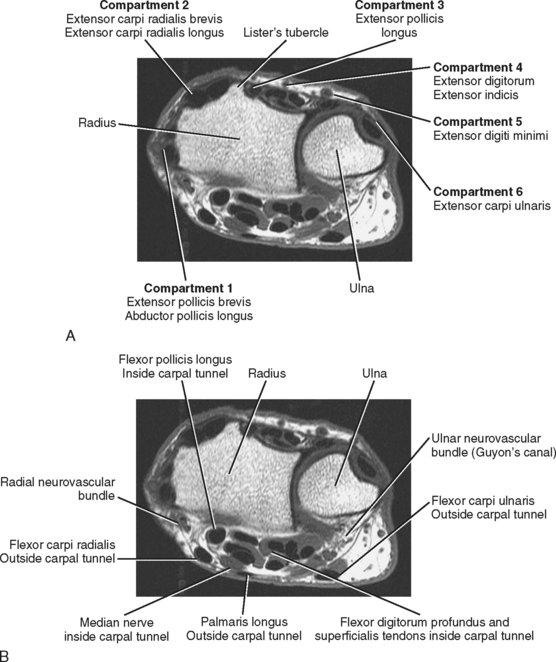
At the level of the wrist, the tendons are broadly classified as either flexor or extensor tendons. The extensor tendons are located along the dorsal aspect of the wrist and are arranged in six separate compartments (numbered one through six) with the first compartment located along the radial aspect of the wrist and the sixth compartment located along the ulnar side of the wrist (Fig. 9-2A). The number of tendons varies within the six compartments, but each compartment contains only a single common tendon sheath, which is shared by all tendons within that compartment (Table 9-1). The flexor tendons are divided into two separate groups based on whether they are located within or outside of the carpal tunnel (Fig. 9-2B and Table 9-2).
Table 9-1 Extensor Compartment Anatomy
| Compartment | Tendons |
|---|---|
| 1 | |
| 2 | |
| 3 | Extensor pollicis longus (proximal to the radioulnar joint) |
| 4 | |
| 5 | Extensor digiti minimi tendon |
| 6 | Extensor carpi ulnaris tendon |
Table 9-2 Flexor Compartment Anatomy
| Compartment | Anatomic Structures |
|---|---|
| Inside carpal tunnel | |
| Outside carpal tunnel | |
| Inside Guyon’s canal | Ulnar artery and nerve |
The range of tendon pathology in the wrist is similar to the range of pathology found in tendons elsewhere in the body. Inflammation isolated to the tendon sheath is referred to as tenosynovitis and may be sterile or infectious (Fig. 9-3). Noninfectious tenosynovitis is most common and typically results from repetitive trauma or mechanical irritation of the tendon sheath but may also occur in association with an inflammatory arthropathy. Tenosynovitis usually leads to the accumulation of fluid and/or synovial proliferation within the tendon sheath and may occasionally be associated with scarring within the tendon sheath. Scarring or fibrosis within the tendon sheath is referred to as stenosing tenosynovitis and may lead to entrapment and loss of function of the tendon. When this occurs at the level of the distal hand or fingers, it may lead to trigger finger.
The compartmental anatomy of the tendons of the wrist makes the axial image at the level of Lister’s tubercle best suited for identifying a specific tendon. As a result, tendon anatomy and pathology are usually best depicted on axial MR images, whereas coronal and sagittal images are complementary. The use of fat saturation increases the conspicuity of abnormalities such as minimal fluid within a tendon sheath and subtle surrounding soft tissue edema. Although frequency-selective fat saturation is the preferred method on a high field strength system, STIR (short tau inversion recovery) imaging can be substituted when frequency-selective fat-saturation techniques produce inhomogeneous fat saturation or when using a low field strength magnet. On MRI, the normal tendon typically demonstrates homogeneous low signal. Each tendon, however, is composed of multiple bundles, and on occasion this anatomic configuration can result in intermediate striations within the substance of the tendon, which can mimic tendinosis or an interstitial tear of the tendon. The normal tendon, however, lacks other signs of inflammation such as tenosynovitis and adjacent reactive soft tissue edema.
Tenosynovitis involving the first extensor compartment at the level of the wrist is referred to as de Quervain disease (Fig. 9-4). The first extensor compartment contains the extensor pollicis brevis and the abductor pollicis longus tendons, and inflammatory changes of this compartment typically result from chronic microtrauma associated with repetitive ulnar and radial deviation of the wrist. There appears to be an increased incidence of de Quervain disease in young women during the third trimester of pregnancy and in the early postpartum period. Postpartum de Quervain disease may be associated with breast-feeding, and speculation has been made that the increased incidence in these young women results from the position of the wrist while feeding or possibly carrying the young infant. Patients with de Quervain’s disease usually present with pain and swelling over the radial aspect of the wrist at the level of the radial styloid, and there is usually little confusion regarding the diagnosis on the basis of clinical examination. On MRI, changes within the tendon sheath may include tenosynovitis, stenosing tenosynovitis, and tendinopathy. Reactive marrow edema within the underlying radial styloid is a common finding seen best on fat-suppressed T2-weighted MR images.
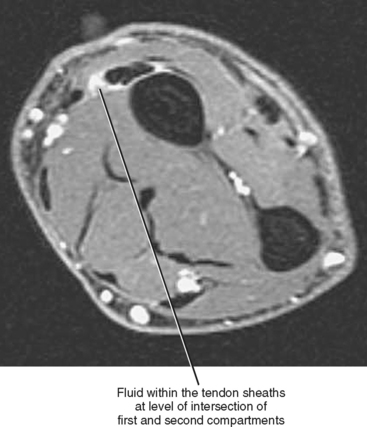
Intersection syndrome refers to a tenosynovitis that occurs in the distal forearm at the crossing levels of the first and second extensor compartments. This condition most often results from chronic overuse and has been associated with rowing and racquet sports. Intersection syndrome is common in helicopter skiing and in aggressive downhill alpine skiing (in up to 11% of participants); in this setting intersection syndrome has also been referred to as bugaboo forearm. The mechanism of injury in this subset of patients is likely repetitive dorsiflexion and radial deviation of the wrist against the resistance of deep snow on withdrawal of the planted ski pole. The extensor pollicis brevis and abductor pollicis longus tendons cross over the second extensor compartment tendons and the extensor carpi radialis longus and brevis tendons at a level approximately 4 to 5 cm proximal to the radiocarpal joint. At the point of crossover, repetitive friction can lead to tenosynovitis, stenosing tenosynovitis, and occasionally adventitial bursa formation. On MRI, intersection syndrome is manifested as fluid within and surrounding the two tendon sheaths at the point of crossover (Fig. 9-5). The primary differential diagnosis is that of de Quervain disease. Decussation syndrome refers to a friction tenosynovitis caused by the third compartment tendons crossing superficial to the second compartment tendons.
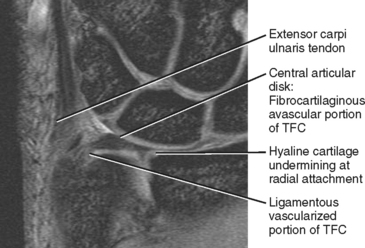
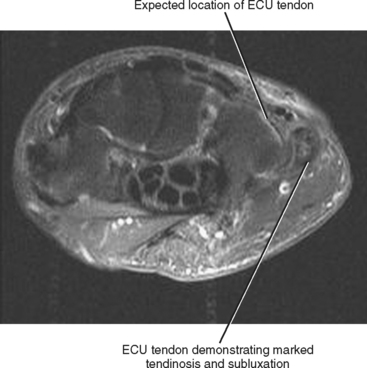
Extensor carpi ulnaris tenosynovitis is also common and often results from excessive repetitive ulnar deviation as occurs in racquet sports. The extensor carpi ulnaris tendon sheath is considered to be a part of the triangular fibrocartilage complex (TFC; see Fig. 9-16), and injuries of the TFC are often accompanied by abnormalities of the extensor carpi ulnaris tendon. As a result, MRI evidence of extensor carpi ulnaris tenosynovitis/tendinosis should prompt a thorough evaluation of the TFC and especially its peripheral attachment for evidence of injury or tear. Extensor carpi ulnaris tendinopathy and tenosynovitis can mimic other ulnar-sided wrist abnormalities such as injury of the triangular fibrocartilage, lunotriquetral ligament tear, or one of the ulnar-sided abutment syndromes. MRI can be useful in differentiating these various entities. Traumatic injury of the extensor carpi ulnaris tendon sheath at the level of the distal ulna can result in tendon instability and recurrent dislocation (Fig. 9-6). Dislocation of the extensor carpi ulnaris tendon often accompanies tenosynovitis and may require dynamic MRI of the wrist or axial MRI of the wrist in the pronated and supinated positions to correctly establish this diagnosis. Subluxation of the extensor carpi ulnaris tendon can result in ulnar wrist pain accompanied by reproducible snapping sensation during wrist motion. Ultrasound is uniquely suited for the evaluation of recurrent subluxation of the extensor carpi ulnaris tendon because a dynamic exam can demonstrate the change in position of the tendon during motion of the wrist (Fig. 9-7).
Laceration or penetrating trauma to the wrist is a common cause of tendon disruption. Closed tears can also occur and are often attritional in etiology, occurring in association with inflammatory processes such as rheumatoid arthritis or occurring secondary to changes in the underlying osseous anatomy, as occurs after carpal fracture or dislocation. A complete description of a tendon tear should include the extent of tear as partial or complete. The location of the torn tendon end is usually described as it relates to the adjacent osseous anatomy. When a full-thickness tear is identified, it is important to accurately describe the length of the gap between the tendon ends. A gap of more than 3 cm often requires a tendon graft for adequate repair. Finally, the integrity of adjacent tendons should be described, since injuries often involve neighboring tendons.
Pitfalls of Tendon Pathology
Several known MRI pitfalls can obscure or mimic tendon pathology at the level of the wrist. Inhomogeneous or failed fat saturation is a common problem that may decrease the conspicuity of fluid located within or surrounding a tendon sheath. Inadequate fat saturation is more likely to occur when the wrist is imaged by the patient’s side, which places the wrist out of the isocenter of the magnet. Recognition of failed fat saturation should be remedied by repositioning the wrist or by adding an axial STIR sequence. Motion artifact is another common pitfall that can result either from patient motion or from pulsating blood within adjacent vessels. Motion artifact can either obscure abnormalities of the tendon or result in spurious intrasubstance signal mimicking pathology. Patient motion can be minimized by ensuring patient comfort and by minimizing the length of the exam time. Phase encoding should be directed in the vertical plane on axial images of the wrist to minimize artifact from pulsating blood over the region of the tendons. Magic angle effect, seen on short echo time sequences, is another potential pitfall that may result in spurious intrasubstance signal and mimic tendinosis. This phenomenon is most likely to occur in the flexor pollicis longus tendon as it courses from the distal aspect of the carpal tunnel toward the base of the thumb, but it has also been described in the extensor carpi ulnaris and extensor pollicis longus tendons. Intrasubstance signal resulting from magic angle can be differentiated from tendon pathology by recognizing that the signal diminishes or resolves on the T2-weighted sequences. The tendon morphology will be normal and there will be a lack of adjacent inflammatory changes when intrinsic signal alteration is the result of magic angle.
LIGAMENTS
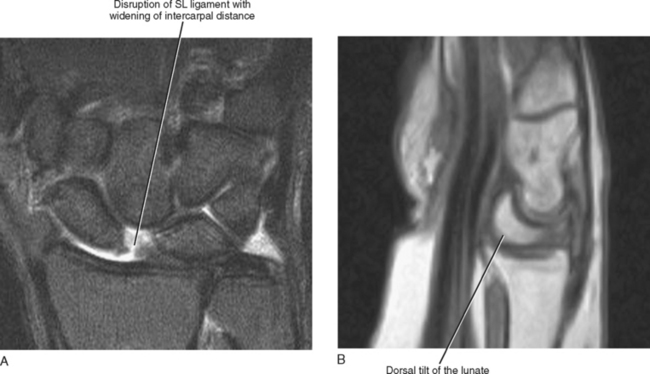
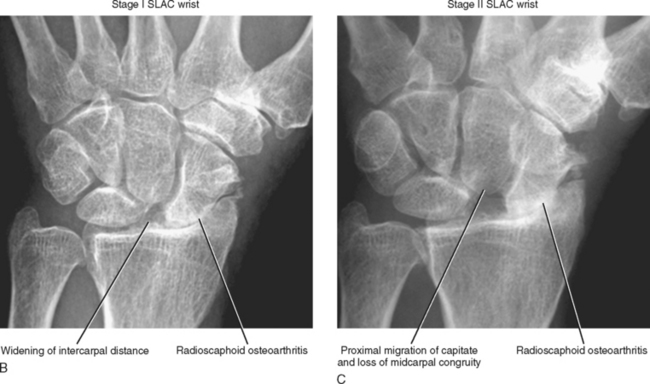
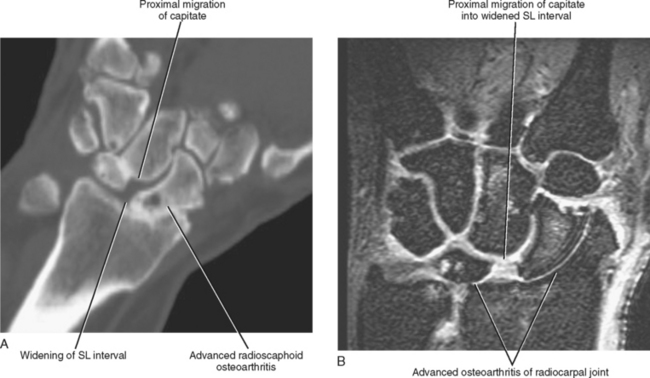
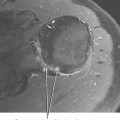
A fall on an outstretched hand is the most common mechanism of injury leading to ligamentous injury and carpal instability. Injury typically begins with disruption of the scapholunate ligament, however, with increasing severity of injury. The forces are transmitted in a pattern that encircles the lunate, resulting in disruption of both the volar and dorsal capsular attachments with the most severe injuries resulting in complete disruption of the ligamentous support for the lunate (Table 9-3). Four stages of injury have been described, ranging from isolated scapholunate ligament disruption to complete perilunate dislocation. Disruption of the scapholunate ligament is associated with an injury pattern referred to as dorsal intercalated segmental instability (DISI), which results in the loss of linkage of the scaphoid, lunate, and capitate. Radiographic and MRI findings indicative of a DISI injury pattern include widening of the scapholunate intercarpal distance, dorsal tilt of the lunate, and volar rotation of the distal pole of the scaphoid (Fig. 9-8). Over time, proximal carpal row instability leads to increased widening of the scapholunate distance and radioscaphoid articular cartilage loss and osteoarthritis referred to as stage I scapholunate advanced collapse (SLAC wrist). Proximal migration of the capitate is a late sequela of instability and results in an end-stage degenerative collapse of the midcarpus with loss of the midcarpal congruity, referred to as stage II scapholunate advanced collapse (SLAC) wrist (Figs. 9-9 and 9-10).
Table 9-3 Common Carpal Instability Patterns
| Pattern | Radiographic Findings |
|---|---|
| Scapholunate (SL) dissociation (rotatory subluxation) | |
| DISI (dorsal intercalated segmental instability) | |
| VISI (volar intercalated segmental instability) |
Although the extrinsic ligaments of the wrist are vital for maintaining proper carpal alignment, MR imaging lacks sensitivity and specificity with regard to the evaluation of the integrity of these ligaments, and for the most part MRI plays only a minor role in the evaluation of these structures. The presence of soft tissue edema and swelling along either the volar or dorsal aspect of the capsule of the wrist in the setting of trauma is an indicator of extrinsic ligament injury and is usually best identified on axial images, whereas the abnormality may also be identified on sagittal and coronal T2-weighted images with fat suppression (Fig. 9-11). The possibility of injury should be suggested on the basis of these findings, but it is difficult to accurately determine the status of the individual extrinsic ligaments. The presence of capsular edema should also prompt a thorough search for small cortical avulsion fractures of the carpal bones, such as a dorsal triquetral avulsion fracture, and radiographic correlation or CT examination may be necessary to accurately depict such avulsion injuries.