Multiple sclerosis is widely recognized as the most commonly identified cause of progressive neurologic disability in young adults throughout the developed world. The disorder is clinically suspected when patients experience either acute attacks of neurologic compromise or instead are afflicted by a steadily progressive deterioration in functional capabilities. The pathophysiology of acute exacerbations is thought to be related to the development of inflammation and its consequences, within strategic and often discrete central nervous system tract systems. Although a myriad of hypotheses have been formulated to explain the underpinnings of the mechanisms that contribute to both the predilection and triggering of the multiphasic inflammatory events that personify multiple sclerosis, much remains to be done to understand fully the specific set and sequence of events that produce the disease and its cardinal features.
Multiple sclerosis (MS) is widely recognized as the most commonly identified cause of progressive neurologic disability in young adults throughout the developed world. The disorder is clinically suspected when patients experience either acute attacks of neurologic compromise or instead are afflicted by a steadily progressive deterioration in functional capabilities. In the former circumstance, attacks or so-called “exacerbations” can literally produce any neurologic symptom ( Table 1 ) with a persistence of at least 24 hours (but often lasting much longer) followed by a period of partial and in some cases nearly complete recovery. The pathophysiology of acute exacerbations (as part of relapsing remitting MS [RRMS]) is thought to be related to the development of inflammation and its consequences, within strategic (often referred to as “eloquent”) and often discrete central nervous system (CNS) tract systems. Although a myriad of hypotheses have been formulated to explain the underpinnings of the mechanisms that contribute to both the predilection and triggering of the multiphasic inflammatory events that personify MS, much remains to be done to understand fully the specific set and sequence of events that produce the disease and its cardinal features.
| Exacerbations | Symptoms | Progression Features | Interventions |
|---|---|---|---|
| Optic neuritis |
|
|
|
| Myelitis |
|
|
|
| Ocular, motor, vestibular |
|
|
|
| Paroxysms |
| Tend to be transient | Membrane stabilizers |
| Uhthoff’s | Virtually any physical or cognitive deficit in multiple sclerosis can be stereotypically and reversibly intensified or exacerbation with infection, heat, prolonged exercise, or stress. | This phenomenon becomes more prominent as the disease advances. Uhthoff’s phenomenon represents one of the most vexing and disabling aspects of multiple sclerosis and is highly limiting to many patients. It signifies reversible conduction block secondary to demyelination. |
|
| Cognitive |
|
|
|
| Fatigue | Literally affects all aspect of an multiple sclerosis patient’s life. Often related to sleep disturbance, mood dysregulation, Uhthoff’s phenomenon, altered properties of physical functions (eg, faulty gait mechanics, spasticity, and so forth). |
|
|
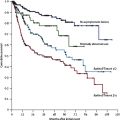
In contrast to the RRMS phase of the disease, many patients are afflicted with either a wholly progressive and insidiously changing course of disability from the inception without any evidence of acute attacks (primary progressive MS), or RRMS patients later transition into this phase of the disease (secondary progressive MS) after years of having intermittently active inflammatory events (clinically characterized by exacerbations and radiographically by new MR imaging lesions). Despite vigorous debate, most who actively manage MS patients understand that the accrual of permanent physical and intellectual disability can be a derivative of the exacerbating (most patients do not fully recover from their attacks), progressive, and even subclinical aspects of the disease.
Historically, MS is not a newly recognized disorder. Perhaps the first individual identified with a disease course thought to be indistinguishable from MS was St. Ludwina of Schiedam, a Dutch girl who lived in the fourteenth century, and who at the age of 16 fell in an ice skating accident, which was subsequently followed by a relapse-remitting course of neurologic attacks and remissions. She later became permanently disabled and died before her sixtieth birthday. The work of Charcot in the nineteenth century was seminal in that he and his group at the Salpetiere in Paris exhaustively chronicalized the longitudinal changes in the disease course and its impact on clinical disability over the life of patients with MS. Further, his group systematically performed neuropathologic studies on the brain and spinal cord on these same patients after death, and thereby established the two cardinal tenets of neurologic practice: where is the lesion that is responsible for the resulting clinical signs and symptoms, and what is the nature or etiology of this lesion? Although Charcot did not discover MS clinically or pathologically, he and his collaborators did institute the framework on which much progress has been made in the understanding of the relationship between the development of tissue injury in the CNS and its relevance to clinical disability.
The first MS diagnostic criteria was known as “Charcot’s triad” and consisted of scanning speech, intention tremor, and nystagmus. Further, his early work emphasized the central tenet of MS diagnosis, that of being a disorder that is multiphasic in producing clinical attacks occurring at different times in a patient’s life, and affecting distinctly different CNS injury targets (hence the adage “multiple events in space and time”). Since the time of Charcot, clinicians have witnessed an expanded and more precise series of diagnostic criteria that have refined the ability to confirm the diagnosis with greater sensitivity and specificity. Perhaps what has changed most profoundly in the last few decades has been the recognition that the presentation of a clinically isolated demyelinating syndrome, the first recognizable clinical event, is most typically associated with clear and unmistakable dissemination of ineloquent brain or spinal cord lesions. This suggests that most of those evaluated with a clinically isolated demyelinating syndrome already have MS (once the mimics have been excluded) as their working diagnosis. This observation underscores the difficulty in trying to identify the true onset of the disease process, making proclamations about early diagnosis and treatment intervention erroneous in most circumstances. There have now been three published early treatment clinical trials that demonstrate benefit to those patients randomized to active disease-modifying therapy with interferon at the time of their clinically isolated demyelinating syndrome, when compared with those receiving placebos. This suggests that the rubric of MS only being declared at a time when a patient has experienced multiple attacks or exacerbations in “space and time” is outdated and likely of detriment to patients. Instead, it now seems appropriate to use the “working diagnosis” of MS when patients present with a single (or more than one) event, not explained by an alternative etiology, and when there is evidence of disease dissemination anatomically as defined by MR imaging criteria. There is little debate today that MS is radiographically substantially more active (perhaps as much as 5–10 times) than what is anticipated observing clinically over time. This confirms that the disease process in MS is much more active than previously appreciated and likely constitutively. An important point of emphasis here is that this level of heightened activity observed by MR imaging is done so with conventional technical applications. With the advent of nonconventional MR imaging techniques, such as with diffusion tensor, magnetization transfer, and spectroscopic applications, it seems that nearly the entire central neuraxis of MS is affected by the disease process (see other sections in this issue for further discussion). Perhaps MS is not truly characterized by “multiple” areas of sclerosis, but rather the true representation of the disease and its associated histopathologic profile is one of a “diffuse” sclerosis.
The inflammatory hypothesis as an underlying and unifying principle for understanding how the course and tempo of tissue injury proceeds in MS is not a contemporary advance. Instead, it was known for quite some time that a distinguishing feature of this disease has been related to the conspicuous and exuberant presence of mononuclear cell infiltrates that seem to congregate around postcapillary venules within the brain and spinal cord. The initial and most rigorous observation of this classic pathologic profile was published by Rindfleisch in 1863. Using rudimentary microscopic techniques, he was able to identify perivenular inflammation in tissues derived from patients with MS. This observation has been corroborated innumerable times, and has been the basis and pretext for widespread research on the mechanisms of mononuclear cell trafficking from the circulation into the various tissue compartments of the body.
Although is it fully appreciated that the interaction of specific families of adhesion molecules facilitates the redistribution of lymphocytes and macrophages from the circulation to the blood vessel endothelium for physical tethering and stabilization, and ultimately transmigration into the CNS, in general there is a paucity of endothelial expression of these molecules in normal subjects. Alternately, in MS patients, there is an unmistakable up-regulation in the expression of cell adhesion molecules on cerebrovascular endothelium that can serve as a scaffolding for the migration of circulating mononuclear cells into the brain and spinal cord. On their entry, these cells can then participate in a complex orchestration of injury cascades that seem to culminate in inflammation; demyelination; remyelination; axonal dysfunction or degeneration; oligodendrocyte apoptosis; and ultimately neurodegeneration and gliosis (the sclerosis component of MS).
What is the evidence for inflammatory mechanisms underlying tissue injury in multiple sclerosis?
Although those who have worked in this field recognize and appreciate the contributions made by modeling inflammation and cellular trafficking mechanisms in animal models of MS, it is abundantly evident that these models do not fully parody the full complexity of molecular processes that are being elucidated in human inflammatory demyelinating disease. As such, this section avoids any discussion whatsoever as it relates to the use of animal experimentation as it may be related to MS pathophysiology, immunology, or immunogenetics. Instead, it is now patently clear that much has actually been learned from the direct investigation of the MS disease process in those afflicted with the condition.
MS is similar to a number of other immune-mediated disorders in that there seems to be fundamental derangements in a series of regulator mechanisms that allow the proceedings of the immune system normally to be telescoped on the identification and neutralization of foreign invaders (eg, virus, bacteria, fungi, parasites). Unfortunately, in MS there is also a corresponding capability inherent within the immune system that allows for the inappropriate recognition of self-epitopes fomenting a series of inflammatory reactions that lead to tissue injury. The ability precisely to distinguish between self-antigens and foreign antigens is related to these regulatory mechanisms that collectively might be referred to as “tolerance.” A breach in tolerance has been considered as a central hypothesis within the landscape of autoimmune disorders. In a sense, the behavior of the immune system is likely akin to that of the system when confronted with a transplanted organ (a kidney, heart, and so forth). As such, MS may be highly related to processes that are germane to transplant rejection. It is not surprising that a number of therapeutic strategies applied to MS and related diseases involve treatments that are mainstays of transplant medicine.
An important disclaimer in any discussion related to the underlying principles of how inflammation is integrated into the grand schema of MS pathophysiology, is that the primary genetic and environmental factors that predispose to and trigger the disease process remain enigmatic. Despite this, much has been learned about the phenomenology that ensues after the inception of the disease process. For instance, it has been demonstrated that MS patients do have T cells that are actively primed against myelin antigens (albeit not exclusively). Relevant to this observation has been that the presence of these cellular clones is strongly correlated with clinical disease activity and resultant disability. An interesting feature of these differentiated and potentially pathogenic (at least partially) lymphocytes is that they exhibit features that render them more resistant to programmed cell death (ie, apoptosis), implicating a failure of an adaptive process that serves to screen and edit the evolution and expansion of autoaggressive responses. Studies using anti-CD4 strategies may have failed on the basis of this disease-related inherent resistance.
The indiscriminate depletion of T cells may not be a viable treatment strategy for patients with MS for a variety of reasons. A subpopulation of CD4 + T helper cells was recently characterized as regulatory T (Treg) cells. The biologic function of these cells seems to be the maintenance of immune homeostasis . The transcription factor forkhead box p3 (FOXp3) seems to be a key regulator of Treg function . It was recently demonstrated that FOXp3 transcription and protein levels are decreased in patients with MS 6 .
Pathologic investigations of human MS brain tissue have revealed various histopathologic substrates, with some degree of heterogeneity. The parenchymal CNS infiltrate has been shown to consist of B and T cells along with macrophages. Although both CD4 and CD8 T cells are redistributed from the peripheral circulation into the perivenular space and CNS parenchyma, importantly, CD8 T cells seem to be enriched and clonally expanded in MS indicating that they must play an important local role. The antigenic specificity of these cells and their role (pathogenic versus immune regulatory), however, is still unclear. Importantly, CNS-specific autoreactive CD8 T-cell responses are classically noted in RRMS. In contrast, a deficiency of CD4 and CD8 T-cell regulatory functions may underlie the proinflammatory state in MS. For instance, therapy with glatiramer acetate results in the restoration of this regulatory capacity of CD8 T cells, which may serve as an important anti-inflammatory mechanism associated with mitigation of the disease both clinically and radiographically.
In addition to the role posited for T-cell dysregulation in MS, a number of lines of evidence have implicated humoral mechanisms as a central element of MS disease pathogenesis. In 1942, Kabat and colleagues reported that cerebrospinal fluid derived from MS patients contained evidence of antibody synthesis (the oligoclonal band) that seemed to be compartment driven (corresponding synthesis was not observed in the peripheral blood). These early studies have been corroborated and expanded (including refined recommendations for using isoelectric focusing techniques to optimize sensitivity) such that it is now recognized that most MS patients have cerebrospinal fluid findings of oligoclonal bands and that their presence at the time of clinically isolated demyelinating syndrome strongly predicts conversion to clinically definite MS. It is important to underscore, however, that a vast array of inflammatory and infectious etiologies can also result in the production of cerebrospinal fluid oligoclonal bands.
Humoral immune responses involve a complex series of molecular changes within B cells that ultimately result in the production of antibodies. On stimulation of B cells there is an initial process of somatic hypermutation within immunoglobulin genes to commence the process of epitope recognition and binding to the business end of antibodies. With time and repeated stimulation (as with booster immunizations) affinity maturation is promoted. Initial development of early IgM antibodies is later transitioned to a class switch to long-term IgG classed antibodies.
A humoral mechanism of potential relevance (albeit not yet proved in MS) to the mechanisms of inflammation in MS is molecular mimicry. An active infection normally generates B cell–derived antibodies targeted against infectious epitopes, which can be structurally (sequence or spatial domain) homologous to self tissue epitopes thereby establishing the possibility of cross-reactivity and the development of autoaggressive immune responses. There is some evidence for this process in patients infected with human T-lymphotropic virus 1 who develop an associated myelopathy (also known as “tropical spastic pareparesis”). It is important to recognize that the human immune system has an inherent capability to generate autoaggressive responses but that a series of adaptive regulatory control mechanisms averts most of these. For instance, the evolution of B cell–derived self-targeted antibodies can provoke replacement of the immunoglobulin light chains with newly arranged molecular variations. This process has been referred to as “receptor revision” or “editing” and has been documented in B cells derived from the cerebrospinal fluid of MS patients. Nevertheless, a failure in the competency of these editing mechanisms may underlie some aspects of humorally mediated tissue injury in MS. The role of B-cell regulation in the pathogenesis and perpetuation of MS has been further appreciated by a recent study that showed that a selective monoclonal antibody against a B-cell developmental protein, CD20, was able significantly to reduce both clinical and MR imaging measures of disease activity in a small cohort of RRMS patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree