
Fig. 41.1
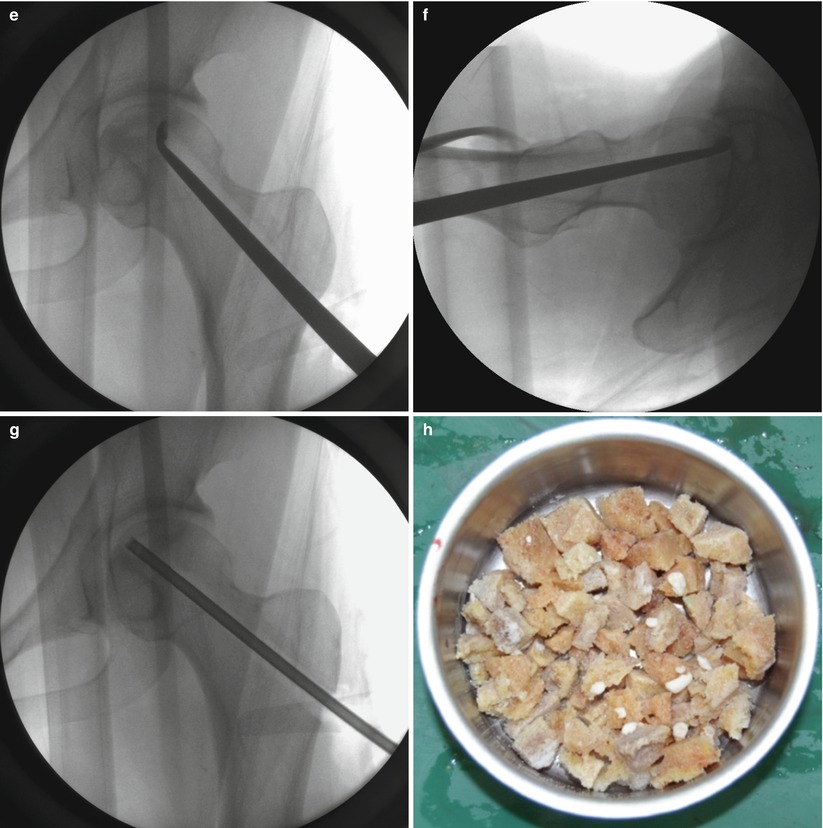
At 1 cm distal to the vastus ridge, a guide pin is inserted to the direction of the center of necrosis under the guidance of the image intensifier in the anteroposterior (a) and axial direction (b). A tunnel reaching the margin of necrotic area is established with the use of 11 mm trephine drill (c) and the cancellous bone block from the proximal femur is reserved for impaction grafting (d). After central core biopsy, the remaining necrotic bone is completely curetted under the image intensifier in two directions (e, f) followed by thorough irrigation of debris (g). The photograph demonstrates washed and squeezed fresh-frozen allograft chips with a size of 7–10 mm (h), and they are impacted into the remaining void following impaction of the cancellous bone block from the proximal femur (i)
A patient is placed in the supine on the fracture table with 20° internal rotation of the leg. Gentle compression instead of traction is applied to press the femoral head against the chondral surface of the acetabulum so as to regain the sphericity and prevent the possible perforation of the femoral head. Five- to seven-cm-sized lateral skin incision is made centered over 1 cm distal to the vastus lateralis ridge. The fascia lata is split in the direction of the skin incision, and the vastus lateralis muscle is lifted off from the lateral cortex of the femur following L-shaped incision of the muscle. After making a small cortical window 1 cm distal to the vastus ridge, a guide pin is inserted to the direction of the center of necrosis (usually superolateral) under the guidance of the image intensifier and preoperative MRI (Fig. 41.1a, b). An intraosseous tunnel reaching the margin of necrotic area is created with the use of a 9–15 mm trephine drill (Fig. 41.1c), and the cancellous bone from the proximal femur is saved for impaction grafting (Fig. 41.1d). For histologic evaluation, central core biopsy is taken from the necrotic bone, and the remnant necrotic bone is completely curetted or removed using high-speed burrs under the image intensifier in two directions (Fig. 41.1e, f). Following irrigation of debris, a normal cancellous bone taken during tunneling is shaped into bone chips with a size of 7–10 mm (Fig. 41.1g). The empty space in the femoral head is filled with these bone chips, and solid impaction is applied layer by layer to cover the subchondral bone thoroughly. The remaining tunnel can be filled with fresh-frozen allograft [14] or autogenous iliac bone graft with or without additional allograft [19] depending on the surgeon’s preference in the same manner (Fig. 41.1h, i). Care should be taken not to put the cortical window inside the lateral cortex of the femur for possible arthroplasty. Lastly, soft tissues including the vastus lateralis and fascia lata are repaired layer by layer. During 6 weeks after surgery, touch weight-bearing with two crutches is allowed followed by weight-bearing up to a maximum of 50 % body weight in the next 6 weeks. Full weight-bearing is permitted using one crutch to slow down from 3 months after surgery [14].
41.4 Technical Considerations
In addition to head-preserving procedure for ONFH, bone impaction grafting is now widely applied to a variety of orthopedic procedures such as management of osteonecrosis in other joints [20, 21], osteosynthesis for complicated fracture [22] or nonunion with large segmental defects [23], ACL reconstruction [24], and primary arthroplasty [25]. Their results of bone impaction grafting are encouraging, but there are still much room for improvements in surgical techniques and need for standardization for optimal treatment. Long-term results after bone impaction grafting for treating ONFH would be determined by proper patient selection, progression of the disease, and graft incorporation, but initial mechanical stability of the graft by optimal surgical technique will allow for long-term incorporation into the host bone without joint destruction. The understandings of the mechanical properties of impacted bone have recently increased, and despite most of these have originated from bench research for revision arthroplasties, some technical improvement can be applied to bone impaction grafting in the treatment of ONFH as well.
41.4.1 Graft Preparation
The technique of graft preparation in bone impaction grafting has been shown to be of both mechanical and biological importance. This technique includes graft selection and washing and particle size and grading.
41.4.1.1 Choice of Allograft and Washing
Optimizing the fat and water content produces a stronger graft that is more resistant to compressive stresses, preventing the femoral head from collapsing until bone growth will occur [26]. When fresh-frozen allograft is impacted, fat, fluid, and marrow particles in the marrow are either exuded or trapped in the space between particles. Their presence acts as lubricants between particles, reducing the interlocking of particles and allowing the graft to move more freely. Furthermore, the presence of this incompressible fluid damps and resists compressive forces during impaction, preventing the graft particles from moving into a compact bone [26]. Washed graft reducing fat content, however, has little lubricating fluid and better contact between the particles. On mechanical testing, washed graft demonstrated significantly more resistance than those without washing regardless of different particle size, and thus, washing allowed the production of stronger impacted graft [27]. On the contrary, Fosse et al. compared the effect of impaction force, number of impaction strokes, and bone liquid contents on mechanical behavior and demonstrated that the overall major contributor on load stiffness was liquid content [28]. High water content decreased load stiffness during load because liquid filled up more of the pore volume surrounding the bone particles, while low fat content increased stiffness significantly only during the initial phase of loading. Thus, they concluded that the preparation and impaction should be performed under dry conditions to improve the initial stability [29]. Recently, McKenna et al. performed mechanical shear testing in vitro on morselized human femoral heads, varying the amount of fat and water to determine their optimum concentrations [26]. They found that reducing the fat and eliminating water greatly improved the strength of bone graft. They concluded that the most effective means of producing a stable graft was first washing the graft with pulsed lavage reducing the level of fat and subsequent squeezing the graft of its remaining liquid content further reducing the total volume of fluid in an operative setting although it did not reach the ideal concentration of fat and water.
While washing appears to improve the mechanical properties of fresh-frozen allograft, the effect of washing on the biological properties is less clear. Washing the trabecular allografts may enhance graft incorporation by washing out immunological inflammatory factors existing in blood, marrow, and fat, while it can also diminish the incorporation process by washing out biologically active factors stimulating new bone formation [30]. Van der Donk et al. performed animal experiments using autograft and allograft and divided them into three treatment groups as those with impacted, rinsed and impacted, and rinsed, impacted, rinsed, and impacted again. After histologic analyses at 6 weeks, they found that new bone and total tissue ingrowth were higher in autograft than in allografts, especially in the nonrinsed group. With rinsing, total tissue ingrowth increased in the allograft group to approach that of autograft, while rinsing after impaction did not additionally alter bone ingrowth. Thus, they concluded that incorporation of allografts could be improved by rinsing the grafts before impaction [30]. Because autograft contains osteoprogenitor cells and local growth factors to induce the mesenchymal cells to differentiate into mature osteoblasts, rinsing removes beneficial factors from the autograft and leads to poorer incorporation [30].
On the other hand, some authors reported that freeze-dried irradiated grafts showed higher stiffness than fresh-frozen grafts whatever the size of the particles [31, 32]. The brittleness of freeze-dried irradiated bone, caused by loss of the capacity to absorb energy in a plastic way, has been demonstrated to be superior to a fresh-frozen one in a femoral impaction model [31]. Also, Cornu et al. explained improved results with freeze-dried irradiated bone due to incomplete rehydration and increase in the interlocking effect by increasing their water content during later progressive rehydration because rehydration could last for longer than 1 day [32]. Although both fresh-frozen and freeze-dried allograft have demonstrated successful outcome after revision THA [16, 17, 33], there is clearly a lack of quality data in this area, and well-designed clinical trials are required to help inform and guide practice [34].
41.4.1.2 Particle Size
The impacted layer of large particles has been reported to be superior, as a greater magnitude of force would be required to deform the large particles compared to smaller particles [35–37]. Xu et al. compared the mechanical properties of impacted graft with a size of 7–10 mm bone and a small slurry bone with a size of 2 mm [38]. They found that 7–10 mm bone grafts showed higher height, elastic modulus, and massive extrusion strength than those of the small slurry bone grafts. Also, the bone mineral density of the 7–10 mm grafts continued to increase during impaction and became higher than that of the small slurry bone grafts after ten impactions. Bolder et al. performed a gradually increasing dynamic loading experiment with radiostereometric analysis [39]. They found that large bone grafts with an average size of 9 mm produced by hand with a rongeur did provide more initial stability than those with a mean size of 2 mm produced by a bone mill. Therefore, considering these biomechanical studies, the use of large bone chips of between 8 and 10 mm appears to be rational to provide adequate initial stability.
Larger particles have a more porous bone bed between the graft particles, and microvascularity may depend on the graft porosity. Therefore, this use of the larger chips might encourage bone ingrowth and seems to be of benefit not only biomechanically but also biologically [40].
41.4.1.3 Particle Grading
The behavior of impacted graft has been investigated largely using the principles of soil mechanics, and according to them, the mechanical properties of impacted particles are dependent on the particle size distribution (grading) as well as the mechanical properties of the individual particle [27]. Fosse et al. examined the relative influence of different bone particle size, impaction energy, and liquid content on impacted bone stiffness and found that pellets with a wider range of particle sizes had better mechanical properties than those with unisized particles [28]. During impaction, large particles in a well-graded pellet slide in between each other, and with better grading, smaller granules fill the voids resulting in more compaction and less deformation. Dunlop et al. performed mechanical shear testing using fresh-frozen allograft with differing particle size distributions. They demonstrated that a well-graded particle size of allograft was more resistant to shear force. Although these results are encouraging, the effects of a well-graded particle size may be less important than surgical technique, and the impaction may compensate the advantages of a well-graded chip size [40]. Biologically, idealized grading of particle size can make the graft more impacted but bring a detrimental effect on subsequent bone ingrowth due to decreased microcirculation [41, 42].
41.4.2 Impaction Technique
One of the fundamental difficulties of bone impaction grafting wherever it is applied is the intraoperative decision regarding how “vigorous” it should be applied and when the graft can be adequately impacted. The degree of impaction is determined by the impaction force and the number of impaction strikes [43]. No specific guideline, however, exists to standardize the amount of energy transmitted to the bone graft and enable the surgeon to determine when the graft is adequately impacted. This is of clinical importance because subchondral perforation during surgery and progression of collapse was a concern in a previous study (7 %) [14]. Also this concern regarding fracture may lead to under-impaction of the graft and subsequent collapse of femoral head. Thus, in the absence of methods for establishing when the graft is adequately impacted, there should be a significant learning curve between over-impaction causing subchondral perforation and under-impaction leading to collapse of femoral head.
Although experimental model is different from clinical situation and the clinical setting of impaction grafting for ONFH is also different from those for revision THA, Flannery et al. examined the threshold force using adult sow femurs in revision THA [44], and the threshold force before fracture was found to be 4 kN. This force was similar to the maximum force obtained from direct impaction of a slap hammer on the load cell, which was 3.5 kN. Fosse et al. also performed the same experiment using embalmed human femurs. The threshold force was found to be 0.5 kN and four-fifths of the femurs fractured above 1.6 kN. Thus, there is limited information regarding adequate force in bone impaction grafting. Further studies should be performed to determine the threshold force of bone impaction grafting in the treatment of ONFH and monitor this force in the clinical setting as well.
Increased number of strikes can bring the particles to slide in between each other and induce plastic deformation. Obviously, stiffness in impacted morselized bone to a certain extent would increase by number of impactions [45]. This rearrangement, however, would reach plateau above which further strokes fail to impact for increasing stiffness of the graft [28]. Fosse et al. measured graft stiffness stroke-by-stroke [29]. They found that no significant increase in stiffness was achieved after five strokes at the highest drop level, while drop level of the impaction slap hammer increased bone stiffness on each layer of morselized bone during impaction. They also compared factors affecting stiffness properties in impacted morselized bone one by one while keeping all other involved factors constant [28]. Graft with low water content had a major effect, while increasing the number of impaction strokes beyond five per layer had a minor effect. Thus, optimal stability was achieved with dried and well-graded particle, but the number of heavy impaction strokes could be restricted.
Because bone graft is impacted manually with a hammer, the concept of “vigorous impaction” is always subjective [40]. Even if the optimal magnitude of the impaction force as well as the number of strikes would be identified, there always exists a risk of over- or under-impaction. Hostner et al. compared conventional impaction technique with an impaction technique using polished and rotating impactors [46]. They found that this new impaction technique obtained a more reproducible procedure and less risk for fracture and resulted in stability equal to that obtained with the conventional technique. Recently, Putzer et al. compared two different methods of bone impaction grafting [47]. The pneumatic method reduced the risk of fracture in vivo, as force peaks were smaller and applied for a shorter period, while results from manual impaction demonstrated higher variability and depended much on the experience of the surgeon. Thus, they concluded that pneumatic hammer was a suitable tool to standardize the impaction process.
41.5 Results
To date, there have been limited outcomes available after bone impaction grafting in the treatment for ONFH. Rijnen et al. reported the first clinical and radiographic outcomes in English after bone impaction grafting in 28 hips with ONFH (10 steroid induced, 4 alcoholic, 1 hereditary hyperlipidemia, 5 trauma related, 1 SCFE, and 7 idiopathic) (Table 41.1) [14]. Fourteen hips (50 %) already had preoperative collapse of the femoral head. The overall clinical success rate was 64 %, whereas 15 hips (54 %) demonstrated radiographic success at an average follow-up of 43 months. Patients older than 30 years had a significantly higher chance of a radiographic failure (hazard ratio, 6.075). Thus, three patients with an average age of 21 years in stage 4 showed remarkable recoveries and had good clinical results with improvement of Harris hip score (HHS) from 45 points preoperative to 89 points postoperative, while those older than 30 years had a preoperative HHS of 60 points, increasing to 71 points postoperative. They also reported that patients with preoperative collapse and use of corticosteroids had worse results. Park et al. reported the outcome in 42 hips (15 alcoholic, 8 steroid induced, 3 posttraumatic, and 6 idiopathic) according to ARCO classification including stage, quantification, and location [48]. They evaluated radiographic results using MRI after the procedure in 25 hips in which THA was not performed at an average follow-up of 15 months (range 11–23). They demonstrated overall clinical and radiographic success rate to be 74 and 50 %, respectively. They reported that lesions with large involvement (>30 %) or lateral location were significantly associated with clinical and radiographic failure in spite of short period of follow-up (average, 29 months) emphasizing the importance of the location as well as the size of involvement. Jung et al. reported outcomes in 95 hips with ONFH (41 alcoholic, 42 steroid induced, and 12 idiopathic). The overall clinical success rate was 78 %, whereas 44 hips (46 %) demonstrated radiographic success at an average follow-up of 43 months. They also concluded that lesions with large involvement or lateral location were significantly associated with radiographic failure.
Table 41.1
Clinical and radiographic results after bone impaction grafting
Hips (patients) | F-U (range), months | Age (range), years
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|