Chapter 34 Imaging of central nervous system (CNS) infection is most often initially performed by means of computed tomography (CT) to assess for the possibility of hydrocephalus or increased intracranial pressure prior to the preparation of a lumbar puncture. Nonspecific parenchymal hypoattenuation indicative of edema on CT is sometimes appreciated in cases of more focal infection. CT is superior in the evaluation of bone erosion and destruction. Magnetic resonance imaging (MRI) is warranted in the assessment of infectious complications such as abscess, empyema, vasculitis, and ischemia in the setting of a worsening clinical condition or lack of clinical improvement despite appropriate therapy. Infection is most often manifested on MRI by abnormal hyperintense signal on T2-weighted (T2W), proton density, and fluid-attenuated inversion–recovery (FLAIR) sequences, with corresponding hypointense signal on T1-weighted (T1W) sequences. Postcontrast T1W images are essential in the evaluation for infectious collections and meningeal enhancement. Magnetic resonance venography (MRV) sequences may detect associated venous sinus thromboses. Diffusion-weighted imaging (DWI) may assist in localizing abscess collections, infection associated with ischemia, or both and may at times help distinguish lymphoma from abscess, especially in immunocompromised patients. DWI may also demonstrate lesions earlier than conventional sequences in viral infections such as herpes and West Nile virus (e-Fig. 34-1). Magnetic resonance spectroscopy has shown promise in distinguishing pyogenic abscesses from those caused by atypical organisms, with the former often demonstrating the presence of amino acids and lack of choline. e-Figure 34-1 West Nile virus. Nearly two thirds of cases of bacterial meningitis in the United States occur in children. Routes of transmission include hematogenous, direct traumatic, congenital routes, as well as direct extension from adjacent sinus or mastoid disease (Figs. 34-2 through 34-4 and e-Fig. 34-5). Imaging plays a key role in determining the course of treatment for bacterial infection. It is essential to distinguish between focal cerebritis (Fig. 34-6), which tends to respond to antibiotics, and abscess, which often requires surgical intervention. Hypoattenuation on CT, indicative of edema, and corresponding hyperintense T2W and hypointense T1W signal on MRI, with patchy nonspecific postcontrast enhancement, are typical imaging characteristics of cerebritis. Mild to moderate mass effect is often present. Sequential imaging is essential in the assessment of the response to antibiotics as well as for progression to an abscess. Progression from cerebritis to abscess generally takes 1 to 2 weeks but may progress more quickly in neonates. Citrobacter, Serratia, and Proteus are the most common causes of neonatal brain abscess. Citrobacter and Serratia infection may cause medullary vein thrombosis and associated hemorrhage (Fig. 34-7). In general, abscesses tend to be situated at gray-white matter junctions, where the diameter of the end arterioles decreases (Fig. 34-8). Opportunistic organisms are common in immunocompromised neonates. Figure 34-2 Parameningeal spread of retropharyngeal infectious process or abscess. Figure 34-3 Transverse sinus thrombosis associated with otomastoiditis or middle ear disease. Figure 34-4 Mastoiditis with associated epidural abscess. Figure 34-6 Cerebritis. Figure 34-7 Citrobacter infection with secondary venous thrombosis. Figure 34-8 Streptococcus viridans abscesses. e-Figure 34-5 Pott puffy tumor, with associated intracranial, extra axial pus. Differential diagnostic considerations of a peripherally contrast-enhancing fluid-filled structure in the brain includes infectious abscess and tumor. On DWI, abscesses will appear hyperintense (and dark on apparent diffusion coefficient, indicating restricting material within the capsule. On both MRI and CT, abscesses tend to have smooth regular inner margins and are often thinner walled along their medial edge than along their lateral margins. Intraventricular rupture of an abscess portends a poor outcome. Spectroscopy of abscesses is notable for the presence of amino acids and lactate (Fig. 34-9) and the absence of normal metabolite peaks. In neonates, ultrasonography may depict a hypoechoic abscess with peripheral hyperechogenicity, which may contain dependent echogenic debris. Figure 34-9 Cerebral abscess. Bacterial meningitis is the most common form of pediatric CNS infection. Although not diagnosed by imaging, imaging is warranted if a diagnosis is unclear, persisting seizures are present, and symptoms persist despite treatment. It is more common in preterm infants and full-term infants within the first month of life. The subarachnoid space tends to resist infection in older children, making meningitis in this age group a rarity. Most cases of neonatal meningitis in the United States are caused by group B Streptococcus (Fig. 34-10) and Escherichia coli. Other less common organisms (e.g., Serratia, enterococci, and Listeria) tend to inflict more extensive destruction. In infants older than 1 month, the most common causative organisms are Haemophilus influenza type B, Streptococcus pneumonia (Fig. 34-11), Neisseria meningitides, and Escherichia coli. Complications of meningitis include cerebritis, abscess, empyema, hydrocephalus, venous thrombosis, infarction (venous and arterial), ventriculitis (e-Fig. 34-12), mycotic aneurysms (Fig. 34-13), and sensorineural hearing loss (Fig. 34-14).
Infection and Inflammation
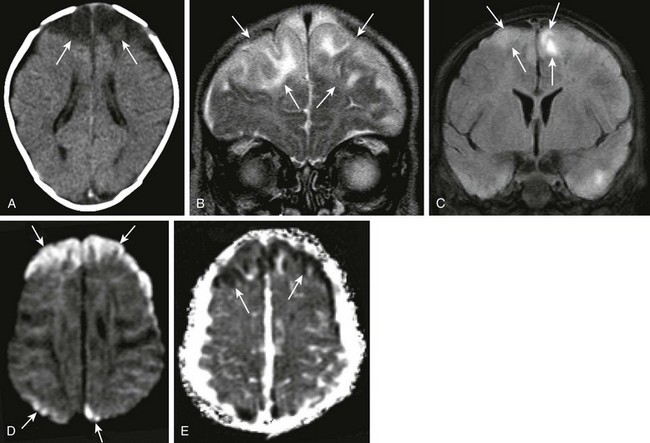
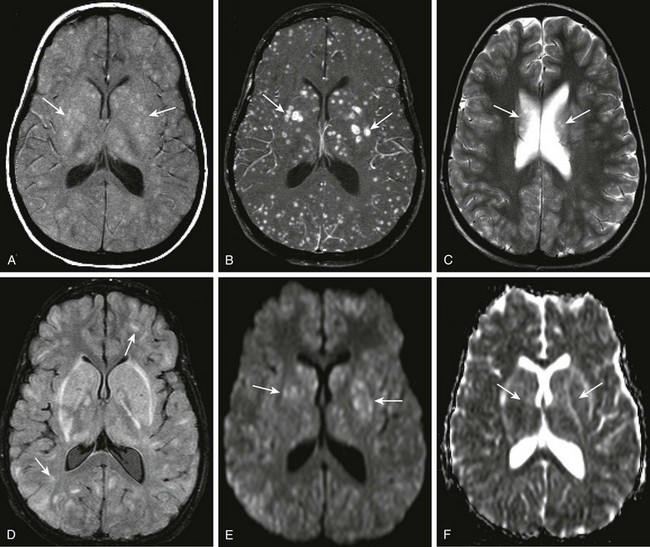
A patient with loss of consciousness and questionable history of mosquito bite. Coronal and axial fluid-attenuated inversion recovery (A and B, respectively), axial postcontrast spin echo T1 (arrows in C), and axial diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) map (D and E, respectively) were obtained. Note the T2 prolongation within the basal ganglia bilaterally (arrowheads in A and B), with some questionable contrast enhancement or magnetization transfer effect as seen on the postcontrast images (C). Increased signal on DWI as well as ADC maps (arrows in D and E), in keeping with T2 shine-through.
Bacterial Infections
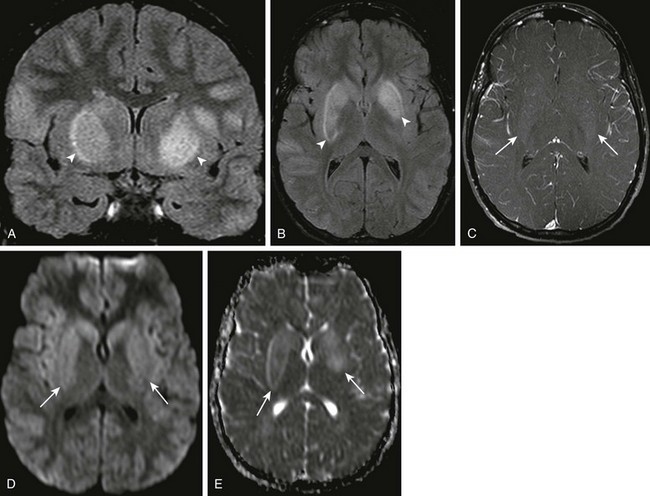
A 3-year-old female child with retropharyngeal abscess, now with fever, headache, emesis, and left sixth nerve palsy. Axial T2-weighted images at the level of the adenoids (A) and sphenoid bone (B) and coronal T2 (C) images, coronal (D) and sagittal (E) postcontrast T1, as well as three-dimensional time-of-flight magnetic resonance angiography (MRA) in the left anterior oblique projection (F) were obtained. Note the inflammatory process within the left retropharyngeal region (arrows in A). Note the abnormal marrow signal within the sphenoid bone (arrows in B and C). In addition, note the abnormal soft tissue seen extending superior to the sphenoid bone on the coronal T2 sequence (arrowhead in C). Corresponding abnormal contrast enhancement is seen along the region of the skull base and planum sphenoidale seen on the postcontrast images (arrows in D and E). Note the diminution in size of the right internal carotid artery (asterisks in C and D) with corresponding narrowing of the right supraclinoid carotid artery on the right on the MRA (arrows in F). (Case courtesy of Kim M. Cecil, Ph.D. Department of Radiology, Cincinnati Children’s Hospital.)
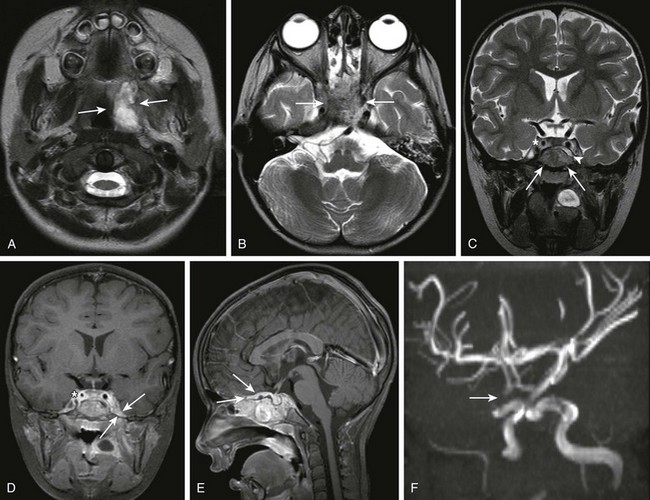
A patient with otitis media, headache, and papilledema. Axial noncontrast (A) and contrast-enhanced (B) computed tomography (CT) of the head through the level of the posterior fossa, axial magnetization transfer T1 precontrast (C) and postcontrast (D) magnetic resonance imaging scans, coronal T2 (E) and coronal multiple intensity projection image from a three-dimensional time-of-flight magnetic resonance venogram (MRV) (F) were obtained. Note the dense appearance within the right transverse sinus on the noncontrast CT study (arrow in A), with corresponding lack of contrast filling on the postcontrast CT study (arrow in B). Corresponding T1 shortening is seen on the precontrast magnetic resonance image (arrow in C), with corresponding abnormal signal on the postcontrast images in keeping with clot or slow flow within the region of the right transverse sinus or sigmoid sinus (arrow in D). Corresponding T2 prolongation is seen on the coronal T2 image (arrow in E). Note the striking asymmetry of flow within the right posterior fossa dural venous system or internal jugular vein on the right on the three-dimensional time-of-flight MRV (arrows F).
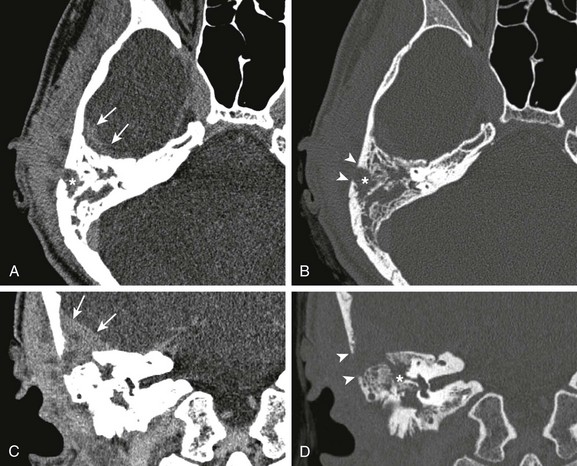
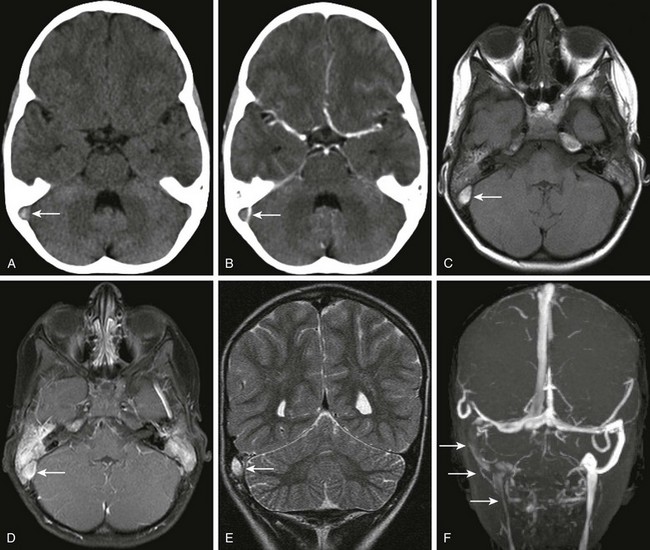
A 17-year-old male with 5-month history of otitis media, now with severe right-sided mastoid pain. Axial postcontrast computed tomography images through the right mastoid region, including soft tissue (A) and bone windows (B), and direct coronal images from the same study obtained on soft tissue (C) and bone windows (D) were obtained. Note the abnormal soft tissue opacification within the right mastoid region (asterisks in A and B). Associated abnormal soft tissue swelling is seen along the external surface of the skull or scalp, with an abnormal soft tissue component seen extending intracranially (arrows), corresponding to epidural abscess formation. Bony resorption or breakdown is seen within the mastoid cortex laterally (arrowheads). In addition, note the erosion of the lateral semicircular canal (asterisk in D).
A 2-year-old male with Staphylococcus aureus bacteremia, persistent fevers, and new-onset of hypertension. A and B, Sagittal T1-weighted and axial T2-weighted images demonstrate T1 and T2 prolongation (arrows). C, Sagittal postcontrast spin echo images show mild cortical enhancement (arrows) D, An axial diffusion-weighted imaging shows increased signal (arrows). E, The corresponding decreased signal indicates restricted diffusion on apparent diffusion coefficient image.
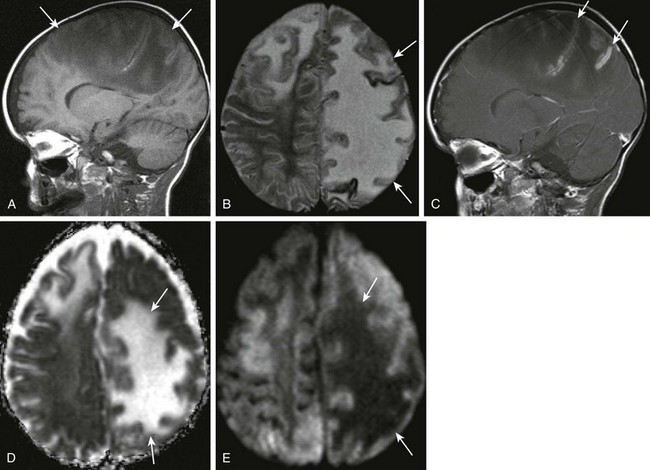
A 7-day-old full-term female neonate with seizures, and gram-negative sepsis, as well as increased white blood cell count on lumbar puncture. Axial precontrast and postcontrast T1, (A and B, respectively), axial T2 (C), axial gradient echo (D), as well as axial diffusion-weighted imaging and apparent diffusion coefficient maps (E and F, respectively) were obtained. Note the area of T1 prolongation within the left posterior frontal parietal region (arrows A and B), corresponding to areas with linear signal voids on both T2 and gradient echo sequences (arrows in C and D), corresponding to distended medullary veins. Note the absence of diffusion restriction and the presence of increased diffusion in the corresponding area on the diffusion-weighted sequences (arrows in E and F).
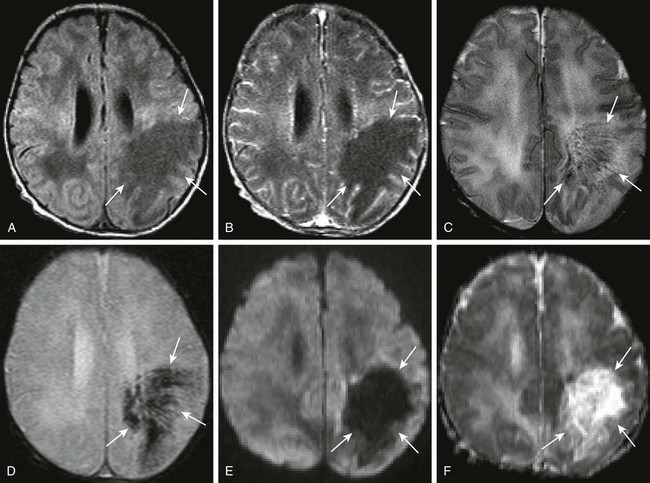
A 12-year-old female child with acute myelogenous leukemia and mental status changes. Axial T1 magnetization transfer (MT) images, precontrast and post contrast (A and B), axial T2 and fluid-attenuated inversion recovery (FLAIR) (C and D), and axial diffusion-weighted imaging with apparent diffusion coefficient maps (E and F) were obtained. Note the areas of T1 shortening on the precontrast MT image (arrows in A), and the corresponding marked gadolinium enhancement within multiple bilateral intraparenchymal nodules of differing size (arrows in B). T2 prolongation is noted on the axial T2 and FLAIR sequences in some corresponding areas (arrows in C and D), but this is markedly less conspicuous than on the postcontrast images. Subtle restricted diffusion is noted in some of the nodular areas, specifically within the region of the basal ganglia bilaterally corresponding to the largest lesions seen on postcontrast images (arrows in E and F).
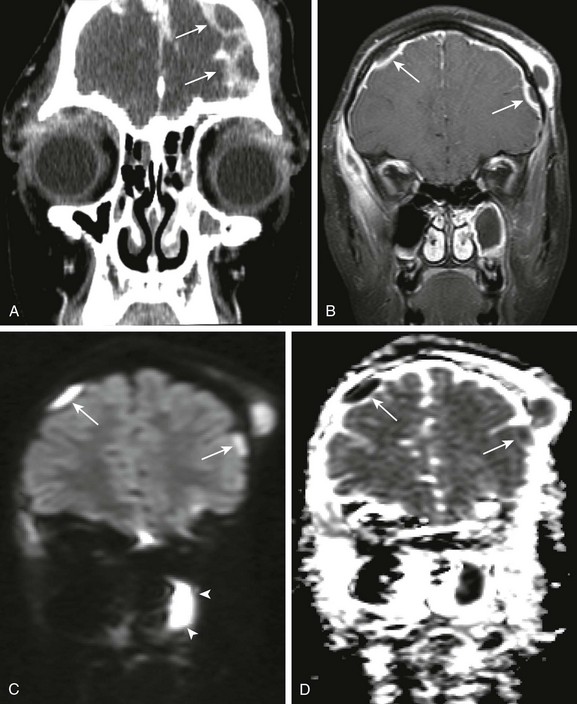
An 11-year old female child with orbital swelling, preseptal cellulitis, and increase in forehead swelling associated with pan-sinusitis. The patient initially presented with syncope, fever, and bilateral orbital swelling. Coronal postcontrast computed tomography (A), coronal postcontrast fat saturated T1 magnetic resonance image through the frontal region (B), and coronal diffusion-weighted imaging with apparent diffusion coefficient map (C and D, respectively) were obtained. Note the abnormal extraaxial collections (arrows in A and B). Corresponding restricted diffusion is seen in the extraaxial space over the right cerebral hemisphere (arrows in C and D). Note also that corresponding to the area of apparent fluid collection within the left maxillary sinus (arrowheads B), an area of corresponding restricted diffusion is present (arrowheads in C and D), corresponding to pus within the left maxillary sinus.
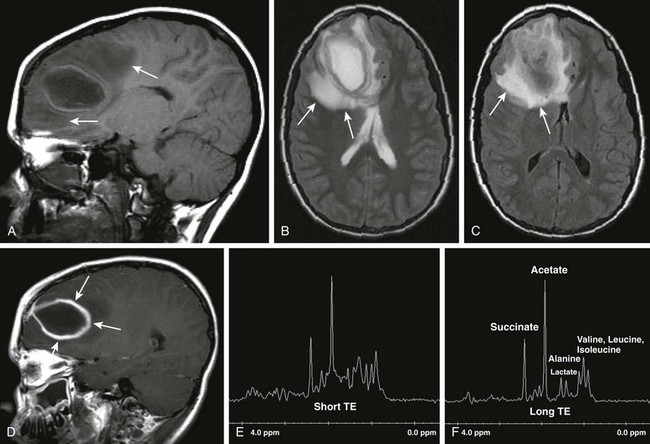
Patient with seizures and fever. Sagittal T1 (A), axial T2 (B), axial fluid-attenuated inversion–recovery (C), postcontrast sagittal spin echo images (D), as well as short TE and long TE spectroscopic images (E and F, respectively) were obtained. Note the areas of T2 prolongation (B and C), with some central low signal intensity (C) in the region of abscess with surrounding vasogenic edema. Thick, rindlike enhancement of the periphery of the right frontal abscess is seen (arrows in D). Spectroscopic images demonstrate abnormal amino acid peaks at around 1 part per million (ppm), and a doublet lactate peak deflected upward at 1.33 ppm.
Infection and Inflammation