In principle, any mechanism with kinetic energy to the thoracic cage may cause blunt cardiac trauma
Typical examples:
Motor-vehicle accident (>20 mph) with compression by the steering wheel
Deceleration trauma
Accidental falls from great heights
Objects of great weight falling directly onto the sternum
Blast and direct forces applied to the chest
Increased abdominal pressure
Cardiopulmonary resuscitation
In many cases, injuries to the heart lead to immediate death. Typically, the myocardium, pericardium, and the coronary arteries are affected. In blunt trauma, the heart can be compressed between a flexed spine and the sternum; however, shearing forces, twisting, and deceleration trauma have also been described. The mechanically injured heart can be further damaged by hypovolemic shock, arterial hypotension, and resulting myocardial ischemia. In addition, heart function may be impaired by hypoxia from other injuries such as pulmonary contusions, pulmonary lacerations, and pneumothorax as well as multi-organ failure (MOF) (Parmley et al. 1958; Fulda et al. 1991; Orliaguet et al. 2001).
Up to 25 % of deaths from traumatic events are associated with cardiac injuries. The incidence of blunt cardiac injury has risen during the last decades, but early diagnosis and efficient, specific treatment are mandatory and are correlated with increasing survival rates. A major proportion of patients with manifest cardiac injuries die on the scene before they can reach medical treatment. In cardio surgery, new technologies are influencing outcomes, as bypass surgery and the use of intra-aortic balloon devices can assist the cardiac function and thus may help to improve the outcome (Table 2) (Mattox et al. 2012; Co et al. 2011).
Table 2
Cardiac injury – clinical presentation
Acute findings | Subacute findings |
|---|---|
Complete hemodynamic instability | Tenderness and pain along the anterior chest wall |
Congestive heart failure | Dysrhythmias |
Cardiopulmonary arrest | New heart murmur |
Cardiogenic shock | Pericardial friction rub |
Symptoms of pericardial tamponade |
2 Imaging Modalities
2.1 Cardiac Ultrasound (US)
Echocardiography (cardiac US) provides precise evaluation of the existence of pericardial effusions. In addition, small volumes of not more than 25 ml can be detected. Myocardial wall motion and the valvular structures can also be assessed, as well as the left ventricular function. Transesophageal echocardiography (TEE) can also be used to assess the ventricular function in cases of myocardial contusion and was deployed to evaluate the aorta for signs of aortic injury (AI) before reliable CT angiography (CTA) from advanced MDCT scanning became available (Restrepo et al. 2007, 2012). However, TEE is more time-consuming and invasive and is difficult to perform with concomitant injuries, e.g., to the face and cervical spine. Additionally, it is not always available and is operator dependent. Therefore today TEE plays only a minor role in the acute trauma setting.
US findings of acute cardiac injury comprise cardiac wall compression and pulmonary artery compression as well as paradox flow patterns, abnormalities of the ventricular septum, and abnormal swinging motion of the heart itself (Restrepo et al. 2007, 2012).
Alternatively, transthoracic cardiac US can be performed. It is rapid, noninvasive, and efficient. It is reported that even limited training in cardiac US techniques may provide an efficient means of detecting pericardial hemorrhage. Sensitivity is reported to be 90 %, specificity 97 %, and accuracy 96 %. Pericardial emergency ultrasound of the heart is an important component of FAST ultrasound (focused assessment with sonography in trauma) (Mattox et al. 2012; Co et al. 2011).
2.2 Conventional Radiography (CR) of the Chest
Supine conventional radiography (CR) of the chest is still a component of the initial trauma workup in the emergency room. However CR is limited to delineate the full spectrum of injuries to the thorax and heart as well. In many cases, however, signs of pneumopericardium, hematothorax, pneumothorax, and mediastinal widening, due to mediastinal hematoma, can be detected. Imaging quality of supine CR of the chest in the emergency setting is often limited and most of the important cardiac injury patterns cannot be detected (Mattox et al. 2012; Co et al. 2011).
2.3 Cardiac Angiography
Angiography of the coronary arteries (syn. cardiac angiography) is not an established component of a typical trauma-imaging workup in the emergency room. However, it is very sensitive and specific in imaging coronary artery injuries, and it can detect even subtle vascular lesions. In addition, it offers the entire spectrum of opportunities for immediate interventional treatments of vascular lesions. It is indicated in all cases of suspected vascular injury and also when ischemia is suspected with ECG changes after trauma, to evaluate patients for traumatic aneurysms, intima dissections, and vascular thrombosis after trauma. Most of these lesions can be detected and can undergo intermediate interventional treatment.
2.4 Multidetector CT (MDCT)
Many patients with suspected multiple trauma undergo a MDCT from head to toe, so-called whole-body CT (WBCT). MDCT is the imaging modality of choice for the evaluation of all kinds of chest trauma and is highly sensitive and specific for the evaluation of lung injuries, pneumothorax, active hemorrhage, pericardial or myocardial injury, pleural and pericardial effusions, hematothorax, and also cardiac herniation and cardiac luxation. MDCT can also depict valvular injuries and papillary muscle rupture as well as avulsion of the aortic and mitral valve (Linsenmaier et al. 2002; Mirvis).
High-quality MDCT is today available in all major trauma centers, it is widely accepted, and MDCT is today the core imaging modality in the major trauma setting. In thoracic and cardiac imaging, MDCT can detect penetrating foreign bodies, it also depicts the track of penetrating objects, and it allows for initiation of a targeted treatment. MDCT has a high sensitivity and accuracy in the detection of pleural and pericardial effusions or pericardial hemorrhage and tamponade. It detects pericardial and myocardial lacerations and also active hemorrhage from the heart. It also depicts luxation and displacement of the heart and has also a high sensitivity for concomitant mediastinal vascular and lung injuries. Due to its high spatial and timely resolution, it delivers isotropic voxel allowing for the calculation of high-resolution multiplanar reconstructions (MPRs). Today small motion and flow artifacts are now much reduced from prior scanner generations. ECG-gated MDCT scanning is an adjunct to the initial whole-body CT (WBCT) in the acute trauma setting. Contrast medium (CM) is administered in all studies, and an extended CM bolus allows for a contrast filling of the right and left heart and the vascular in- and outflow at the same time. Primary axial reconstruction is performed with the thinnest possible slice thickness (ST) of 0.5–0.625 mm; diagnostic axial images are reconstructed at 1–1.5 mm and coronal and sagittal MPRs at 2–3 mm and VRT as well (Fig. 1) (Mirvis; Korner et al. 2009).
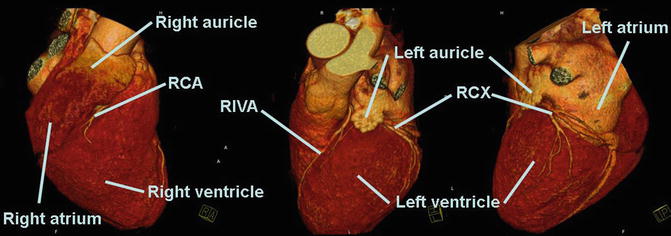
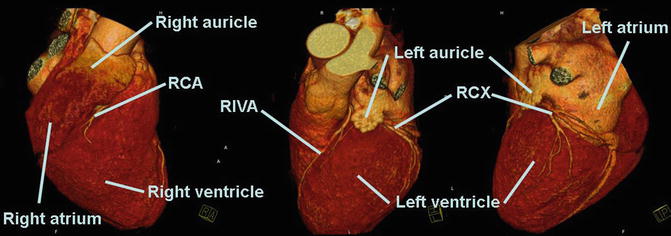
Fig. 1
CT anatomy of the heart ECG-gated cardiac CT in a volume-rendering technique (VRT) for radial display
2.5 Cardiac Magnetic Resonance Imaging (MR)
Cardiac magnetic resonance imaging (MR) has the ability to assess cardiac anatomy as well as cardiac function; it can visualize signs of myocardial ischemia and myocardial infarction (MI). In myocardial contusions, it can depict abnormal cardiac wall motion and abnormal valve function and can detect edema and ischemia of the myocardium. MRI is not useful in the early and acute trauma workup as availability of 24 h/7 days is limited, the exam is complex to be performed, and the patient monitoring is difficult at the same time. However, if indications are given, it is a valuable noninvasive imaging method in addition to MDCT of the acute setting (Co et al. 2011; Korner et al. 2009).
3 Blunt Cardiac Injuries
Minor injuries are so-called myocardial contusions (syn. cardiac contusion); more severe injuries comprise ruptures of the pupillary muscles, valve injuries, injuries to the coronary arteries, and septal and myocardial injuries as well as cardiac rupture. Most common causes of blunt cardiac injury are high-speed motor-vehicle accidents (MVAs), crush or blast injuries, falls from height, and less common, direct violence or direct impact to the chest or abdomen. Also iatrogenic injuries are reported due to cardiopulmonary resuscitation (CPR). A clinical algorithm is available for management of patients after blunt cardiac trauma (Fig. 2).
Fig. 2
Clinical algorithm for management of patient with suspected blunt trauma to the heart. The algorithm distinguishes minor isolated chest trauma from major isolated chest trauma and multiple trauma (El-Chami et al. 2008)
3.1 Myocardial Contusion
Myocardial contusion is best defined as motion changes of the cardiac wall when myocardial infarction (MI) could be ruled out. Clinically it can be suspected in cases of significant chest trauma and persistent arterial hypotension despite volume therapy (Embrey; Kaye and O’Sullivan).
Myocardial contusion has to be differentiated from myocardial infarction which can be clinically difficult to distinguish. In myocardial infarction (MI), symptoms are related to a vascular territory, and the tissue at the risk shows a transition zone when in myocardial contusion the tissue at risk is more confined and has a distinct edge. The incidence of myocardial contusion is reported in a wide range with 10–75 %, probably due to inconsistent findings, and a scientific standard for diagnosis is still missing (Mattox et al. 2012; Co et al. 2011; Symbas; Tenzer).
These injuries are also named under the term myocardial contusion (alternatively, myocardial concussion) and are usually best diagnosed by laboratory testing of isoenzyme MB of creatine phosphokinase (CPK-MB), echocardiography, and ECG. The troponin test is an additional laboratory test (CTNI and CTNT >0.1 μg/l), with increased levels of the protein troponin usually observed in patients with cardiac contusions. Typically, patients only undergo monitoring on intermediate care units (Table 3) (Mattox et al. 2012; Co et al. 2011; Symbas; Tenzer).
Table 3
Cardiac injury – laboratory and ECG diagnosis
Laboratory findings/cardiac enzymes | ECG findings |
|---|---|
Cardiac markers are biomarkers measured to assess heart dysfunction: Myoglobin, LDH-1 isozyme, glycogen phosphorylase isoenzyme BB (GPBB), creatine kinase MB, troponin T and I Creatine kinase MB (CK MB) has turned out to be nonspecific Troponin T: very specific marker for cardiac injury (91 %), but with low sensitivity (31 %) Troponin I shows the best correlation of sensitivity and specificity in different trials. In combination with EKG abnormalities, it exhibits 100 % sensitivity for detection of clinically significant blunt cardiac trauma such as cardiogenic shock, dysrhythmias requiring treatment, or structural cardiac abnormalities related to trauma Levels <1.05 μg/L in asymptomatic trauma patients, indicative of cardiac injuries Levels >1.05 μg/L associated with ventricular dysrhythmias and left ventricular dysfunction The remaining cardiac parameters are not relevant for trauma monitoring | The important role of ECG bases on the fact that electrical instability is an important indicator for blunt cardiac trauma ECG is a quickly available tool for the first survey: Hemodynamically stable patients with normal EKG need no further monitoring Significant electrical disorders are suggestive of cardiac injuries especially the presence of any new bundle branch block Other typical findings: persistent sinus tachycardia (most often), atrial fibrillation, ST depression, ST elevation Limitation: present abnormalities are not pathognomonic markers for diagnostic correlations |
The introduction of the diagnosis cardiac contusion is controversial as clinical importance, incidence, and morbidity and mortality remained controversial. It is accepted that younger patients with ECG abnormalities after trauma should undergo further evaluation. ECG is a clinical indicator in multiple injured patients as significant cardiac disease is relatively rare in young patients after trauma.
When ECG abnormalities occur, they are significant and need further evaluation. Clinical recommendations comprise that patients after thoracic trauma, as long as they are symptom-free, do not need any surveillance or monitoring; in symptomatic patients, intermediate care or telemetry monitoring is considered to be sufficient (Cachecho et al.; Fabian et al.; McLean et al.).
Pathophysiologically there is a wide range of tissue damage in myocardial contusions, from transmural hemorrhage and tissue necrosis to superficial contusions with different extend of tissue loss. The resulting perfusion defects and myocardial dysfunction most likely result from focal contusion and tissue edema when coronary artery disease is not present. The right heart is more affected due to its position next dorsal to the sternum. Clinical findings comprise ECG changes and elevated cardiac enzymes (creatine phosphokinase and serum cardiac troponin) (Allen and Liedtke; Ghersin et al.).
Clinical symptoms can mimic myocardial infarction, including dyspnea and chest pain; the ECG changes are variable and most cases are uncomplicated. However, a progress to an arrhythmia, cardiac dysfunction, hypotension, and low-output failure as well as myocardial rupture can be observed leading to life-threatening cardiac failure.
Abnormal cardiac wall motion is best diagnosed with echocardiography. In the setting of whole-body computed tomography after trauma (WBCT), there are no specific imaging features reported for myocardial contusion so far. Advanced ECG-gated MDCT enables an anatomic workup including CT angiography (CTA) of the coronary arteries. In addition, it allows for a functional assessment of the heart including assessment of the cardiac wall motion in 4D technique and initial reports on myocardial perfusion. Concomitant injuries of the thorax and mediastinum are present in many cases and can deteriorate the clinical situation (Fig. 3) (Embrey; Kaye and O’Sullivan).
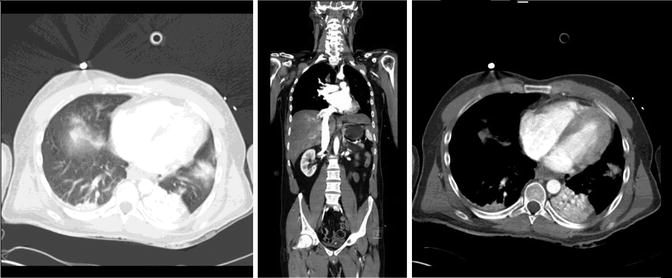
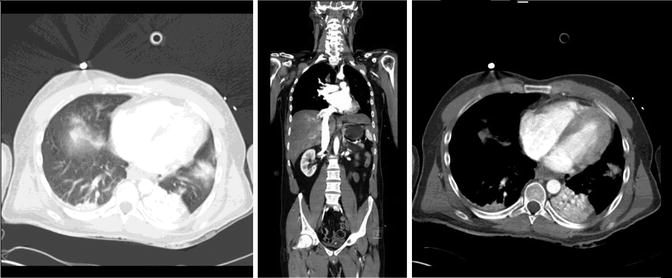
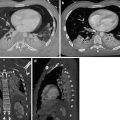
Fig. 3
Myocardial contusion: ungated MDCT of the whole body showing heart dilatation of the right atrium and ventricle, pulmonary contusion and hematothorax, and atelectasis of the left lower lobe. A contrast reflux with retrograde paradox flow in the inferior vena cava (IVC)
Cardiac MR and positron emission tomography (PET) can delineate the possible extend of the hypoperfused myocardium and can be used for further workup if myocardial contusion is suspected (Co et al. 2011; Kaye and O’Sullivan).
3.2 Injuries to the Pericardium
Pericardial tears can differ in size from millimeters to an extent over the entire pericardium. They are most common at the diaphragmatic surface and the left-sided pericardium. Typically they are result of an increased intra-abdominal pressure or the direct impact to the chest and mediastinum (Fulda et al. 1991; Parmley et al.).
Conventional radiography (CR) may show air in the pericardium (pneumopericardium); pericardial injuries can be complicated by diaphragmatic rupture and cardiac herniation from resulting in severe cardiac failure. However CT findings are by far more sensitive and specific.
Pericardial tears and ruptures are rare injuries, with an incidence of only 0.3–0.5 %. They occur with severe deceleration forces or are due to osseous fragment perforation by fractures to the sternum or the ribs. Pneumopericardium is a complication of pericardial rupture; an air collection is located ventral to the myocardium in the pericardial sac. Pneumopericardium is a sign for pericardial injury. The tear itself can be detected by irregular margins of the pericardium, discontinuity, and interposition of fat or long parenchyma. This can be further complicated by cardiac tamponade and compression. Pneumopericardium is always a sign for pericardial injury; the pericardial tear itself can be detected by irregular margins or discontinuity of the pericardium, but also by interposition of fat or lung parenchyma (Restrepo et al. 2007; Farhataziz and Landay) (Fig. 4).
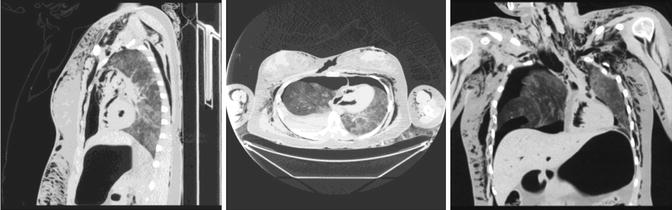
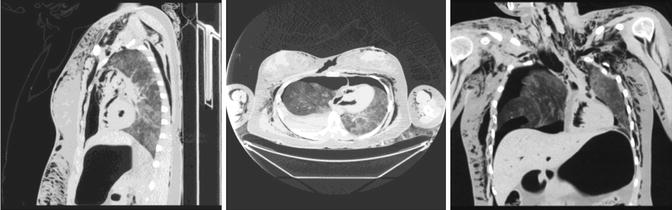
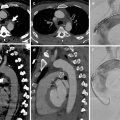
Fig. 4
Pneumopericardium: ungated MDCT showing a pneumopericardium on post-mortem CT (PM CT). There is pathological air collection in the chambers of the heart, pneumomediastinum, soft tissue emphysema, pneumothorax, gastric hyperinflation, and hematothorax
After pericardial injury MDCT can be used to depict pericardial effusions. In the acute trauma setting, every pericardial effusion has to be evaluated for hemorrhage; MDCT can measure the density of effusions in Hounsfield units (HU) and confirm pericardial hemorrhage and tamponade (Restrepo et al. 2007).
Further complications include the displacement of the heart through the pericardial rupture into the mediastinum or thoracic cavity, showing an empty air-filled pericardium on MDCT. As the vascular structures are stretched or also rotated (also described as volvulus), this can lead to immediate compression of the heart and obstruction of the vascular system. Cardiac luxation describes herniation and compression of the heart, which can result in obstruction of the upper venous inflow over the superior vena cava (SVC). Luxation can occur in up to 28 % of pericardial ruptures, and there is a high associated mortality rate of up to 67 %. An ECG allows observation of a change of the heart axis. Cardiac US is of limited value only. MDCT can be used to diagnose heart displacement as well as the compression and deviation of the myocardium and the heart chambers (Fig. 5) (Moront et al.; Bruschi et al.).