Fig. 1
Penetrating tracheal injury secondary to intubation. Supine chest radiograph shows overdistention of the endotracheal cuff (dashed line). Furthermore, left pneumomediastinum (arrows), right heart contour outline (arrowheads), and bilateral pulmonary contusions are also evident (Reproduced with permission from Elsevier)
Internal or non-penetrating injuries may occur secondary to inhalation of noxious fumes or gases, tracheal compression on the rigid vertebral column, or due to aspiration of liquids or foreign bodies. When the tracheobronchial tree is occluded by foreign bodies or there is a sudden chest compression with closed glottis, as in crush or steering wheel injuries, an explosive rupture may occur (Stark 1995).
During recent years, an increase in traffic accident has caused an increase in blunt tracheobronchial injuries, and the most common non-penetrating injury mechanism is the motor vehicle accident. The exact mechanism of intrathoracic, tracheobronchial disruption from non-penetrating trauma is unknown, but these injuries include longitudinal lacerations of the distal trachea or near the carina (usually within 2.5 cm), with complete or partial disruption of the main bronchus (more common, right bronchus) and other lobar bronchi.
2 Mechanism of Injury
The causes of airway injuries are divided into blunt trauma, penetrating trauma, or iatrogenic rupture and into neck (larynx and cervical trachea) or thoracic lesions (chest trachea and bronchi).
Blunt trauma at the neck can cause a hyperextension mechanism that results in tracheal tears and paramedian vertical fractures of the larynx and trachea or lead to complete laryngeal–tracheal separation (Dougenis 2002; Milner 2008); another mechanism is direct blow to the neck injuring the thyroid or cricoid cartilages but also the tracheal rings due to compression against the vertebral column. In a vehicle accident, both mechanisms happen: neck hyperextension from sudden deceleration and direct impact of the neck to the steering wheel or the dashboard: this is the “padded dashboard syndrome” (Nelson 2007) (Fig. 2). Other mechanisms are consequent to improper use of seat belts as a direct blow to the neck in front-on collision or by the sudden increase of intratracheal pressure while the glottis is reflexively closed (Rathlev et al. 2007).


Fig. 2
Cervical tracheal injury secondary to blunt trauma. Parasagittal reformatted 16-row MDCT image depicts displacement of the endotracheal cervical tube (arrowheads) through a wall defect consistent with a cervical tracheal injury. This finding was confirmed by bronchoscopy (Reproduced with permission from Elsevier)
The usual mechanisms of tracheobronchial disruption are (1) excessive pressure in the bronchial tree when the glottis is closed, causing airway blowout at the point of the greatest diameter, i.e, the carina (Laplace’s law); in this case, the rupture occurs when the intraluminal pressure exceeds the elasticity of the membranous trachea and bronchi; (2) decrease in the anterior–posterior chest diameter with increase in the lateral diameter; when the lungs are pulled out laterally, the main bronchi and carina become disrupted; and (3) severe and sudden deceleration giving rise to sheer forces that disrupt the airway at the points of relative fixation such as the cricoid cartilage and the carina, similar to the mechanism of traumatic injuries of the thoracic aorta (Huth et al. 1997). In most of cases, probably a combination of these three mechanisms causes the airway lesion (Kiser et al. 2001).
Tracheobronchial injuries are rare in the pediatric population, because the pediatric patient’s chest wall is more elastic than the adult’s chest wall (Balci et al. 2004). This elasticity decreases when the age increases due to the progressive ossification of the rib cage and the development of increased intercostal muscle tone (Grant et al. 1998). Spontaneous tracheal rupture in a pediatric patient can be secondary to paroxysmal coughing or pernicious vomiting. Non-penetrating tracheobronchial injuries less commonly are secondary to fractures of the regional skeleton of the upper thorax, particularly of the first three ribs.
According to data published by Burack et al., even though only 1 of 188 patients who did not die rapidly on the scene or after the admission to the emergency department had sustained a tracheal injury, it is important for the radiologist to identify this kind of lesion, since missed diagnosis may have fatal consequences (Burack et al. 2007).
Acute injuries of the tracheobronchial tree may be iatrogenic in origin: tracheal intubation, tracheotomy, bronchoscopy or other per-oral intervention (tracheal or esophageal stent placement), and surgery (Paraschiv 2014). The most common cause of iatrogenic tracheobronchial rupture is tracheal intubation, especially when it is performed in stressful, emergency conditions. The site of injury is, preferentially, the posterior membranous wall (Massard et al. 1996; Marty-Ane et al. 1995).
Post-intubation tracheobronchial rupture is an emergency condition, secondary to tube tips placed excessively, cuff over inflation that produces excessive stretching of the membranous wall or by endotracheal tube-repositioning maneuvers without deflating the cuff (Figs. 1 and 3).
Fig. 3
Penetrating tracheal injury after intubation. (a) At the level of the thoracic inlet, chest CT scan shows overdistention of the endotracheal cuff (arrowheads). (b) Corresponding chest radiograph clearly depicts the same CT finding (arrowheads). (c) Surgical specimen shows endotracheal cuff herniation through the injured tracheal wall (arrows) (Reproduced with permission from Elsevier)
Bulging of tracheal wall until tracheal rupture can be a complication of hyperinflated cuff that can lead to ischemic necrosis and subsequent tracheomalacia or strictures, particularly if its diameter exceeds 1.5 times the tracheal diameter (Chen et al. 2001b).
Factors favoring post-intubation tracheal rupture are the lack of experience of the anesthetist; use of double-lumen endotracheal tubes, or a too-thick endotracheal tube; presence of chronic pulmonary disease; and congenital tracheal anomalies.
The conditions most commonly associated with injuries of the trachea in intubation procedure are female gender, age over 50 years old, double-lumen tube, and excessive pressure in the endotracheal cuff (Paraschiv 2014).
A rare complication of blunt chest trauma is the tracheoesophageal fistula that may occur to focal necrosis of the esophageal wall and lead to perforation into the trachea (Stark 1995).
3 Terminology and Clinical Issues
The natural history of blunt tracheobronchial injuries may vary from one patient to another. Many patients immediately die at the trauma scene for acute respiratory insufficiency or within 2 h for associated injuries. A small proportion of patients may present in a delayed fashion, usually within 4 weeks of injury, with hemoptysis, pneumonitis, or both, complicating an obstructed airway (Scaglione et al. 2006). Only rarely do patients present with a healed airway injury years later, typically with dyspnea or the diagnosis of asthma.
Tracheal or main stem bronchi injuries are often not recognized initially, due to its rare incidence, lack or subtle clinical manifestations, and the much more overt clinical signs of other more common associated injuries (Wiot 1983).
After an acute airway injury, the common symptoms are dyspnea and respiratory distress, hoarseness, or dysphonia. The most common signs of airway injuries are subcutaneous emphysema, pneumomediastinum, pneumothorax, and hemoptysis. These symptoms and signs are nonspecific for this kind of injury. Cervical– thoracic subcutaneous emphysema is the most common finding (65–87 %) (Paraschiv 2014). Pneumothorax, due to the splitting of the mediastinal pleura, occurs in 17–70 %, and the most specific characteristic is the inability to re-expand the lung after chest tube positioning.
A rare clinical manifestation is Hamman’s sign, a crackling sound, synchronous with heartbeats, may be heard over the precordium produced by the heart beating against air-filled tissues (Wong and Knight 2006).
4 Imaging
4.1 Radiological Signs
Radiological studies improve the diagnosis of tracheobronchial injuries, especially when the clinical findings are subtle and in the first hours after the injury.
Standard or supine chest and cervical X-rays may reveal early suggestive signs as deep cervical or mediastinal emphysema (92–100 %), pneumomediastinum (85 %), or pneumothorax (40 %). These are the most common findings in radiographs. When the pneumomediastinum or pneumothorax is conspicuous, in supine position, the signs of “continuous diaphragm” or “deep costophrenic sulcus” can be appreciated (Fig. 4) due to the redistribution of the air preferentially accumulated over the diaphragmatic structure and anterior to the lungs, respectively (Scaglione et al. 2002).
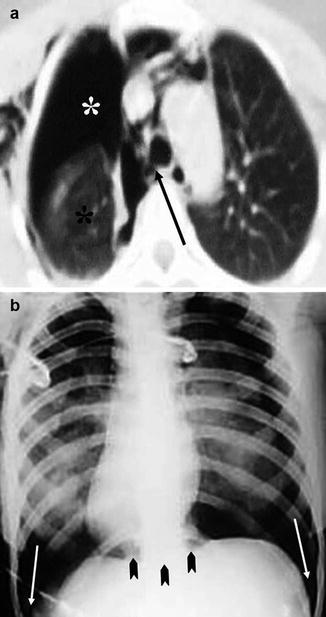
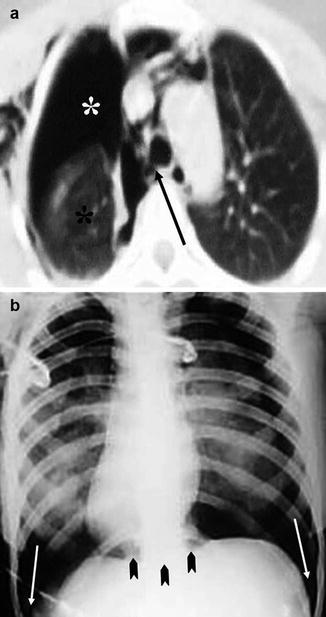
Fig. 4
Blunt bronchial injury (a) CT scan shows right-sided subcutaneous emphysema, pneumothorax (white asterisks), and pneumomediastinum. The right lung, which is partially collapsed, is detached from the main bronchus (arrow) and drops posteriorly (black asterisk) in the right hemithorax—the “fallen lung” sign. (b) Supine chest X-ray shows the “deep costophrenic sulcus” sign (arrows) and the “continuous diaphragm sign” (arrowheads) (Reproduced with permission from Elsevier)
Other signs suggestive for tracheobronchial injuries include tracheal deformity and overdistended endotracheal balloon cuff (Figs. 1 and 3). On lateral radiographs of the cervical spine, a high position of the hyoid bone associated to deep cervical emphysema can be an important indication of tracheal transection (Polansky et al. 1984).
Defect in tracheal contour, deviation of the endotracheal tube tip, and tube’s cuff overdistention or protrusion beyond the edge of the tracheal wall (Chen et al. 2001b) are more specific signs of tracheobronchial rupture.
In some cases, the overdistention of balloon precedes the pneumomediastinum of several hours and may be the first and “small” signs of tracheobronchial injury. A cuff diameter greater than 2.8 cm is an indirect sign of tracheal tear (normal diameter of trachea is 2.7–2.8 cm), excluding other causes: balloon is located in the esophagus, patient is chronically intubated, or preintubation of tracheal enlargement (Rollins and Tocino 1987).
A tracheobronchial lesion may be also seen as a “bayonet sign” when a sharp angulation of the normal tracheal column or of the bronchial lumen occurs (Scaglione et al. 2002).
The “fallen lung” sign may be appreciated when the air leak through the injured tracheobronchial wall leads to lung collapse below the hilus, indicating complete rupture or transection of the main bronchi. This sign was first described by Oh et al. in 1969 and Kumpke in 1970.
A bronchocele/pneumatocele may also be detected after blunt trauma as a consequence of compression–decompression trauma of the chest causing rupture of the small airways and is seen as round radiolucent areas on a chest X-ray (Scaglione et al. 2002; Barbick et al. 2005) (Table 1).
Table 1
X-ray findings
Specific |
Defects in tracheobronchial contours |
Deviation of the endotracheal tube tip |
Tube’s cuff protruding beyond the edge of the tracheal wall |
“Bayonet” sign
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|