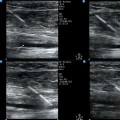
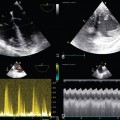
59 Significant advancements have been made in the use of ultrasound technology since its inception in the early 1950s.1 These advances have revolutionized the practice of critical care medicine. Currently, clinicians in the intensive care unit (ICU) have at their disposal a tool at the bedside that augments the physical examination and is safe, portable, noninvasive, and readily available. Ultrasound technology uses sound waves, and through reflection, refraction, and attenuation of these ultrasound beams, image acquisition occurs, thus limiting the patient’s exposure to radiation, unlike chest radiography and computed tomography.2,3 The lack of radiation exposure also allows multiple sites to be evaluated repeatedly with minimal risk to the patient (Chapter 1). Bedside ultrasound enables immediate integration between the clinical scenario that requires investigation and the operator. This allows a more focused, goal-directed evaluation of hemodynamically unstable patients with immediate interpretation of data and implementation of personalized therapy.4 On review of the literature, the time needed to obtain information during bedside ultrasound evaluation is very brief given the magnitude of information obtained during each evaluation (Table 59-1). Appropriate, focused examinations can be performed as part of routine practice on teaching rounds. TABLE 59-1 Time Needed to Obtain Information during Bedside Ultrasound Goal-directed echocardiography enables qualitative assessment of left and right ventricular size and function, identification of pericardial effusion and evaluation for tamponade physiology, measurement of internal vena cava (IVC) diameter, and assessment of respiratory variation to determine preload responsiveness.17,20,21 Critical care ultrasound (CCU) facilitates bedside detection of pleural fluid and pneumothorax and can be used to guide thoracocentesis for diagnostic-therapeutic purposes, as well as other invasive procedures (e.g., placement of thoracostomy tubes, paracentesis, abscess drainage). CCU guides arterial and central venous cannulation and facilitates the placement of peripherally inserted central catheters and hemodialysis catheters.22 CCU detects venous thrombosis14 and free intraperitoneal and pericardial fluid (focused assessment with sonography for trauma) and facilitates the evaluation of patients for acute renal dysfunction23–25 and volume status. CCU can be used in conjunction with the physical examination to improve accuracy and clinical utility and enhance the teaching of various physiologic principles.26 It can provide immediate feedback to confirm or refute the physical findings. For example, within a few minutes of using CCU the cause of life-threatening conditions triggering hypotension can be elucidated or excluded from the differential diagnosis. If a resident hears a typical murmur of mitral regurgitation on physical examination, this can be confirmed within minutes with bedside echocardiography. Immediate feedback enhances learning.
Integrating ultrasound into critical care teaching rounds
Overview
Safety
Time efficiency
Investigation
Average Time
Lung ultrasound
2-3 min5,6
Internal jugular vein cannulation (mean start until vessel located)
9.5-13.8 sec7–10
Subclavian vein cannulation (mean start until vessel located)
26.8 sec11
Doppler ultrasound
11.7-15 min12–14
Transthoracic echocardiography
6-10.5 min15–17
Inferior vena cava measurements
5-5.8 min18,19
Critical care ultrasound is clinically useful
Teaching tool
Radiology Key
Fastest Radiology Insight Engine