Fig. 18.1
Branches of thoracic spinal nerve roots (Reprinted with permission from eMedicine.com, 2010. Available at: http://emedicine.medscape.com/article/1143675-overview)
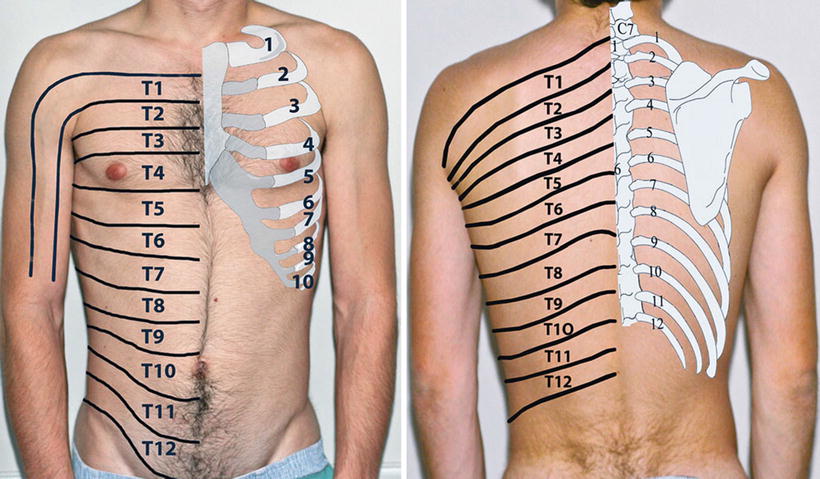
Figs. 18.2 and 18.3
Dermatomes of thoracic nerve roots and relation to ribs
Ribs
True ribs – first to seventh, connect directly to the sternum through costosternal cartilages.
False ribs – eight to tenth, so-called because their cartilages do not reach the sternum directly but instead attach to the rib immediately above.
Floating ribs – 11th and 12th, only reach to cover the back and do not have attachment to the sternum.
Costochondral joints – the articulation between the rib and the cartilage connecting them to the sternum. They start at the first rib, just lateral to the sternum. As they go inferior, they become more lateral till the tenth rib; it is almost at the anterior axillary line.
Nerves
As the thoracic nerve roots emerge from the intervertebral foramen, they immediately split into the ventral rami that form the intercostal nerves and the posterior rami (see Fig. 18.1). Anterior branches form the gray and white rami communicantes of the thoracic sympathetic chain. The posterior rami innervate the zygapophyseal (facet) joints, muscles and skin of the thoracic midline, and paraspinous area of the back.
The intercostal veins, arteries, and nerves (VAN) travel for the most part in the costal grove, protected from direct trauma with the nerve being most inferior on the edge of the rib. After exiting the foramen, the intercostal nerves are near the middle of the intercostal space between the parietal pleura and the inner side of the intercostal muscles. As the nerve approaches the angle of the rib, the nerve then emerges between the internal intercostal muscle layer and the outer portion of the innermost intercostal muscle to its location on the costal groove.
Small collateral nerve branches develop as the intercostal nerve progresses anteriorly, innervating the intercostal muscles and the ribs. At about the midaxillary line (MAL), the lateral cutaneous nerve arises. The lateral cutaneous nerve splits into posterior and anterior branches that innervate the skin of the chest wall from the scapular line to midclavicular line. The intercostal nerve continues anteriorly within the costal groove between the internal intercostal muscle layer and the outer portion of the innermost intercostal muscle, but as it progresses anteriorly, it once again emerges internal to the innermost intercostal muscle. As intercostal nerves approach the sternum, they emerge as the anterior cutaneous branches, innervating the anterior chest.
Thoracic nerve roots – branch into the dorsal primary rami and the anterior rami which become the intercostal nerves.
Dorsal primary rami – innervate the posterior midline and paraspinous muscles and skin.
Intercostal nerves – innervate distinct band-like segments of muscles (myotomes) and skin (dermatomes).
Collateral branches – arise from the intercostal nerves to innervate the intercostal muscles and ribs.
Lateral cutaneous nerve branches – arise in the MAL and divide into anterior and posterior branches to innervate the skin of the majority of the torso.
Anterior cutaneous nerves – divide into medial and lateral branches to innervate the skin of the anterior torso
Cross innervation – as the nerves travel distally, they overlap so that even total loss of a single nerve root is unlikely to produce a noticeable sensory loss. To develop a complete sensory loss, usually you have to block two to three intercostal nerves.
Special Considerations
1.
First, intercostal nerve arises from the ventral ramus, but a portion of the ventral ramus goes on to join the brachial plexus.
2.
Second, intercostal nerve also supplies a small branch of the ventral ramus to the brachial plexus.
Dermatomal Distribution
Dermatome distribution maps of intercostal nerves have long been published from a variety of sources and should always be viewed as approximations [11, 12]. In particular as noted above, a single intercostal nerve block seldom results in a total anesthesia of single dermatome due to cross innervation; however, dermatome charts can be used as a guide in selecting level of placement of intercostal nerve blocks (see Figs. 18.2 and 18.3).
Local Anesthetic
Local anesthetic choices are similar as in other nerve block procedures, the most common being lidocaine or bupivacaine. For single-shot INB, a volume of 3–5 mL is usually more than adequate per level injected. Total dose however should be monitored to reduce the risk of systemic toxicity. Alkalinization of the local anesthetic for intercostal nerve blocks has been found to be of little clinical benefit [13]. The use of epinephrine has been proposed as a possible increased safety factor by constricting local vessels and reducing uptake or by producing a tachycardia as a warning sign of accidental intravascular injection. However, other studies have called this into question and shown increased hemodynamic changes compared to other types of nerve blocks [14].
For continuous INB, an infusion of 0.25 % bupivacaine at 2 mL/h is usually adequate.
Clinical Applications
INB has been shown to be useful for a variety of anesthetic and analgesic uses in the distribution of the torso. Among these are:
1.
Post-thoracotomy pain
2.
Post-rib fracture pain
3.
Cancer pain
4.
Mastectomy and breast surgery pain
5.
Shingles pain
6.
Intercostal neuralgia
7.
Costochondritis
8.
Abdominal wall pain
Studies have shown that INB for post-thoracotomy pain offers advantages in preserving effort-dependent pulmonary function compared to opioid analgesia [15, 16].
The first three intercostals also innervate sensation portions of the upper arm and axilla, while the lower intercostals from T6 to T12 innervate the muscles of the upper abdomen and overlying skin [17]. Therefore, intercostal nerve blocks at the appropriate level can easily control symptoms in the affected region, allowing for decreased dependence on opioid analgesics. This can be useful in cases where one needs to avoid respiratory depressant or mental status changes.
Effective perioperative analgesia with continuous INB also has been demonstrated to reduce the incidence of chronic post-thoracotomy neuralgia [18]. While bupivacaine single-shot INB is reported to last longer than lidocaine, no significant difference has been reported in the outcome between infusions of lidocaine or bupivacaine for continuous infusions [19].
Trauma to an intercostal nerve by thoracotomy can lead to either pain or a sensory loss over the skin of the affected nerve or pain assisting in identifying the level injured. Similarly, trocar placement during laparoscopic procedures such a cholecystectomy can lead to similar problems. Numerous studies also have looked at use for a variety of conditions as noted above. Most studies are anecdotal, as noted in a recent case report on treatments for costochondritis [20].
Technical Tips
Some studies have suggested that a short-beveled needle is likely to be safer and more accurate for INB [21].
Continuous intercostal catheter analgesia is a more efficient way of performing INB, allowing a longer therapeutic effect. For most applications, an epidural catheter kit is the most convenient to use.
Use of elastomeric infusion pumps has been shown to be a safe and effective adjunct in postoperative pain management after thoracotomy [22].
Paravertebral Nerve Block
The thoracic paravertebral space is a somewhat triangular space that is laterally continuous with the intercostal space [23, 24]. Anatomical borders are:
Medial border – vertebral body, intervertebral disk, and spinal foramina
Posterior border – transverse process, superior costotransverse ligaments, and ribs
Anterior border – parietal pleura
Intercostal nerves, their collateral branches and posterior primary rami, and the thoracic sympathetic chain all pass through the paravertebral space, making it an ideal site for blockade of the various afferent nociceptive nerve impulses [25].
The mechanism of action of the PVNB is intercostal nerve block via the paravertebral spread of local anesthetic [26]. Spread of a mean of six dermatomes (range, five to seven) has been demonstrated by injection of methylene blue at thoracotomy and infusion of contrast medium in postoperative patients [26]. Techniques described have included blind placement [27, 28], by neurostimulator [29], by loss of resistance, by and ultrasound.
Clinically, PVNB is comparable with epidural block in respect to pain relief but without the well-known side effects of the epidural analgesia [30]. PVNB is therefore seen as a useful technique for pain control of breast, thorax, and abdomen, and many have considered it the technique of choice [31–33]. While one prospective study failed to that show a single-shot PVNB was superior to continuous wound infiltration [34], the technique of continuous catheter PVNB is gaining popularity. The ability to perform this effectively at bedside with ultrasound guidance [35] also simplifies the ability to perform this procedure in a greater variety of settings.
The effectiveness of PVNB injections with local anesthetic and steroids in acute herpes to prevent postherpetic neuralgia has been studied and been shown to be useful [36].
Complications
Complication rates for INB are low. They are reported to include:
1.
Intravascular systemic injection with subsequent local anesthetic toxicity
2.
Pleural puncture and pneumothorax
3.
Hematoma
4.
Neural injury
5.
Infection
6.
Total spinal anesthesia
Many studies have documented the higher plasma levels of local anesthetic concentrations after intercostal nerve block [37] relative to other nerve block locations. However, the incidence of local anesthetic toxicity is low.
Pneumothorax, one of the most commonly thought of complications, is actually also rare. One study in surgical patients looked at over 100,000 individual nerve blocks and found no severe systemic toxic reactions, and the incidence of pneumothorax was 0.073 % [38]. Another study in patients who received INB for rib fractures due to trauma showed a higher rate of 1.4 % [39], still a low rate considering the higher risk of pneumothorax in rib fractures.
Rare complications can include total spinal anesthesia. This may occur by inadvertent injection into a dural cuff extending outside the intervertebral foramen [40, 41]. This has been reported with paravertebral block injections and catheter placement [42], and similarly, neurolytic injections have led to total spinal cord injuries.
Procedure Description
Intercostal Nerve Block
Standard monitors are applied.
Patient is place in a comfortable prone position.
Sedation with a combination of midazolam (0–3 mg) and fentanyl (0–150 μg).
Identify the posterior spinous process by palpation and mark on skin.
Draw a paramedian line at the lateral edge of the paraspinous muscles.
Palpate for the inferior edge of each rib at this line and mark the skin at this site at the previously marked line.
Inject local anesthetic into the skin at each one of the planned injection sites.
Connect a 4-cm 25-gauge needle to a control syringe with the local anesthetic of choice.
Use the nondominant hand and index and middle fingers to again palpate the inferior edge of the rib at the planned injection site (Fig. 18.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree