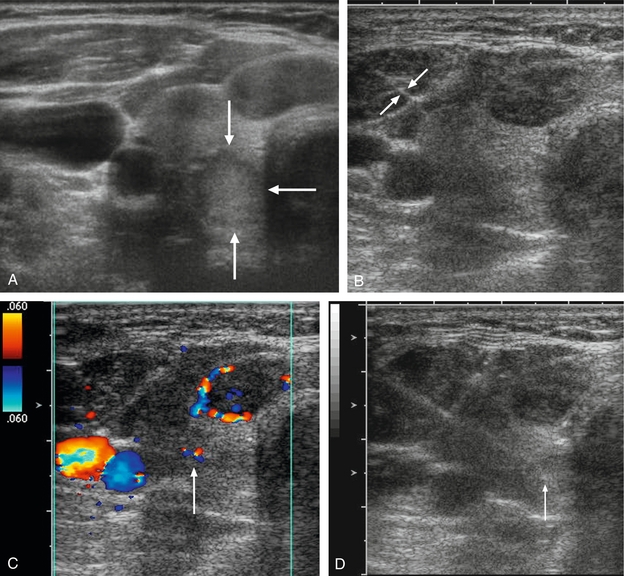
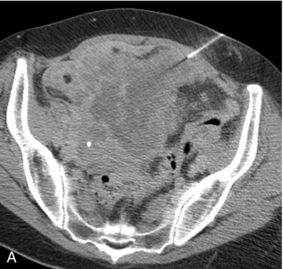
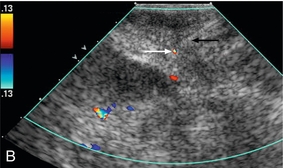
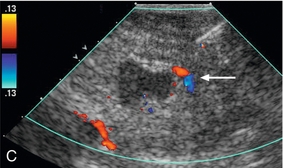
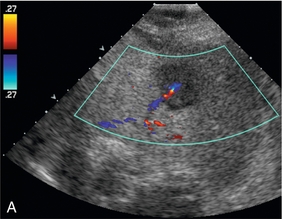
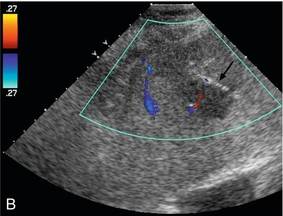
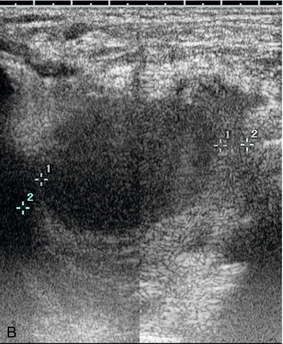
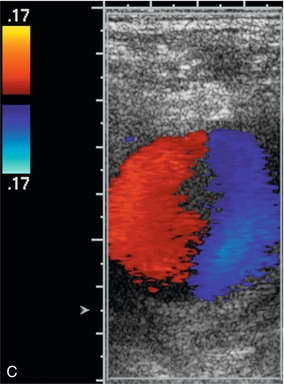
Chapter 16 Ultrasound is the preferred modality for performing imaging-guided interventional procedures. Advantages over other modalities such as CT include real-time guidance allowing precise needle placement, portability, relatively low cost, and lack of ionising radiation.1,2 The addition of colour Doppler has been shown to be of great utility during interventional procedures. The primary benefit is the enhanced ability to visualise blood vessels during needle placement. Other advantages include improved needle visualisation and timely identification of procedural complications (Box 16-1). Specific Doppler applications can be divided into pre-procedure planning, intra-procedural guidance, and post-procedure monitoring. The most important use of colour Doppler ultrasound in interventional procedures is visualisation of blood vessels along the needle trajectory. This allows the vessels to be avoided as the needle is advanced, thereby minimising the risk of bleeding.3 Alternatively, in some situations such as arteriography or venography, colour may be useful to localise vessels for puncture. The focus of this chapter will be the use of colour Doppler for non-vascular interventional procedures. The addition of colour Doppler to imaging guidance has been shown to reduce the risk of bleeding in both percutaneous liver and kidney biopsies.4–6 Good guidance technique routinely incorporates colour Doppler imaging immediately prior to needle placement anywhere in the body. Specific vessels (Table 16-1) should be identified during certain common interventional procedures (Fig. 16-1). TABLE 16-1 Specific Vasculature Structures That Doppler US can Identify and Help Avoid When Performing Biopsies, Aspirations, or Drainages in Various Body Regions FIGURE 16-1 Thick slab coronal MIP image from a CTA shows the positions of the internal mammary (black arrows), superior epigastric (white arrows), and inferior epigastric (block arrows) arteries. These must be identified and avoided during procedures involving an anterior approach. In fine needle aspiration of thyroid nodules and lymph nodes, colour Doppler is used to avoid the internal jugular veins and carotid arteries and their major branches (Fig. 16-2). In the chest, colour Doppler ultrasound has been shown to improve vessel visualisation during transthoracic needle aspiration biopsies.7,8 During mediastinal biopsy, not only should the great vessels be visualised, but a specific search for the internal mammary arteries and veins must be performed. Intercostal vessels can be avoided by advancing the needle directly over ribs, as the vessels run along the inferior margin of the ribs. However, a search for intercostal vessels with colour Doppler is warranted, especially if the needle must be directed close to the inferior margin of the rib in order to target the lesion. FIGURE 16-2 Thyroid fine needle aspiration biopsy. (A) Grey scale US image shows an isoechoic posterior right thyroid nodule (arrows). (B) The proximal needle (arrows) is visualised within hypoechoic muscle but the tip is difficult to identify as it enters more echogenic tissue. (C) Colour Doppler image shows colour flow at the tip of the needle (arrow) as it is gently jiggled back and forth, as well as demonstrating the internal jugular vein and carotid artery. (D) After the needle tip and vessels are identified, colour Doppler is turned off and the needle tip (arrow) is seen in the nodule while avoiding the vessels. Ultrasound-guided percutaneous liver biopsy can be performed using a sub-xiphoid approach to access the left lobe, or an intercostal approach into the right lobe. Although both techniques are acceptable, some authors favour a sub-xiphoid approach to avoid damage to intercostal structures and avoid traversing the pleura.9 However, a recent study reported a 0.8% (6/776) rate of significant bleeding complications from percutaneous US-guided liver biopsy, all from the left lobe approach.10 Four of the six cases were attributed to superior epigastric artery injury. These vessels lie approximately 4 cm from midline at the level of the xiphoid process. Therefore the superior epigastric arteries must be identified and avoided during left lobe biopsies or any other procedure in the epigastric region. If they cannot be visualised, a midline approach is preferred in order to avoid these vessels. Likewise, the inferior epigastric arteries should be identified during any puncture in the lower abdomen or pelvis, such as paracentesis (Fig. 16-3). Additionally, as paracentesis is often performed in cirrhotic patients with portal hypertension, colour Doppler should be also used to identify enlarged abdominal wall varices. FIGURE 16-3 CT- and US-guided pelvic mass biopsy. (A) CT was used for initial superficial needle placement during percutaneous biopsy of a large heterogeneous pelvic mass. (B) Colour Doppler was then utilised and revealed the needle trajectory (black arrow) was directed towards the inferior epigastric artery (white arrow). Slight repositioning allowed for the needle to be advanced avoiding the artery as shown in (C). Also note the tumour vessel (arrow) that was identified and avoided. During liver biopsy colour Doppler can decrease bleeding risk by visualisation and avoidance of major intrahepatic vasculature. Fine needle aspiration biopsy under US guidance is an established technique for distinguishing between bland and malignant portal vein thrombus. Colour Doppler improves visualisation of the thrombus by identifying flow surrounding it or within it, and can guide needle placement directly into the thrombus without traversing patent portions of the portal vein and helping avoid the adjacent hepatic artery.11 Colour Doppler is useful to distinguish hepatic vessels from bile ducts when performing transhepatic cholangiography. Colour and spectral Doppler US can identify tumour neo-vascularity. It is important to avoid such vessels as they lack a normal coagulation response and have a higher propensity for bleeding (Fig. 16-4). Puncture of these vessels can result in aspiration of a large amount of blood during FNA which will degrade the specimen and reduce diagnostic yield. FIGURE 16-4 Hypoechoic liver lesion biopsy in a patient with metastatic breast cancer. (A) Colour Doppler image shows a tumour vessel along the posterior aspect of the liver mass. (B) Colour Doppler image showing the biopsy trajectory (arrow) in the anterior portion of the mass in order to avoid this vessel. A less common but highly important use of colour Doppler ultrasound is the identification of vascular lesions such as pseudoaneurysms and arteriovenous fistulas (AVFs) prior to performing an intervention. On grey scale US, a pseudoaneurysm can appear to be a cystic lesion or fluid collection and aspiration or drainage may be requested. Puncture of such a lesion could result in a life-threatening haemorrhage. This scenario may be encountered in the setting of acute pancreatitis, where pseudocysts are common. However, splenic (or any branch of the celiac axis) artery pseudoaneurysm can mimic a pseudocyst and must be excluded before performing an intervention. Colour Doppler US can easily identify the vascular nature of these lesions by demonstrating the characteristic swirling blood in a ‘yin-yang’ pattern (Fig. 16-5). The use of colour Doppler in the treatment of pseudoaneurysms is discussed elsewhere in this book. FIGURE 16-5 A 65-year-old man with a history of melanoma and neck mass. (A) Non-contrast CT through the neck reveals a soft tissue attenuation mass in the superior mediastinum displacing the trachea. A CT-guided biopsy was requested, however, the lesion was first studied with US. (B) Grey scale US reveals a hypoechoic mass, however colour Doppler (C) shows the classic ‘yin-yang’ pattern of a pseudoaneurysm and biopsy was deferred. Arteriovenous fistulas have been reported as a complication of renal biopsies in 3–18%.12 Although often asymptomatic, they are of particular importance in renal transplant recipients who often undergo multiple biopsies. These lesions must be identified and avoided prior to repeat biopsy in order to minimise the risk of serious bleeding. Arteriovenous fistulas are rarely seen on grey scale US but can be easily identified on colour Doppler. Tissues surrounding the fistula vibrate due to the high-velocity blood flow and may show a flash of colour noise – the equivalent of a palpable thrill or audible bruit. The feeding artery will demonstrate aliasing unless the pulse repetition frequency is increased. Spectral Doppler tracings show high-velocity, low-resistance waveform in the feeding artery, and high-velocity, arterialised flow in the draining vein (see Chapter 10, Fig. 10-19). Real time visualisation of the needle tip is an advantage of US-guided intervention. Generally, the needle should only be advanced when the tip can be seen in order to ensure successful access to the target lesion and to avoid inadvertent puncture of adjacent structures. Unfortunately, it can be difficult to clearly delineate the needle tip and that is a common source of frustration when performing US guided interventions. Visualisation of the needle is particularly difficult when it traverses tissues that have high echogenicity similar to that of the needle (fatty livers), when the needle is advanced parallel to the insonating beam, and with small-gauge needles. Many techniques have been described to improve needle tip visualisation, such as roughening the surface of the needle tip, Teflon coating, and the so-called ‘pump manoeuvre’ where the needle stylet is gently moved back and forth within the needle. The addition of colour Doppler US is a useful adjunct to improve needle visualisation.11,13 Colour Doppler detects motion of any kind and therefore the movement of the needle or inner stylet is more easily detected and the needle localised (Fig. 16-2).
Interventional and Intraoperative Doppler
Introduction
Pre-Procedure Planning
AVOIDANCE OF BLOOD VESSELS
Procedure site
Vessels to identify
Neck/thyroid
Carotid arteries/jugular veins
Mediastinum
Internal mammary artery
Chest/upper abdomen
Intercostal vessels
Left liver/epigastric region
Superior epigastric artery
Abdomen/pelvis
Inferior epigastric artery and abdominal wall varices

IDENTIFICATION OF VASCULAR LESIONS

Intra-Procedural Applications
IMPROVED NEEDLE VISUALISATION
Interventional and Intraoperative Doppler