Fig. 5.1
MRA images showing the internal carotid artery segments (from wikipedia.org, courtesy of Behrang Amini). C1, cervical segment. C2, petrous segment: this is the horizontal segment located within the temporal bone. C3, the lacerum segment, which is a small segment that starts from the petrous apex, passing above the foramen lacerum, and is covered by the trigeminal ganglion. C4, the cavernous segment, also known as the carotid syphon, is subdivided into three segments, the posterior vertical, horizontal and anterior vertical. Its branches are the meningohypophyseal trunk and the inferolateral trunk. C5, the clinoid segment, terminates where the ICA passes into the subarachnoid space. C6 is the ophthalmic segment, which extends to the origin of the PcoA: its branches are the ophthalmic artery and the superior hypophyseal artery. C7 is the communicating segment which extends from the origin of the PCoA to the ICA bifurcation into the MCA and ACA. Its branches are the AChoA and PCoA
Common anatomical variants of the ICA are:
Aberrant ICA (which presents clinically as a retrotympanic pulsatile mass) in which the ICA runs posterolaterally in the hypotympanum;
Persistent stapedial artery, vestigial branch, which passes between the cochlear promontory and the stapes and is associated with the absence of the foramen spinosum;
Persistent trigeminal artery (Fig. 5.2) is a relatively common carotid basilar anastomosis and runs parallel to the 5th cranial nerve.
The ACA is divided into three segments: A1, A2 and A3 (Fig. 5.3).
Common anatomical variants are:
Absence or hypoplasia of the A1 segment;
Azygous ACA in which the A2 segments are fused in a single ACA.
The MCA is divided into 4 segments: M1, M2, M3 and M4 (Fig. 5.4).
Common anatomical variants are:
Early bifurcation or trifurcation;
MCA duplication.
Posterior Circulation
The posterior circulation is supplied by the terminal segment of the VA, the basilar artery and its branches (Fig. 5.5).
The VA is divided in 4 segments: proximally to distally, V1, V2, V3 and V4.
V1, V2 and V3 are extracranial segments. V4 is the intradural segment which starts where the vertebral artery pierces the dura and runs superomedially, behind the clivus. The VA joins the contralateral VA to form the basilar artery. V4 branches off from the posterior inferior cerebellar artery (PICA).
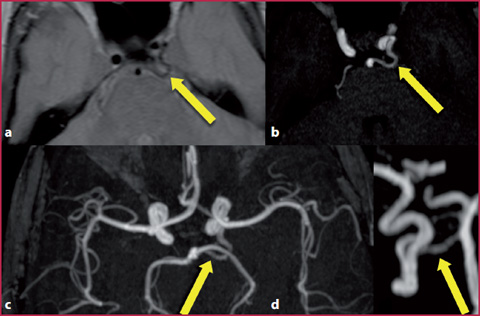
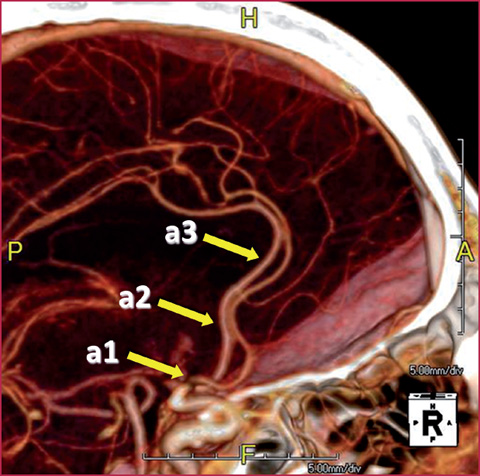
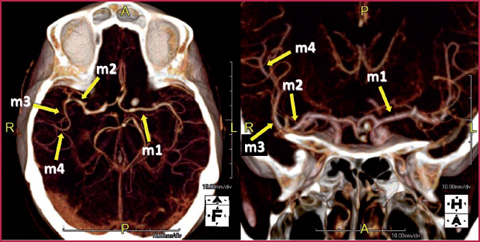
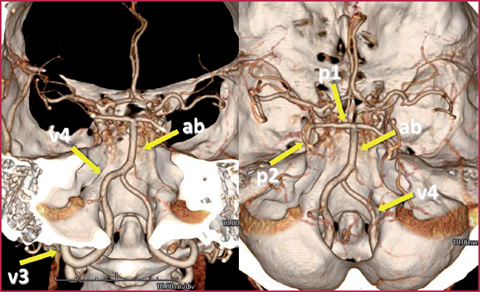
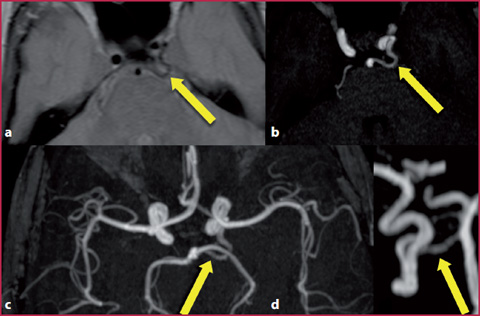
Fig. 5.2
Patient with a persistent trigeminal artery. a Axial proton density image; b source image taken from the 3D TOF; c MIP reconstruction from the MRA 3-D TOF; d selective reconstruction of the ICA and basilar artery. There is a supernumerary artery (yellow arrow), linking the ICA and the basilar artery (carotid basilar anastomosis)
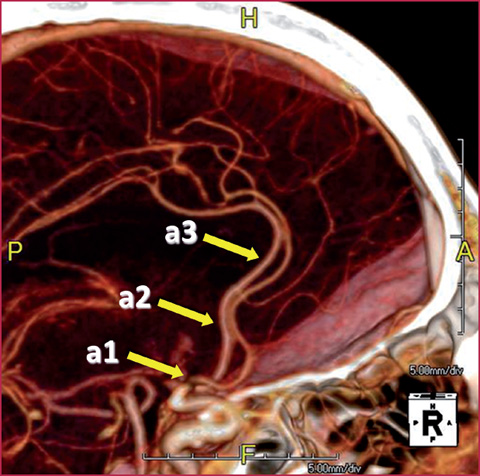
Fig. 5.3
CTA showing the segments of the anterior cerebral artery. a1 is the communicating segment which runs from the ACA origin to the origin of the ACoA and runs above the optic nerve. a2 is the post-communicating segment which runs from the origin of the ACoA to the origin of the frontopolar artery and branches off from the orbitofrontal artery. a3 is the segment distal to the frontopolar artery which branches off from the pericallosal and callosomarginal arteries
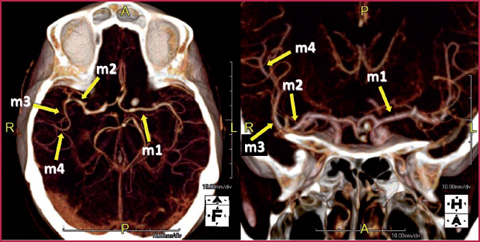
Fig. 5.4
CTA showing the segments of the middle cerebral artery. m1 is the horizontal segment which extends from the ICA to the sylvian fissure running in a lateral direction. It bifurcates or trifurcates before the sylvian fissure. It branches off from the perforating vessels and the anterior temporal artery. m2, the insular segment, is characterized by the vessels originating after the bi- or bifurcation. m3, the opercular segment originates from the sylvian fissure passing through the temporal and frontal operculi. m4 is the deep cortical segment characterized by the branches originating from the sylvian fissure and extending to the cerebral convexity
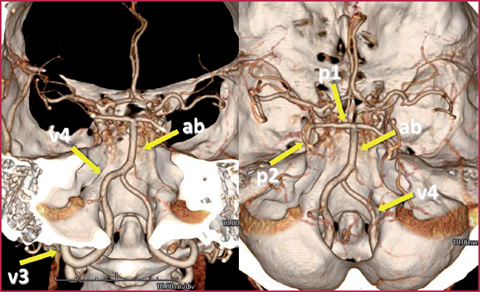
Fig. 5.5
Volume rendering reconstructions of brain CTA. The terminal segments of the vertebral artery (v3 and v4), the basilar artery (ba) and the proximal segments of the posterior cerebral arteries are shown (p1 and p2)
The BA runs in the prepontine cistern anterior to the brainstem and originates from the confluence of the two vertebral arteries. It bifurcates into two posterior cerebral arteries (PCA) at the level of the interpeduncular cistern. The branches of the BA are the anterior inferior cerebellar artery (AICA) and the superior cerebellar artery (SCA).
Common anatomical variants are fenestrations and duplications.
The PCA is divided into 4 segments named P1, P2, P3 and P4.
P1 is the precommunicating segment which runs from the basilar artery to the PCoA.
P2 runs in the ambient cistern and branches off from the posterior medial choroidal artery and posterolateral choroidal artery.
P3 is the quadrigeminal segment which runs in the quadrigeminal cistern posterior to the midbrain.
P4 is the calcarine segment which terminates in branches leading to the occipital and parietal lobes.
Circle of Willis
Circle of Willis The circle of Willis (COW) is a cerebral anastomotic ring formed by the branches of the ICA and VA, located the base of the brain. The following arteries contribute towards the formation of the COW: 2 ICA, 2 A1, ACoA, 2 PCoA, 2 PCA, and the BA. The branches of the COW are the perforating lenticulostriate arteries, the thalamoperforating arteries, and the thalamogeniculate arteries.
Anatomical variants of the COW are very common, seen in up to 60% of patients. The most common variants are:
A1 segment hypoplasia or absence;
fetal origin of the PCA;
absence of the ACoA.
Venous System Anatomy
The intracranial venous system has two components: the dural venous sinuses and the cerebral veins (Fig. 5.6).
The dural venous sinuses are large veins covered by dura mater invaginations which form their walls. The superior sagittal sinus is a median structure localized in the outer margin of the falx cerebri; it originates from the foramen cecum anteriorly and terminates at the level of the torcular posteriorly. The inferior sagittal sinus is located in the inferior margin of the falx cerebri and communicates posteriorly with the vein of Galen, from which the straight sinus originates, directed to the torcular. The transverse sinuses originate from the torcular, run laterally, become sigmoid sinuses at first and then internal jugular veins at the level of the jugular foramina. The cavernous sinuses are located laterally to the sella turcica and contain the ICA and the 6th cranial nerve.
The cerebral veins are thin-walled venous structures located in the subarachnoid space directed toward the dural sinuses. Venous drainage is typically centrifugal, except for the deep brain structures. Most of the brain is drained by the cortical veins.
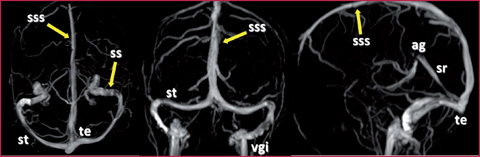
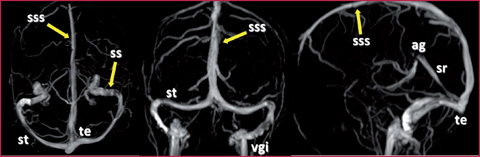
Fig. 5.6
Anatomy of the intracranial veins, MIP reconstructions obtained from a 3-D phase contrast study. ss, sigmoid sinus; sss, superior sagittal sinus; st transverse sinus; vgi, internal jugular vein; sr, straight sinus; ag, Vein of Galen; te, torcular Herophili
5.2 5.2 CTA and MRA Technique
Vascular imaging of the central nervous system is performed by CTA, MRA and conventional angiography (DSA).
Since the evaluation of the intracranial circulation is frequently performed together with the vessels of the neck, refer to the neck protocol for a discussion of the technique. Some technical tips are useful for the evaluation of the intracranial circulation.
For CTA, a fast imaging scanner similar to the one used for the carotid arteries should be used. The region of interest (ROI) used for the bolus tracking can be placed in the distal extracranial ICA segment, easily identifiable in the precontrast scans.
For the MRA , the most frequently used sequences are 3-D time of flight [3D-ToF Magnetic Resonance Angiography (MRA)] and T1-weighted contrast-enhanced MRA [Contrast-Enhanced (CE)-MRA].
Unlike body imaging, ToF is usually the most commonly used technique. CE- MRA is preferentially used in high-flow arterial disease, in the evaluation of a stenotic arterial segment, in the evaluation of AVM, and in the post-treatment follow-up of brain aneurysms.
For the visualization of the intracranial veins, the most commonly used technique is the 3D Phase-Contrast (3DPC).
5.3 5.3 Brain Aneurysms
Clinical Features and Diagnosis
Intracranial aneurysms are classified according to their morphology.
The berry aneurysms are focal dilations, caused by a genetic susceptibility to mechanical stress on the vessel walls. They originate in the arterial bifurcations where hemodynamical stress is higher.
Fusiform aneurysms are caused by atherosclerosis and are characterized by arterial wall ectasia caused by damage to the tunica media.
Blister aneurysms are small focal dilations, typically located in the supraclinoid ICA.
In 95% of cases, the intracranial aneurysms originate from the COW (90% anterior circulation = ICA, PCoA, ACoA and MCA; 10% posterior circulation = BA bifurcation and PICA) (Fig. 5.7).
The most common clinical presentation is the subarachnoid hemorrhage (SAH) (Figs. 5.8-5.9), which is associated with very severe headache. Typically the patient is a young adult, complaining of the worst headache of his/her life.
Imaging and Dictation Tips
When facing a typical clinical scenario, or when a non-enhanced CT of the brain demonstrates a SAH, it is necessary to perform a CTA or an MRA to localize the aneurysm.
Get Clinical Tree app for offline access
The SAH appears as a subarachnoid hyperdensity on the CT scan or a hyperintensity on the T2 FLAIR sequence.
A subarachnoid T2 FLAIR hyperintensity is associated with other possible etiologies such as meningitis or pial amyloidosis.
The localization of the SAH suggests the location of the aneurysm: interhemispheric SAH > ACoA, sylvian fissure > MCA, suprasellar cistern > ACoA.
In 95% of cases, a perimesencephalic subarachnoid hemorrhage is not related to aneurysm rupture, but to other etiologies.
When describing an aneurysm, the exact location, the morphology, the size of the sac, the size of the neck, the direction of growth, and the presence of intra-aneurysmal thrombosis are features recommended for inclusion in the dictation.
It is important to establish the presence of perforating vessels arising from the dome of the aneurysm, for which the DSA has a higher sensitivity compared to MRA or CTA.
When an aneurysm is found, look for other aneurysms.
Carotid C4 segment aneurysms are difficult to see on the CTA due to the concurrent opacification of the cavernous sinus where the C4 segment is located.
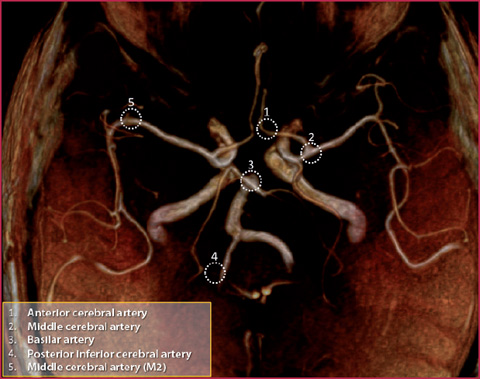
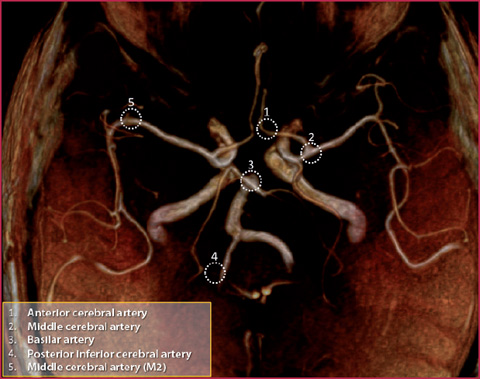
Fig. 5.7
Schematic view of the circle of Willis and preferential locations of intracranial aneurysm
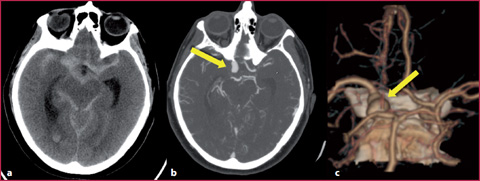
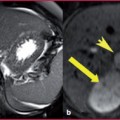
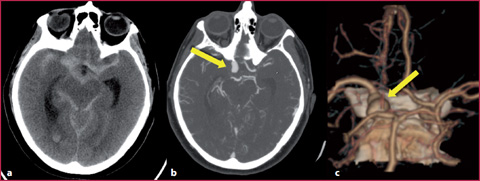
Fig. 5.8
Patient with subarachnoid hemorrhage and carotid ophthalmic aneurysm. a Brain CT. b CTA. c Volume rendering reconstructions. There is a subarachnoid hemorrhage in the suprasellar and perimesencephalic cistern and a right carotid ophthalmic aneurysm (yellow arrow




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree