64 Intraneural Injections
Safety issues for ultrasound in regional anesthesia practice have been raised by several authors.1,2 Tremendous controversy and debate surround this field, particularly in regard to the subject of intraneural injection.
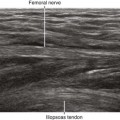
A large number of seemingly innocuous intraneural injections imaged with ultrasound have been reported.1,3,4 In these cases, although nerve expansion from injection was reported, no loss of nerve border integrity was detected. All these intraneural injections were believed to be low pressure. Most of these harmless intraneural injections have been detected by retrospective review of ultrasound recordings of blocks and were not recognized online in real time. All these intraneural injections were in nerves with high collagen content and polyfascicular architecture. There have been no reported cases of intraneural injections in monofascicular nerves, which would more likely result in functional damage.
We have yet to establish the sonographic signs of intraneural injections that produce functional damage. To date, there has been only one published report of sonographic nerve imaging following nerve injury resulting from needle injection.5 Sonography cannot distinguish between subepineurial and subperineurial needle tip placement. Subperineurial injection is thought to be more harmful.6
Intraneural injections have been dichotomized into high-pressure and low-pressure types.7,8 The low-pressure type has not been associated with injury and may be common in clinical practice. Collateral damage may be the mechanism of adjacent fiber injury after high-pressure injection (nerve blast injury from explosion with surrounding nerve fascicles damaged).
Ultrasound may be able to identify some factors that influence the chance of nerve injury during regional anesthetics. Nerve echotexture may play an important role in perioperative nerve injuries. Polyfascicular nerves contain more protective connective tissue than monofascicular nerves. The outcomes after monofascicular nerve injuries are probably worse than after polyfascicular injuries.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree