Case presentation
A 22-month-old female presents with cough and congestion for the past 5 days. She was noted to have persistent fever to 102 degrees Fahrenheit. She has been taking oral fluids well, but this has decreased over the past few days, although she still has good urine output. There has been no vomiting, diarrhea, or concern for foreign body ingestion/choking episodes. Her physical examination reveals a febrile child (101.5 degrees Fahrenheit) with a respiratory rate of 25 breaths per minute, a heat rate of 140 beats per minute, and a pulse oximetry reading of 85% on room air. She is alert and vigorous but with mild respiratory distress. There are scattered crackles and wheezing throughout her lung fields, but especially at the left lower lobe. She has moderate intercostal retractions without stridor or grunting. The remainder of her examination is unremarkable.
Imaging considerations
Plain radiography
This is often the first-line imaging modality in patients with concern for a pulmonary process, usually pneumonia. Atelectasis on plain radiography may be difficult to distinguish from a lobar consolidation that may be seen with other processes, such as pneumonia. There are radiographic features that can assist with the differentiation of atelectasis and consolidation. Compared to pneumonia, atelectasis is a process of volume loss and is associated with signs of volume loss such as a shift in the normal position of fissures or pulmonary vessels, a mediastinal shift toward the side of the atelectasis, or unilateral diaphragmatic elevation. While atelectasis can involve any lobe of the lungs, the right and left lower lobes and the right middle lobe are frequent sites of atelectasis, especially in patients with asthma. Plain radiography does not expose the patient to significant amounts of ionizing radiation compared to other ionizing modalities (e.g., computed tomography [CT]). Two views of the chest are recommended.
Ultrasound (US)
US is an emerging imaging modality in many pediatric imaging applications. There are some reports using US to detect atelectasis, particularly in the neonatal population, which have shown promise, but US is not typically a first-line imaging modality. ,
Computed tomography
CT can detect atelectasis but is not employed as a first-line imaging modality in general.
Imaging findings
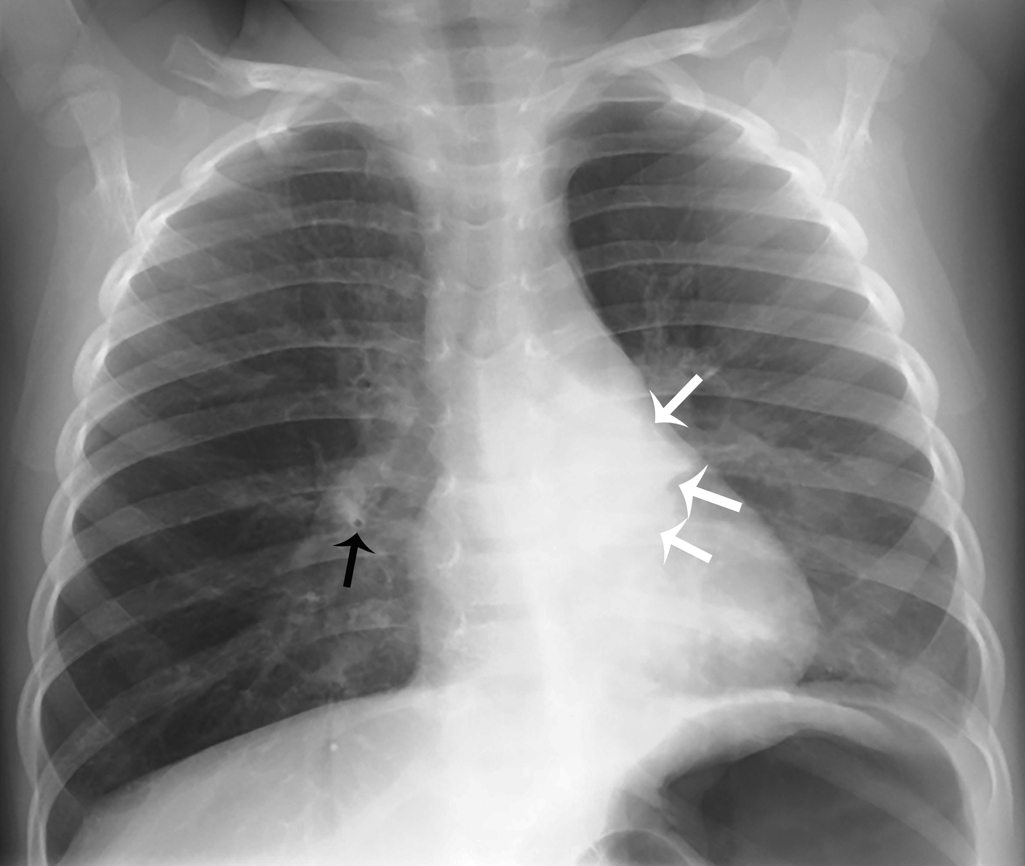
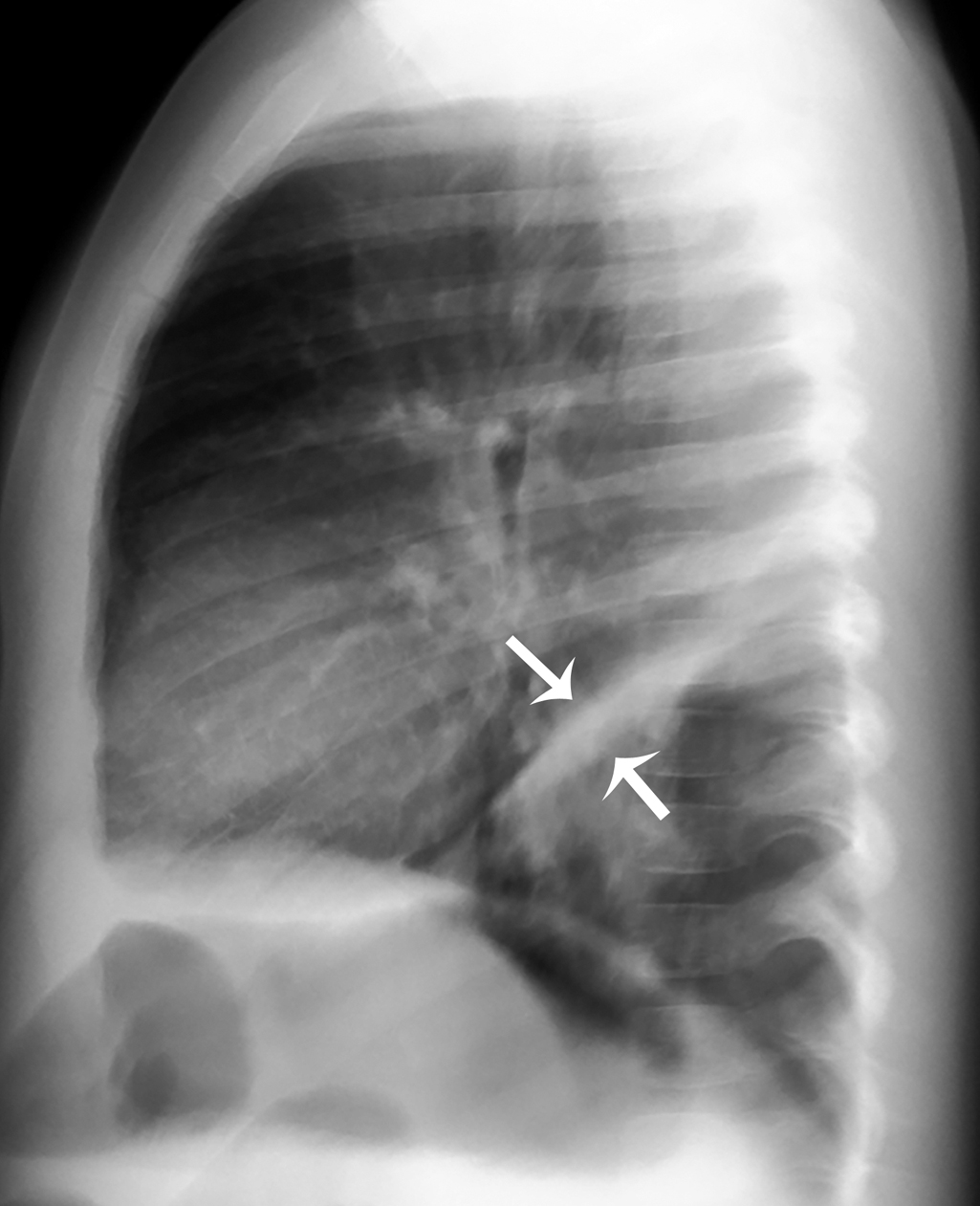
Plain radiography of the chest was obtained. Here, a two-view (posterior-anterior and lateral) study is provided ( Figs. 38.1 and 38.2 ). The examination demonstrates increased parahilar interstitial markings and peribronchial thickening bilaterally. There is consolidation in the retrocardiac left lower lobe, with angular borders, that has a bandlike appearance on the lateral view, an appearance consistent with atelectasis. There is no effusion or pneumothorax. In light of the history, radiographic appearance, and clinical exam, these findings are consistent with atelectasis due to airway disease rather than pneumonia.
Case conclusion
The child was placed on high-flow nasal cannula oxygen with improvement of her symptoms. She had vigorous nasal suctioning performed. Due to her hypoxia and respiratory distress, she was admitted to the hospital for monitoring and supportive care. After several days, she improved and was able to be discharged with close monitoring and follow-up.
Pediatric atelectasis has various etiologies. These can be categorized as: ,
- 1.
Airway obstruction—either from exogenous causes (such as an airway foreign body or recurrent aspiration) or endogenous causes (mucous plugs in cystic fibrosis or infectious processes, such as pneumonia, bronchiolitis, or ciliary mobility syndromes).
- 2.
Compression of lung parenchyma—due to chest masses (either primary or due to metastasis), cardiomegaly, pneumothorax, pleural effusion, hemothorax, or neuromuscular diseases (such as spinal muscular atrophy).
- 3.
Surfactant deficiency—as can be seen in pulmonary edema, submersion injuries, and acute respiratory distress syndrome.
A common cause of atelectasis in the pediatric population is mucous plugging associated with an infectious process. The clinical presentation of atelectasis can be nonspecific but often is dependent on the underlying process. For example, in bronchiolitis, fever, wheezing, rhonchi, and crackles are usually present in some degree. Although none of these findings are specific for atelectasis, the presence of focal wheezing or diminished breath sounds can be found and can be suggestive of atelectasis. A thorough history and physical examination can assist the clinician in determining the most probable etiology of atelectasis.
Special mention should be made of right middle lobe syndrome, originally described by Graham to describe atelectasis from compression of the right middle lobe bronchus due to peribronchial lymphadenopathy. , Findings similar to right middle lobe syndrome have been reported in other sections of the lung as well. , The precise prevalence is unknown, but this entity is more commonly found in the preschool-age population. Right middle lobe syndrome should be suspected when patients present with chronic or persistent cough, wheezing, or recurrent/persistent “pneumonia” in the right middle lobe. Interestingly, this entity is frequently overlooked by physicians, and patients often have been treated with multiple courses of antibiotics prior to diagnosis. Right middle lobe syndrome, commonly seen in pediatric asthma patients, is most commonly due to bronchial wall inflammation and plugging in the right middle lobe with persistent atelectasis. , Radiographic findings are often misinterpreted as pneumonia and treated as such, although antibiotics are not indicated. Chest radiography is the first-line imaging modality for investigating middle lobe syndrome; CT can be utilized as a secondary imaging study to investigate the patency of the bronchial apparatus, evaluate for bronchiectasis, as well as assess for any causes of extrinsic compression, such as adenopathy or masses, or endobronchial lesion such as mass or foreign body. While the role of US in the investigation of middle lobe syndrome remains to be defined, magnetic resonance imaging has emerged as an imaging option. Management is dependent on the underling etiology of the middle lobe syndrome and often involves subspecialty consultation, particularly with pediatric pulmonology. The outcomes of patients with middle lobe syndromes are overall favorable, although long-term outcome data are lacking. , There are reports of up to one-third of patients having residual respiratory symptoms, including mild obstructive airway disease. , ,
Treatment of atelectasis is dependent on the underlying disease process. Patients with asthma, cystic fibrosis, and underlying chronic illnesses are managed with appropriate medications and treatments appropriate to the underlying disease process. Chest physiotherapy is another method that has been employed, especially in the inpatient setting, to help relieve atelectasis and improve pulmonary mucous clearance. , There are few published studies evaluating the management of pediatric atelectasis, although various modalities, such as nebulized medications and intrapulmonary percussive therapy, in addition to chest physiotherapy, have been investigated. Patients with persistent atelectasis should have a pediatric pulmonology consultation and flexible bronchoscopy should be considered. , There are entities (e.g., endobronchial tumors) that can present with persistent atelectasis that require further investigation beyond plain radiography. ,
For comparison, several cases are presented here:
A 6-year-old girl with a history of asthma presented with two separate episodes of fever, cough, and wheezing, 5 months apart. At her first presentation, opacity and volume loss were noted in the right lower lobe on chest radiograph, consistent with right lower lobe atelectasis. When she was again symptomatic 5 months later, chest radiograph shows the right lower lobe to be re-expanded and normal, but there is opacity and volume loss in the left lower lobe, consistent with left lower lobe atelectasis. Note the similar appearance of atelectasis in either lower lobe, as both lower lobes characteristically collapse inferiorly and medially ( Figs. 38.3 and 38.4 ).











