Case presentation
A 7-year-old male is brought in for evaluation. A few hours prior to presentation, he was jumping up and down on a couch when he jumped off, landing on his right leg. He states he heard a “pop” and then began to experience pain and difficulty with ambulation secondary to the pain. There is no reported loss of consciousness; he denies neck pain, back pain, hip pain, weakness, numbness, or other symptoms.
His physical examination reveals an afebrile child who is complaining of right lower leg pain. His heart rate is 91 beats per minute, respiratory rate is 20 breaths per minute, and blood pressure is 118/62 mm Hg. There is mild swelling to the anterior surface of the midshaft of the right tibia and fibula. There is no obvious deformity. There is no abrasion, laceration, or ecchymoses. His anterior tibial and posterior tibial pulses are intact. He has no pain, swelling, or tenderness to the ipsilateral hip, knee, ankle, or foot. He has normal range of motion at these joints. He is grossly neurologically intact. There is no back tenderness, crepitus, step-off, or deformity.
Imaging considerations
Plain radiography
Plain radiographs typically suffice when assessing acute tibial injuries in children and include anterior-posterior (AP) and lateral views. These should incorporate the entire length of the lower leg and include both knee and ankle.
Computed tomography (CT)
This modality is rarely indicated for midshaft fractures. Tibia or fibular fractures that involve the knee (e.g., tibial plateau) or ankle joint may require use of non-contrast CT to evaluate the extent of the fracture.
Magnetic resonance imaging (MRI)
This modality is not indicated in the initial evaluation of tibia or fibula fractures. In instances where the fracture may involve the knee or ankle joint, MRI may be helpful to evaluate associated ligamentous or meniscal injuries.
Imaging findings
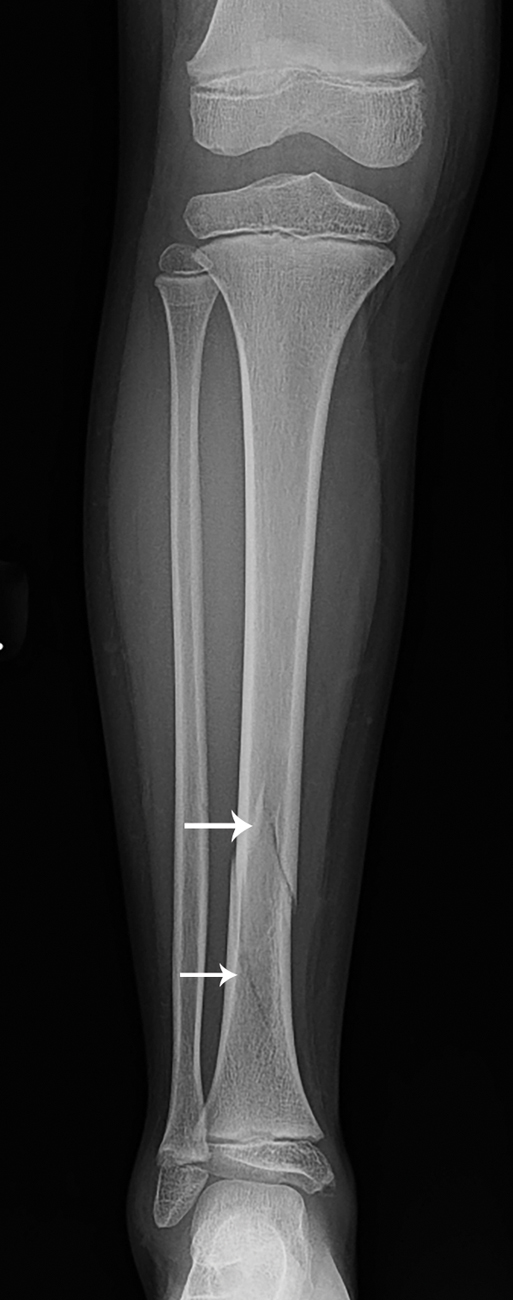
Two-view imaging of the right tibia and fibula was obtained. There is a nondisplaced spiral fracture of the distal tibia with an intact fibula, with visualized joints that are normal and no abnormal bone density; the visualized portions of the knee and foot appear normal ( Figs. 67.1 and 67.2 ).

Case conclusion
Pediatric Orthopedics was consulted and recommended application of a posterior long leg splint, with follow-up in 1 week, since this injury was an isolated, nondisplaced tibia fracture. Strict return precautions were provided and included symptoms of compartment syndrome. Follow-up imaging several months later demonstrates a progressively healing right distal tibia fracture noted in stable alignment ( Figs. 67.3 and 67.4 ).


Tibial shaft fractures are the third most common fracture in children—only fractures of the femur and forearm are more prevalent. , Approximately 30% of cases of tibial fracture have an associated fibula fracture. Adolescent patients are more likely to have combined fractures of the tibia and fibula than other pediatric age groups. ,
A few unique types of pediatric tibia and fibula fractures are important to identify:
Transverse fractures of the tibia/fibula result from a direct blow, and while they are frequently seen in sports injuries, they are also the most common type of long bone fracture associated with nonaccidental trauma.
Bowing fractures are caused by axial loading and may be subtle on radiographs.
Buckle fractures occur when compressive forces lead to buckling of the cortex. Findings on radiographs may be subtle, especially on the AP view.
Stress fractures present as gradual onset of pain and limp and are much more common in older adolescents and young adults. Only 9% occur in children younger than 16 years old, 32% in adolescents aged 16 to 19 years old, and 59% in patients over 20 years old; the proximal third of the tibia is the most often region affected. Radiographs may be normal or may show limited cortical changes or subperiosteal bone formation.
Isolated fibula fracture s may also occur when there is a direct blow to the lateral lower leg; however, prior to diagnosis, it is important to closely examine the distal tibial physis, as concomitant fractures to this location are frequently present.
Spiral (toddler’s) fracture/oblique fractures often occur with minor trauma. These fractures are frequently not seen on lateral radiographs, and the appearance of the fracture on AP view can also be subtle and difficult to visualize. Internal oblique views may also aid in identifying the fracture, although sometimes the fracture can only be visualized over a week after the injury, when bone resorption at the fracture site, periosteal reaction and callous have developed. In this case, the lower leg should be immobilized and made non–weight bearing until repeat imaging is performed. Such fractures commonly occur in the distal half to third of the tibia. Although operator dependent, extremity ultrasound has also been described as a possible imaging modality. Ultrasound may show a hypoechoic hematoma along the tibial cortex or elevated periosteum indicative of a fracture, despite negative radiographs.
Spiral fractures should be considered suspicious for nonaccidental trauma when they occur when the patient is too young to walk or cruise. Pathognomonic findings for abuse include metaphyseal fractures that can be seen as corner fractures and bucket handle fractures.
Treatment of tibia fractures is dependent on several factors. Consultation with a qualified pediatric orthopedic surgeon is appropriate if there are questions regarding management. There are accepted parameters with respect to angulation, displacement, translation, and degree of shortening that guide surgical versus nonsurgical treatment. There are myriad surgical intervention techniques that are available for use; which technique is utilized is largely individualized to each patient and clinical situation. Surgical intervention is most often indicated for patients with open fractures, children who are difficult to cast or are at risk for compartment syndrome (such as obese children), segmental fractures, or fracture patterns that are not able to be well controlled with casting. One study examining closed reduction versus operative management of closed tibia fractures found no difference in outcome, but patients with associated fibula facture or more severe initial fracture displacement (>20%) were more likely to fail closed reduction treatment. As a general rule, combined tibia and fibula fractures, displaced Salter-Harris type I–III fractures, and Salter-Harris type IV fractures mandate immediate orthopedic consultation. Nondisplaced Salter-Harris type I–III fractures of the tibia may be managed conservatively with immobilization and timely pediatric orthopedic follow-up (usually within 1 week).
Distal fibular fractures are commonly reported in pediatric patients, and the majority of these are Salter-Harris type I and II injuries or distal avulsion injuries; more severe Salter-Harris Classification fractures (i.e., III–V) rarely occur as isolated injuries. Isolated distal fibula fractures are stable and usually can be treated with immobilization. Interestingly, the traditional management of casting for several weeks has been challenged, given the low likelihood of complications associated with these injuries. Options that have been explored include a walking cast/boot, ankle bracing, and elastic stockinettes, along with crutch use; patients managed with these have been shown to have good outcomes, faster return to activities, and overall improved satisfaction.
If surgical intervention is not indicated, casting can be accomplished in the emergency department setting utilizing procedural sedation (previously known as “conscious sedation”). Use of fluoroscopy is helpful to ensure proper alignment after reduction and cast application. Many authors recommend admission for observation after reduction to ensure appropriate pain control and to monitor for the development of compartment syndrome, although this is often institution dependent. , Compartment syndrome is not common in the pediatric population compared to the adult population, and the risk of this complication is even lower in children under the age of 8 years. , , Reported rates of compartment syndrome in pediatric patients are between 0.2% and 8%, although the rate is lower in preadolescent patients. , , , Patients with certain injury mechanism histories appear to be at higher risk for the development of compartment syndrome: high-energy mechanisms (for example, skiing accidents, falls from significant height, and motor vehicle accidents), significantly displaced fractures, the presence of an associated fibula fracture, and open fractures. , One study has suggested that children under the age of 12 years old with closed, minimally displaced, tibia-only fractures that resulted from a low-energy mechanism can be discharged if pain is adequately controlled, careful return precautions are given, and timely follow-up is ensured.
For comparison, several other cases are provided:
A 14-year-old male presented to the Emergency Department with right leg pain and swelling after jumping from a horse, landing on his right leg ( Figs. 67.5 and 67.6 ). He had no other injury. His examination demonstrated skin dimpling at the site of the presumed fracture; this dimpling can be seen on the images, which demonstrate an acute, oblique fracture of mid tibial shaft and a transverse fracture of mid fibular shaft. Pediatric Orthopedics was consulted and the fracture was reduced and splinted. IV antibiotics (cefazolin) were administered. He was admitted to the hospital and underwent intramedullary nailing without complication.











