Case presentation
A 2-year-old female is brought for evaluation for right leg pain. The child was jumping in a trampoline house and fell on her right leg. The parents, who accompany the child, did not witness the mechanism by which the child injured her leg, but they state that the child was on the trampoline with several other children, the oldest of whom is 9 years old and is with the patient and her parents. The family reports that all children were bouncing vigorously when the child’s right leg became caught in a gap between the pads. After this event, the patient had pain with ambulation, which localized to the right lower leg. There are no other historical concerns, such as emesis, loss of consciousness, neck pain, or back pain.
The child appears comfortable and is interactive. She has vital signs appropriate for her age. Her examination is unremarkable, except for tenderness over the distal portion of her right lower leg. There is no edema or deformity. The patient is grossly neurovascularly intact. There does not appear to be any neck, hip, or back pain.
Imaging considerations
Plain radiography
Plain radiography is the initial imaging modality of choice in children with musculoskeletal injury. Exposure to ionizing radiation is low and this resource is widely available. Sedation is not required. A two-view (anteroposterior [AP] and lateral) study should be obtained, but consideration should be given to utilization of an oblique view, as some fractures may be better visualized on this projection. Comparison views of the injured and noninjured extremities are typically not necessary and are not routinely obtained; however, in some cases, comparison views may be helpful if there is a finding that is questionable for injury. Note that toddler’s fractures can be subtle on plain radiography, and images can be normal even in the setting of a fracture.
Fractures in nonambulatory children or children in which a given history is not compatible with either physical examination or imaging findings should prompt concerns for nonaccidental trauma. In these children, appropriate imaging, including a skeletal survey and, if indicated, neuroimaging, should be obtained, as recommended by the American Academy of Pediatrics and other organizations.
Other imaging modalities
Interest in the utilization of ultrasound as an imaging modality to detect fractures has grown over the past decades. Advantages of this modality are availability and lack of ionizing radiation. However, this modality is operator dependent, requiring expertise in its use and interpretation of findings. As such, ultrasound use may be limited in detecting fractures, particularly subtle injuries. Other imaging modalities, including computed tomography and magnetic resonance imaging, are not indicated in the acute work up of a suspected toddler’s fracture.
Imaging findings
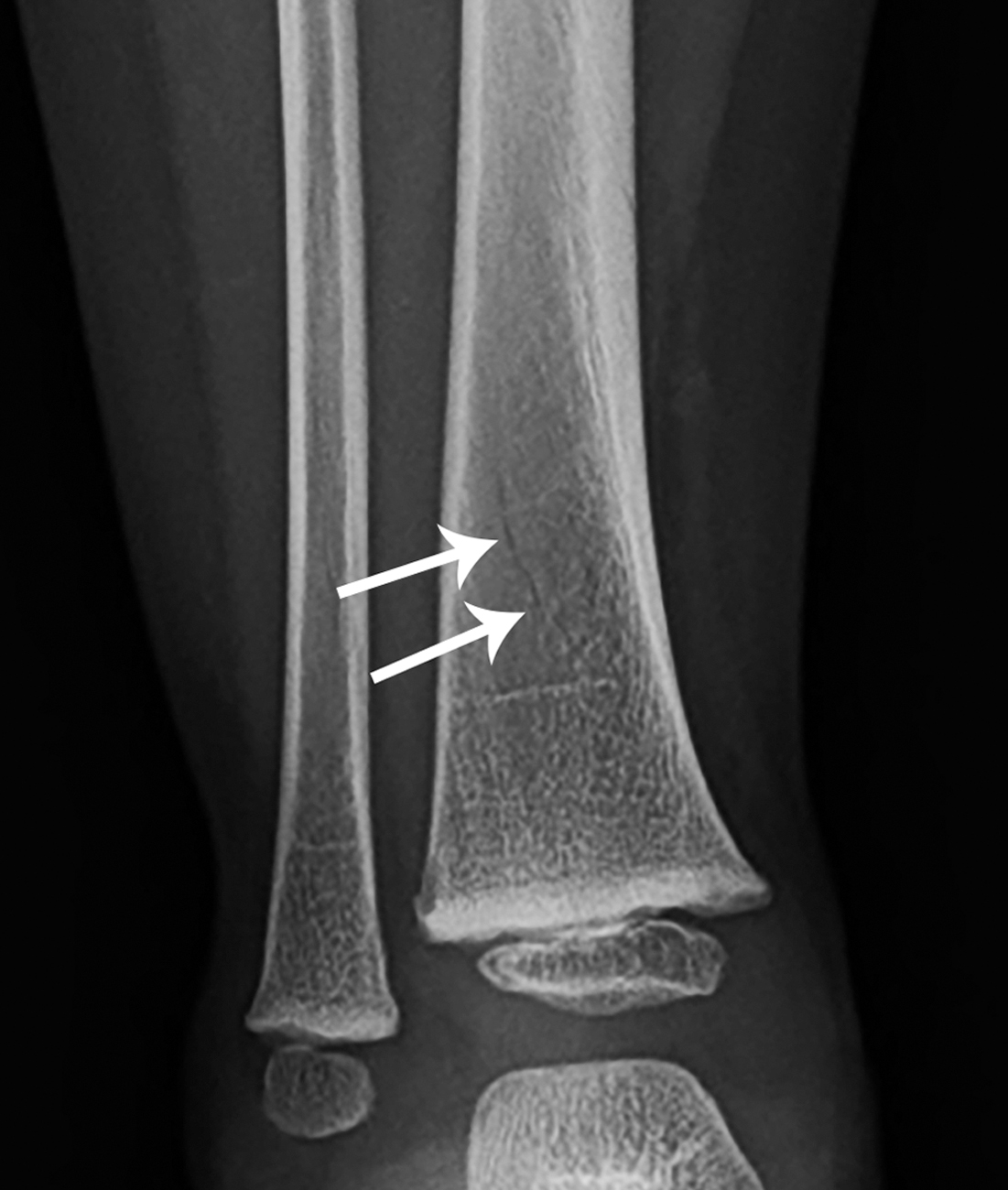
Two views (AP and lateral) of the involved extremity show a nondisplaced right distal tibia fracture ( Fig. 76.1 ). This fracture is not well visualized on the lateral view, but no signs of angulation or displacement are seen ( Fig. 76.2 ). The visualized portions of the knee and ankle do not show any apparent facture or signs of injury.

Case conclusion
This child was noted to have a toddler’s fracture of the tibia and was placed in a posterior short leg splint, with referral to Pediatric Orthopedics. Repeat imaging approximately 1 month after the injury demonstrated healing of the fracture with no apparent complication ( Figs. 76.3 and 76.4 ).











