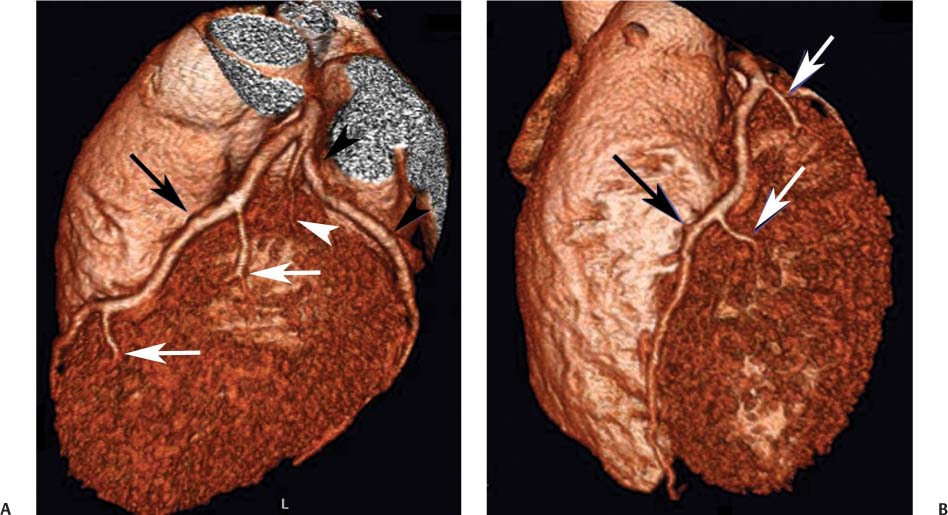
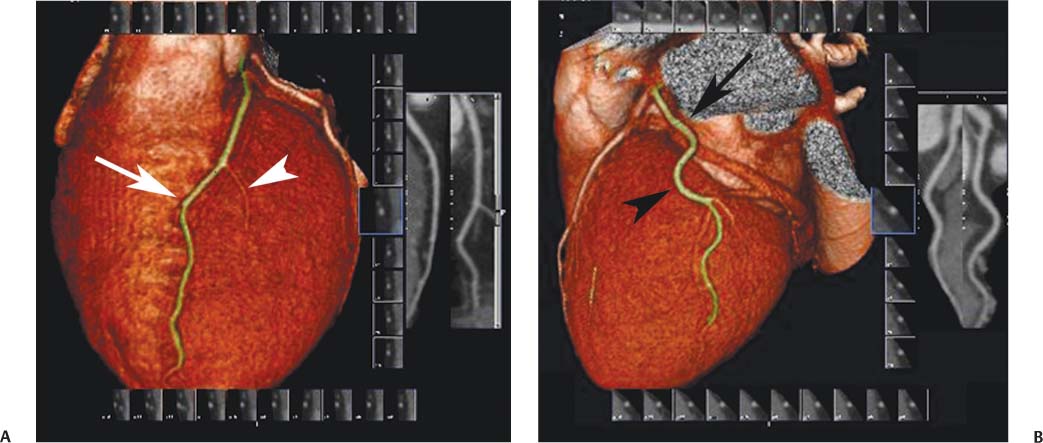
1 Coronary heart disease is the single largest cause of mortality in the United States and is an underlying or contributing cause in one of every five deaths.1 It is estimated that 785,000 Americans will have a new coronary attack in 2009, and 470,000 will have a recurrent attack. Furthermore, 195,000 silent first myocardial infarctions occur each year. One American will suffer a coronary event every 25 seconds, and one American will die of coronary heart disease every minute. The death rate from coronary heart disease has declined over the past four decades because of secondary preventive therapies used after myocardial infarction, new and improved treatments for angina and heart failure, and reductions in specific risk factors (cholesterol, blood pressure, smoking).2 However, the favorable improvements in risk factors among Americans have been partially offset by increases in body mass index and diabetes, such that the burden of disease remains high. The prevalence of coronary heart disease is about 6.0% in black Americans and 6.1% among white Americans.3 Evaluation of chest pain and related symptoms is the most common reason for an emergency department visit by an adult man and the second most common reason for a visit to the emergency department by an adult woman in the United States.4 Chest pain accounts for more than six million emergency department visits and almost two million inpatient hospital admissions annually. Acute coronary syndrome (ACS) refers to the patient who presents with an acute myocardial infarction or unstable angina. The number of patients admitted annually to U.S. hospitals with the diagnosis of ACS is close to a million. More than 2% of patients who present to an emergency department with ACS are discharged inappropriately; these missed diagnoses are associated with increased mortality.5,6 Preventive therapy for coronary disease depends on prospective identification of the patient who is truly at risk for ACS before the appearance of symptoms. Effective treatment of ACS depends on a rapid and accurate diagnosis of this entity in the symptomatic patient. The imprecise predictive value of risk factors, clinical symptoms, and biochemical markers is a major limitation in the treatment of coronary heart disease. Cardiac CT has the potential to improve the accuracy of risk stratification for preventive therapy7–9 and efficiently excludes the diagnosis of ACS in the patient with chest pain.10–13 Imaging of the heart and coronary arteries is complicated by the rapid, nonlinear motion of cardiac structures. Coronary CT angiography (CTA) became practical with the introduction of electrocardiographic gating and multislice technology. Among the various modalities capable of cardiac imaging, CT excels in its ability to depict coronary calcification, coronary anatomy, and cardiac-chamber morphology. The information obtained from cardiac CT is often complementary to that provided by other studies, including echocardiography, nuclear scintigraphy, cardiac magnetic resonance (MR) imaging, and conventional catheter angiography. Numerous studies have demonstrated the accuracy and high negative predictive value of CT for evaluation of coronary artery stenosis.14 Given the lower costs associated with CT compared with conventional angiography, CT provides a cost-effective alternative to diagnostic catheterization for the evaluation of coronary artery disease (CAD) in most patients.15 Clinical trials continue to establish the utility and cost-effectiveness of cardiac CT coronary angiography for specific clinical indications.16 Recent improvements in CT technology with faster scans, better temporal resolution, lower radiation exposure, and dual-energy imaging continue to expand the applications of CT to cardiac imaging. Additional clinical trials are needed to demonstrate the utility of CT for newer applications that include stress imaging and evaluation of myocar-dial perfusion.17 Two major categories of advanced CT technology have been applied to cardiac imaging: electron-beam CT (EBCT) and multislice–multidetector computed tomography (MDCT). EBCT is best known for its application to measure coronary artery calcification (Fig. 1.1). Calcium scoring provides cardiac risk stratification with a low radiation dose of about 1 mSv. More than one thousand publications have documented the utility of EBCT for coronary calcium scoring. EBCT is distinguished by the absence of moving parts within the scanner and by a short acquisition time, which reduces motion artifact. The ultrafast scan time of EBCT (33–50 msec) is possible because a rotating electron beam is used to produce thin-section tomographic scans without gantry rotation. However, EBCT is limited in terms of slice thickness (not <1.5 mm) and overall image noise. Fig. 1.1 Coronary calcium and calcium scoring. Axial image through the level of the left anterior descending artery demonstrates the presence of calcification in the proximal portion of this vessel (arrows). A detailed discussion of calcium scoring is covered in Chapter 5. Fig. 1.2 Surface-rendered volumetric images of the left coronary circulation provide a three-dimensional prospective and demonstrate positions of the coronary arteries relative to the underlying cardiac structures. (A) Left anterior oblique (LAO) projection demonstrates left anterior descending artery (black arrow), as well as two diagonal branches (white arrows). A normal variant, the ramus medianus, extends from a trifurcation of the left main coronary artery (white arrowhead). The third branch from the left main coronary artery is the circumflex (black arrowheads), which travels in the left atrioventricular groove. No obtuse marginal branches are identified from the circumflex artery. The territory of left ventricular free wall is supplied entirely by the diagonal branches and the ramus. (B) Shallow LAO from a more caudal vantage point demonstrates the left anterior descending (LAD) coronary artery as it courses down the anterior interventricular groove (black arrow). The two diagonal branches are again identified (white arrows). (C) Anteroposterior view again demonstrates the LAD (arrow). Two septal perforator branches extend from the LAD into the inter-ventricular septum (arrowheads). The septal perforators are identified only in their proximal portions before entering the interventricular septum. MDCT has assumed the dominant role for contrast-enhanced CTA of the coronary arteries (Fig. 1.2). The spatial resolution and signal-to-noise characteristics of MDCT are superior to those of EBCT. Overall image quality for coronary CTA is better with MDCT compared with EBCT, especially with heavier patients. MDCT technology is available from competing manufacturers, who are continuously improving their systems to provide the best spatial and temporal resolution and the best techniques to reduce artifact from calcium and metallic stents. “Conventional” 64-slice MDCT technology remains the “workhorse” of cardiac CT imaging, with a temporal resolution in the range of 165 to 210 msec. Several MDCT scanners are now available with 256 or 320 slices to provide greater anatomic coverage. Newer scanners use faster gantry rotation times and dual radiographic sources to achieve a temporal resolution as low as 75 msec with subsecond scan times for the entire heart.18 Advances in dual-energy and multienergy imaging techniques are poised to provide further improvements in plaque characterization and evaluation of myocardial enhancement. These techniques should provide additional prognostic information through assessment of plaque composition and stability19 and myocardial perfusion studies.20 With respect to the detection of stenosis in native coronary arteries, numerous studies have compared the diagnostic accuracy of coronary CTA with that of invasive catheter angiography, the traditional gold standard. In most of these studies, significant coronary stenosis is defined as diameter reduction of 50% or more. A recent meta-analysis of 64 slice studies demonstrated a sensitivity of 99% (95% confidence interval [CI], 97–99%) and a specificity of 89% (95% CI, 83–94%) for the presence of significant coronary stenosis in a patient-based analysis.14 In a by-segment analysis, CTA demonstrated a sensitivity of 90% (95% CI, 85–94%) and a specificity of 97% (95% CI, 95–98%). The median negative predictive value of CTA for patient-based detection of coronary disease was 100%. Although the abundant publications from single-center trials demonstrate very high sensitivity and negative predictive value for significant coronary stenosis, these results have only recently been tested in multicenter trials. Accuracy is often lower in multicenter trials when technology is used in a standardized fashion on a more diverse patient population by multiple investigators. The results of multicenter trials by Budoff and colleagues,21 Meijboom and coworkers,22 and Miller and colleagues23 are summarized in Table 1.1, along with meta-analysis results from Mowatt et al,14 Meijer and associates,24 and Vanhoenacker et al.25 All these studies support the high negative predictive value of a normal coronary CTA to exclude the presence of significant coronary stenosis. Cardiac CT may be performed for a wide range of clinical applications. Technical details related to multislice scanners, scan protocols, and radiation dose are discussed in Chapter 2. The remaining chapters in this text are organized to discuss individual applications of cardiac CT. Gated CT of the heart without administration of contrast material has proven useful to image coronary calcium as a measure of overall atherosclerotic plaque burden (Chapter 5). Although this technique does not demonstrate the presence or absence of stenosis in a particular patient, it is useful for risk assessment.26 Clinical trials suggest that coronary calcium scoring can modify the predicted risk based on the Framingham risk score.27 A consensus has emerged that coronary calcium scoring is most appropriate for asymptomatic individuals with an intermediate Framingham risk in whom the calcium score may be used to determine the appropriate levels of lifestyle modification and pharmacologic therapy.28
Key Issues in Cardiac CT
 Coronary Heart Disease
Coronary Heart Disease
 Cardiac Computed Tomography Technology
Cardiac Computed Tomography Technology
 Accuracy of Coronary Computed Tomography Angiography
Accuracy of Coronary Computed Tomography Angiography
 Clinical Applications of Cardiac Computed Tomography
Clinical Applications of Cardiac Computed Tomography
Author | Sensitivity (by Patient) | Specificity (by Patient) |
|---|---|---|
Budoff et al21 | 0.95 | 0.83 |
Miejboom et al22 | 0.99 | 0.64 |
Miller et al23 | 0.85 | 0.90 |
Mowatt et al14 | 0.99 | 0.89 |
Meijer et al (40- & 64-slice)24 | 0.98 | 0.91 |
Vanhoenacker et al25 | 0.99 | 0.93 |
CTA has numerous cardiac applications. It provides a noninvasive assessment of coronary anatomy (Chapter 3) and a clear demonstration of coronary anatomic variations and anomalies (Chapter 4). Because CT demonstrates adjacent anatomic structures as well as coronary arteries, MDCT provides a unique opportunity to assess the origin and course of a coronary artery relative to the aortic root, pulmonary artery, and myocardium (Fig. 1.3). Coronary venous anatomy is also visualized (Fig. 1.4). With respect to assessment of coronary anatomic variations, CTA is often superior to conventional catheter arteriography.29
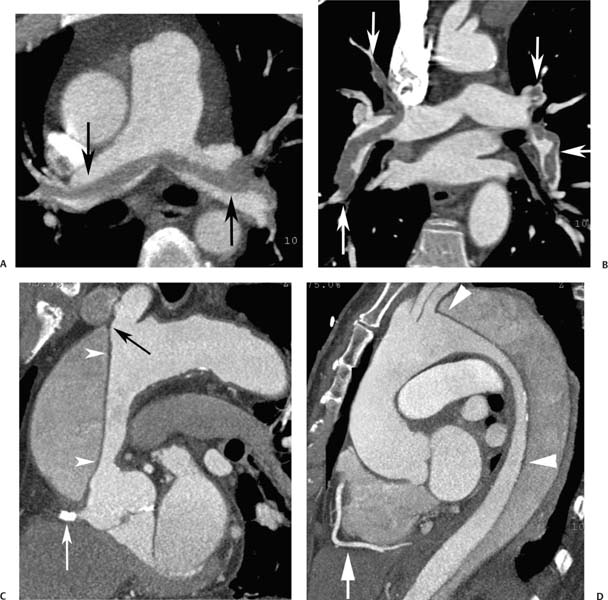
Coronary CT demonstrates high sensitivity for the detection of coronary artery stenosis (Chapter 6). Although diagnostic accuracy may be limited in patients with heavy coronary calcification, there is a general consensus that “a normal CT coronary angiogram allows the clinician to rule out the presence of hemodynamically relevant coronary artery stenoses with a high degree of reliability.”7 In patients who do not have a high pretest likelihood of coronary stenosis, a normal CT coronary angiogram serves to obviate any further need for a diagnostic coronary workup.30 Because the radiation dose with state-ofthe-art coronary CTA is lower than that of nuclear scintigraphy and the negative predictive value of CT is superior to that of nuclear scintigraphy, CTA provides a reasonable alternative to nuclear scintigraphy for the evaluation of chest pain in a patient with a low to intermediate risk for CAD. In the setting of an emergency department patient presenting with chest pain, CT can be used for a “triple rule-out” to evaluate the pulmonary arteries for pulmonary embolism, the thoracic aorta for dissection, and the coronary arteries for significant stenosis (Fig. 1.5). With a single examination requiring no more than 100 mL of intravenous contrast, CTA can evaluate all three of these serious vascular causes of chest pain as well as nonvascular extracardiac causes of pain (Chapter 15).31
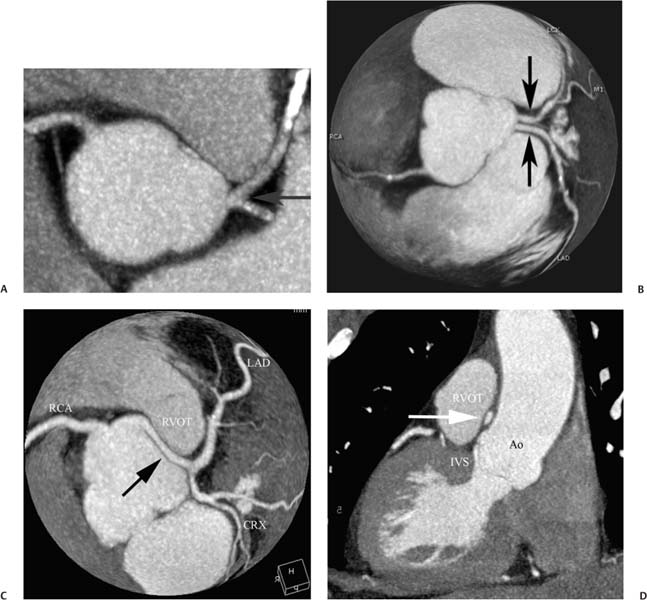
Fig. 1.3 Anatomic variations in the left main coronary artery. (A) Slab maximum intensity projection (MIP) demonstrates a cloacal left main coronary artery, which branches immediately into the left anterior descending (LAD) coronary artery and circumflex arteries (arrow). (B) Globe MIP in a second patient demonstrates independent origins of the LAD and circumflex arteries (black arrows). A left main coronary artery is not present. The globe MIP demonstrates three-dimensional relationships of the coronary vessels to the underlying cardiac anatomy. (C) Globe MIP in a third patient demonstrates an anomalous left coronary artery (arrow) passing between the aorta and right ventricular outflow tract (RVOT). (D) Sagittal reconstruction demonstrates the anomalous vessel (arrow) passing between the aorta (Ao) and RVOT above the level of the interventricular septum (IVS).
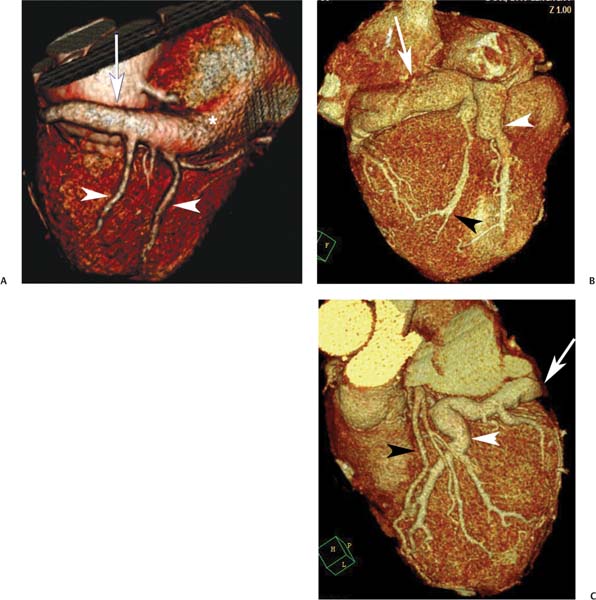
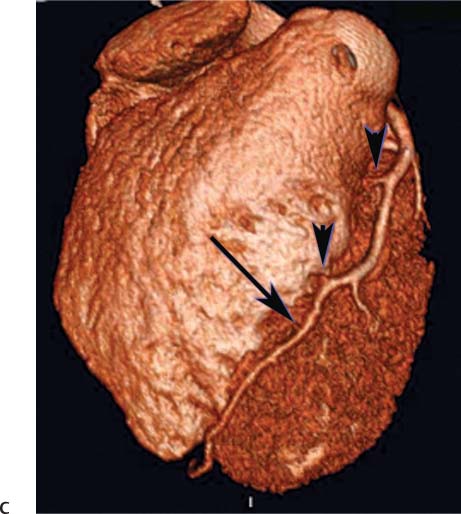
Fig. 1.4 Coronary veins from two different patients. (A) Surface image of the posterior aspect of the left ventricle demonstrates the coronary sinus (arrow) as it extends around the left atrioventricular (AV) groove into the right atrium (*). Several coronary veins (arrowheads indicate the posterior vein of the left ventricle and the left marginal vein) are identified as they course into the coronary sinus. (B) Surface image of the crux of the heart demonstrates dilated coronary veins related to obstruction of the coronary sinus (arrow). A dilated middle coronary vein is identified in the posterior interventricular groove (white arrowhead). A collateral vein is present along the surface of the left ventricle (black arrowhead). (C) Surface image of the anterior aspect of the heart in the same patient as in part B. The dilated great cardiac vein (arrow) represents the continuation of the coronary sinus in the left AV groove. The dilated anterior interventricular vein (white arrowhead) courses down the anterior interventricular groove alongside the left anterior descending artery (black arrowhead).
In patients with known coronary disease who have been treated with angioplasty and a stent, the question of instent stenosis or stent thrombosis often arises. Current 64-slice CT technology is limited in this evaluation because of blooming artifact associated with calcium and metallic stents.32 Nonetheless, larger stents are often well evaluated, and conventional angiography may be avoided in these patients after demonstration of a normal stent lumen (Chapter 7). Recent studies suggest that the sensitivity and specificity of CT for in-stent stenosis are greater than 90% in adequately visualized stented vessels.33 Given the current pace of technological advances in CT, it is likely that future improvements will expand further the utility of cardiac CT for imaging of stents.
Fig. 1.5 “Triple rule-out” scans in four different patients with evidence of acute pulmonary embolism or aortic dissection. (A) Coronal maximum intensity projection (MIP) demonstrates a saddle pulmonary embolism extending across from the right to the left pulmonary artery (arrows). (B) Coronal MIP demonstrates pulmonary embolism extending into upper and lower lobar branches (arrows). (C) Oblique MIP demonstrates the ascending aorta and aortic arch with a stent in the proximal right coronary artery (RCA; white arrow). A type “A” dissection of the ascending aorta is present with an intimal flap (arrowheads) beginning from just above the RCA origin and extending to the origin of the innominate artery (black arrow). (D) Oblique MIP of the thoracic aorta in a different patient demonstrates a type “B” dissection extending from just beyond the origin of the left subclavian artery down through the thoracic aorta (arrowheads). The RCA is identified as it courses around the right atrioventricular groove (arrow).
CTA is useful in both the pre-operative planning of coronary bypass surgery and in the post-operative evaluation of bypass grafts (Chapter 8),34 especially in the setting of repeat cardiac surgery after previous bypass.35 CTA clearly demonstrates the location of bypass grafts relative to other cardiac and thoracic anatomic landmarks. Venous bypass grafts are easily evaluated for stenosis or thrombosis. Arterial bypass grafts are more difficult to evaluate because of their smaller size. Native vessels are difficult to evaluate in these patients because of extensive calcification. Future improvements in CT technology are likely to expand this application as well.
Assessment of cardiac morphology and function is usually performed with echocardiography or cardiac MR. The lack of ionizing radiation with these techniques presents a major advantage over CT when detailed imaging of the coronary arteries is not needed. When evaluation of coronary anatomy is required, cardiac CT can provide assessment of coronary anatomy, cardiac morphology, and function (Chapter 9)36 and cardiac valves (Chapter 10)37 in a single evaluation (Fig. 1.6). A recent review of patients imaged with coronary CTA for suspected CAD identified unsuspected cardiovascular morphologic abnormalities in almost 1% of patients, including aortic aneurysms, hypertrophic cardiomyopathy, valvular heart disease, ventricular septal defects, left ventricular noncompaction, left atrial myxoma, and left ventricular apical aneurysms.38 Assessment of morphology and function is quite useful in preoperative and postoperative studies for valve surgery and ventricular remodeling as well as in planning for left atrial ablation (Chapter 11) and other percutaneous interventional procedures (Chapter 12). Imaging of the coronary circulation can be combined with imaging of the thoracic aorta for pre-operative assessment and post-surgical evaluation of aortic aneurysms and dissections (Chapter 13). Finally, CT imaging of the heart and great vessels may be useful for evaluation of congenital heart disease in the adult (Chapter 14).
Four new category I Current Procedural Terminology (CPT) codes have been introduced for 2010 to replace the former category III codes, which were viewed as “investigational” by many insurance carriers. Calcium scoring is covered by the code for cardiac CT without contrast material (75571). Evaluation of cardiac anatomy and chambers as well as coronary and pulmonary veins is covered by the code for contrast-enhanced cardiac CT (75572). A separate code is used for evaluation of cardiac anatomy in the setting of congenital heart disease (75573). Evaluation of coronary arteries, including evaluation of bypass grafts and stents, is included along with evaluation of cardiac morphology in the code for CTA of the heart (75574). There is no longer an add-on code for cardiac function; evaluation of cardiac function is subsumed into codes 75572–75574.
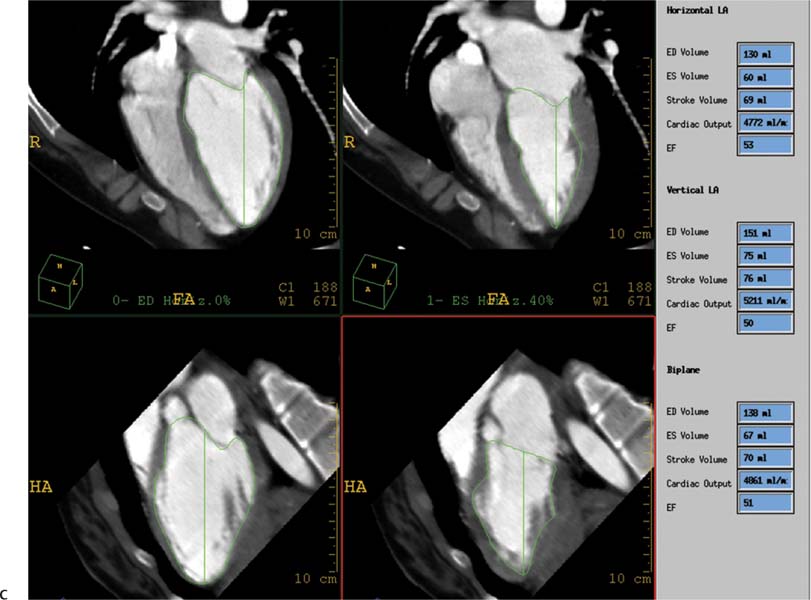
Fig. 1.6 Surface-rendered image of the left coronary circulation demonstrating tools for the assessment of coronary stenosis and evaluation of left ventricular (LV) function. In this patient, the circumflex artery supplies the majority of the LV free wall. (A) The left anterior oblique surface projection demonstrates the left anterior descending artery (LAD) as it courses into the anterior interventricular groove (arrow). A single small diagonal branch is identified (arrowhead). Assessment of the vessel lumen is facilitated with orthogonal curved maximum intensity projection (MIP) images of the LAD along the right side of the image and by short-axis images through multiple levels presented as small squares surrounding the surface projection. The LAD appears normal with no stenosis. (B) Left lateral projection demonstrates the circumflex artery as it courses in the left atrioventricular groove (arrow). The circumflex artery terminates in a large obtuse marginal branch (arrowhead), which supplies much of the left ventricular wall. Diagonal branches are not well developed in this patient. Orthogonal curved MIP images along the right side of the image and short-axis images of the circumflex demonstrate a normal vessel. Surface-rendered image of the left coronary circulation demonstrating tools for the assessment of coronary stenosis and evaluation of left ventricular (LV) function. In this patient, the circumflex artery supplies the majority of the LV free wall. (C) Calculation of the ejection fraction is performed with a biplane Simpson algorithm using systolic and diastolic images in orthogonal four-chamber and two-chamber views. A low normal ejection fraction of just over 50% is computed.
 Appropriate Utilization of Cardiac Computed Tomography
Appropriate Utilization of Cardiac Computed Tomography
Based on the recent statement of the American Heart Association (AHA), calcium scoring is most appropriate for risk stratification of patients with intermediate risk as suggested by traditional risk factor assessment.28 Although the AHA criteria for calcium scoring are based on an intermediate Framingham risk score, a logical extension of this position suggests that calcium scoring is appropriate in any asymptomatic population with an intermediate risk of coronary heart disease based either on a Framingham risk calculation or on other risk factors not considered in the Framingham analysis (such as an elevated C-reactive protein, metabolic syndrome, obesity, or a family history of premature coronary disease).39 An elevated calcium score may alter the expected risk of a coronary event and demonstrate a need for more aggressive lifestyle modifications or medical therapy.
A review of appropriateness criteria for cardiac CT conducted under the auspices of the American College of Cardiology Foundation concluded that cardiac CTA is most appropriate for evaluation of “cardiac structure and function and for diagnosis in symptomatic, intermediate CAD risk patients.”40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree