Fig. 55.1
Anteroposterior radiograph of the knee demonstrating a radiolucent (osteonecrosis) lesion (orange circle) of the medial femoral condyle with collapse of the weight bearing portion
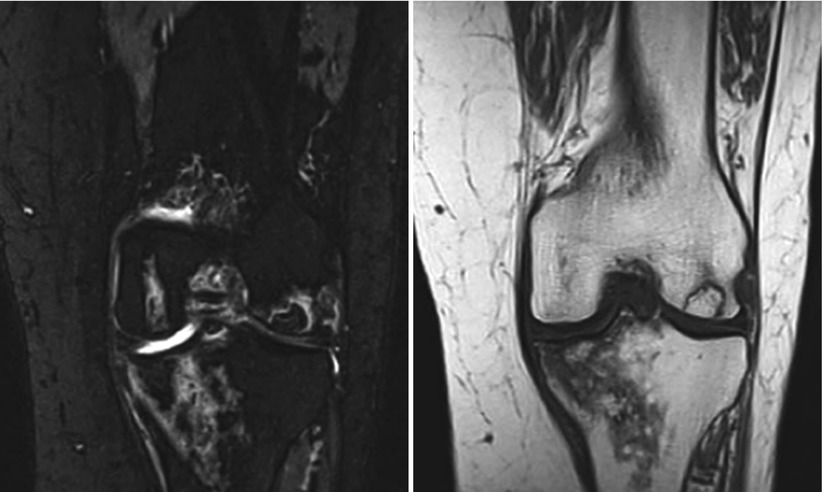
Figs. 55.2 and 55.3
Coronal MRI images suggestive of osteonecrotic regions in the distal femur and the proximal tibia
The initial finding that can first be identified on MRI is bone marrow edema that is not visible on CT or radiographs. MRI’s main limitation is that it may not detect an ON lesion for 4–6 weeks after symptom onset. This time frame is called the “window period” [3]. The other limitation of MRI is if it demonstrates bone marrow edema, it may be attributable to other causes including osteochondritis dissecans, bone bruise, or reactive processes [10].
End-stage ON shares many of the radiographic findings of severe osteoarthritis, and cases of ON may be misclassified as osteoarthritis. Fortunately, at that stage treatment is the same for both disease processes [12].
Aratake et al. looked at the use of fluoride PET imaging to evaluate SPONK. They found that fluoride PET scans could detect SPONK and measure lesions with comparative accuracy to radiographs and MRI. Further research will be needed to determine if it or other imaging techniques will provide additional prognostic or diagnostic information [18].
55.8 Diagnosis
The diagnosis of SPONK is heavily based on the history with sudden onset of pain with no identifiable etiology for ON. Secondary ON will have an identifiable cause in the patient’s history. Imaging helps confirm the diagnosis, but in the early stages, the findings on imaging are not specific. Osteochondritis dissecans is on the differential, but it is more often found in patients younger than 25 years old and located to a single condyle without affecting other parts of the joint. Also, imaging would demonstrate the separation of articular cartilage with subchondral bone [1]. Other causes of knee pain could include meniscus and ligament injuries that would present with other clinical and imaging findings [10]. Osteoarthritis can have similar symptoms, but it usually has a more chronic and progressive onset of pain.
There are studies being conducted to find additional markers for SPONK such as serum or synovial fluid markers. Synovial levels of chondroitin 6-sulfate have been found to be significantly greater in cases of SPONK than medial compartment osteoarthritis. Studies evaluating serum markers such as bone-specific ALP, osteocalcin, procollagen type I N-terminal propeptide, and C-terminal cross-linking telopeptide did not have any difference between osteoarthritis and SPONK [24]. Further research may be able to identify other markers either in synovial fluid or serum that can help distinguish osteoarthritis from ON. Although with the current treatment options, the clinical utility of distinguishing the two remains to be seen.
55.9 Treatment and Clinical Results
55.9.1 General Principles
Treatment of osteonecrosis of the knee depends on the extent of disease. Early lesions may be treated with nonoperative or joint-preserving techniques. Advanced osteonecrosis may require a joint replacement [25]. Historically, the treatment options for osteonecrosis of the knee include conservative management, arthrotomy with curettage, high tibial osteotomy, and arthroplasty [20]. Conservative options include weight loss, analgesics, isometric quadriceps exercises [20], and protected weight-bearing with assistive devices [26]. Traditionally, these options have been reserved for patients with small osteonecrotic lesions with mild symptoms. Muheim and Bohne recommended conservative treatment for patients with small osteonecrotic lesions less than 3.5 cm2 in area and tibia1 osteotomy with arthrotomy for those with large osteonecrotic lesions exceeding 5 cm [19, 21]. Initial treatment for patients diagnosed with osteonecrosis involves conservative management for at least 3 months duration [26]. Arthrotomy with curettage is performed in cases with large lesions [20]. These patients have minimal osteoarthritic changes and no significant knee deformity. In cases of significant varus deformity of the knee, high tibial osteotomy may be performed [20]. The ideal correction is to obtain a femorotibial angle of 170° (10° valgus) [20]. Arthroplasty is reserved for large lesions with degenerative changes and possible malalignment of the knee [20].
Modern techniques are also focused on joint-preserving therapies prior to arthroplasty [26]. Patients that remain symptomatic after at least 3 months of conservative management may undergo diagnostic arthroscopy of the affected knee. If diffuse chondral lesions and subchondral collapse are noted, chondroplasty and debridement of loose tissue can be performed 26. If intra-articular pathology such as meniscal lesions is found, appropriate debridement and meniscectomy are performed [26]. After diagnostic or therapeutic arthroscopy, percutaneous core decompression of the osteonecrotic lesion may be performed using a small-diameter drill bit through an extra-articular approach [26]. Focal chondral defects can be treated with osteochondral autologous transfer from less weight-bearing regions of the articular cartilage of the knee [26]. Patients who remain symptomatic despite repeat core decompressions, or who progress to condylar collapse despite joint-preserving surgical treatment, are indicated to undergo total or unicompartmental knee arthroplasty (UKA) [26]. A recent systematic review of the literature between 1999 and 2012 showed that among joint-preserving procedures, core decompression prevented additional surgical treatment in pre-collapse knees with a failure rate of 10.4 %. Autogenous and osteochondral grafts decreased the need for additional surgery in both pre-collapse 0 % and post-collapse knees 10.5 % [27].
55.9.2 Bisphosphonates
Bisphosphonates, such as alendronate, have been used successfully to treat osteonecrosis of the femoral head, as they may prevent bone resorption during the reparative phases of osteonecrosis [25]. Another bisphosphonate, neridronate, is used primarily for the treatment of Paget disease and osteoporosis [25]. Corrado et al. [28] explored the use of this medication as a nonoperative treatment for osteonecrosis of the knee. Their patient had reduced pain and swelling after 2 months of this medication combined with analgesics. Their treatment protocol included 100 mg/day of aspirin, 0.5 μg of calcitriol, and 25 mg/month of intramuscular neridronate. An MRI scan obtained 2 months after initiation of treatment showed decreased bone marrow edema and reduction in the size of the necrotic lesions.
55.9.3 Antitumor Necrosis Factor Alpha (Anti-TNF-Alpha) Agents
Tumor necrosis factor alpha (TNF-alpha) has been identified as the compound that regulates production of interleukin-1 in rheumatoid arthritis which can be treated with anti-TNF-alpha medications such as adalimumab [29, 30]. A case report demonstrates that a 54-year-old man with monoarticular rheumatoid arthritis and osteonecrosis of the left knee, who failed corticosteroids and systemic treatment, was given a 40-mg intra-articular injection of adalimumab, and 1 week later, pain and stiffness resolved and range of motion improved. The patient was given a second injection 15 days later, and an MRI taken 1 month thereafter showed healing of the osteonecrotic lesion [31].
Although the role of anti-TNF-alpha medications in osteonecrosis is not understood, they may affect the cytokines responsible for the osteoclast progenitor cell regulation [29]. In this case, it is difficult to determine whether the change in MRI findings represents resolution of an osteonecrotic lesion or only bony edema associated with degenerative changes [25].
55.9.4 Core Decompression
Jacobs et al. were the first to describe the treatment of osteonecrosis of the knee using core decompression [32]. However, prior to the knee, core decompression was used successfully in the treatment of osteonecrosis of the hip [33]. Marulanda et al. used core decompression and modified the procedure with the percutaneous drilling of 3-mm holes in each of 61 knees (38 patients; average follow-up, 3 years; range, 2–4 years) [34]. They reported a 92 % (56 knees) successful clinical outcome, which they defined as a postoperative Knee Society score of 80 or more points. Two knees with poor outcomes were treated with total knee arthroplasty (TKA) and had postoperative Knee Society scores of 90 and 91 points. Of the remaining three knees with poor outcomes, two were treated with bilateral arthroscopic debridement and one with a bone grafting procedure. At the latest follow-up, however, these three knees were still categorized as having poor outcomes (Knee Society scores <80 points). The authors reported low rates of complications and morbidity with core decompression [34].
55.9.5 Biologic Substitutes
A new technique combines artificial bone grafting and core decompression for selected patients with SPONK [35]. In this study, there were strict primary and secondary indications for identifying which patients were to receive this procedure. Primary indications included a diagnosis of SPONK in the medial femoral condyle and a femorotibial angle between 173° and 179°. A secondary indication was a patient’s inability to undergo TKA or high tibial osteotomy because of other diseases. The authors treated 12 patients with this combination approach, which involved decompression and grafting, using a calcium hydroxyapatite ceramic device with an interconnected porous structure (IP-CHA; NEOBONE®, Toshiba Ceramics Company, Tokyo, Japan). The lesions were curetted, and grafting was accomplished with the artificial bone plugs in a mosaicplasty fashion. After an average 2-year follow-up, 12 patients had a statistically significant improvement in the Japanese Orthopedic Association score assessing pain on walking, pain on ascending or descending, range of motion, and joint effusion. MRI scans showed smooth surfaces between the bone graft and the femur in nine (75 %) of 12 patients. There was, however, no histologic evaluation for the presence of osteonecrosis [35]. Larger study groups and long-term follow-up are required before the combination of core decompression (a proven technique) with artificial bone grafting can be considered an option of choice
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








