8
Large Bowel
Diverticular Diseases
Overview
 Diverticula are outpouchings of the mucosa through the colonic wall. Usually located at the area of colonic wall that is traversed by arterioles (vasa recta)
Diverticula are outpouchings of the mucosa through the colonic wall. Usually located at the area of colonic wall that is traversed by arterioles (vasa recta)
 False diverticulum includes only mucosa and submucosa
False diverticulum includes only mucosa and submucosa
 May lead to perforation or bleeding
May lead to perforation or bleeding
Signs and Symptoms
 Abdominal pain, fever, leukocytosis, lower GI bleeding
Abdominal pain, fever, leukocytosis, lower GI bleeding
Diagnosis
 Hinchey classification of perforated diverticular disease:
Hinchey classification of perforated diverticular disease:
• Class I: Perforation with localized paracolonic abscess
• Class II: Perforation with pelvic abscess
• Class III: Perforation with purulent peritonitis
• Class IV: Perforation with feculent peritonitis
 Diverticulitis: CT scan with IV contrast. Water-soluble rectal contrast is relatively contraindicated in the setting of acute diverticulitis
Diverticulitis: CT scan with IV contrast. Water-soluble rectal contrast is relatively contraindicated in the setting of acute diverticulitis
 Lower GI bleed from diverticula: Colonoscopy, visceral angiography, tagged red blood cell scan
Lower GI bleed from diverticula: Colonoscopy, visceral angiography, tagged red blood cell scan
Treatment/Management
 Diverticulitis with no diffuse peritonitis: Conservative treatment with bowel rest, antibiotics
Diverticulitis with no diffuse peritonitis: Conservative treatment with bowel rest, antibiotics
 Recurrent diverticulitis: Cut off for timing of surgery still a controversial debate, but most patients are offered resection if they have had more than three episodes of diverticulitis;failure to resolve an episode despite medical management; complicated diverticulitis (for example: perforation with abscess formation, colovesicular fistula, etc); or if the attacks are increasing in severity or frequency
Recurrent diverticulitis: Cut off for timing of surgery still a controversial debate, but most patients are offered resection if they have had more than three episodes of diverticulitis;failure to resolve an episode despite medical management; complicated diverticulitis (for example: perforation with abscess formation, colovesicular fistula, etc); or if the attacks are increasing in severity or frequency
 Abscess: IR drainage
Abscess: IR drainage
 Bleeding: Resuscitation, therapeutic colonoscopy, IR embolization, surgical resection for persistent, or the rare case of uncontrollable bleeding
Bleeding: Resuscitation, therapeutic colonoscopy, IR embolization, surgical resection for persistent, or the rare case of uncontrollable bleeding
RADIOLOGY
Diverticulosis
 CT findings (Fig. 8.1)
CT findings (Fig. 8.1)
• Focal outpouchings from the colonic wall without surrounding inflammation (which would indicate diverticulitis)
FIGURE 8.1 A–E
A. Psoas muscle
B. Vertebra
C. Small bowel loops
D. Liver
E. Stomach
F. Spleen
G. Descending aorta
H. Bladder
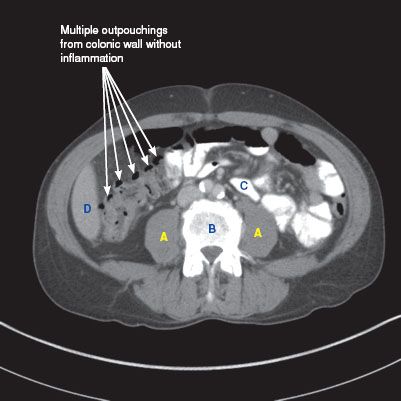
FIGURE 8.1 A
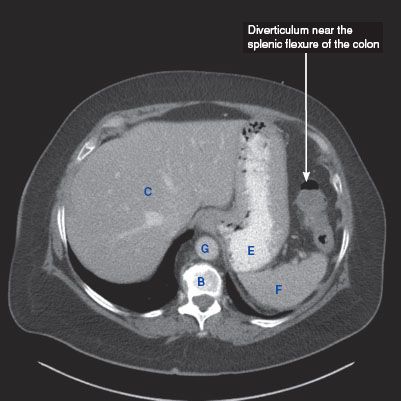
FIGURE 8.1 B
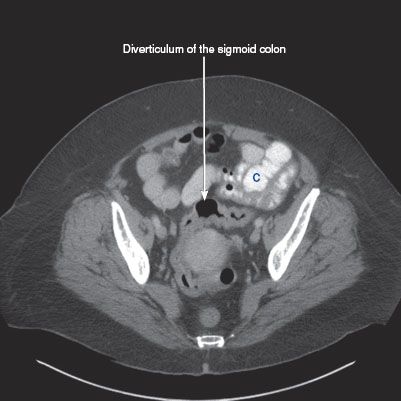
FIGURE 8.1 C
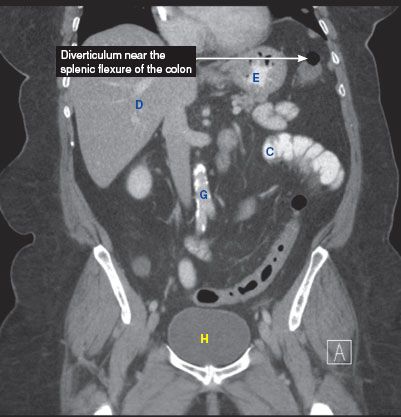
FIGURE 8.1 D
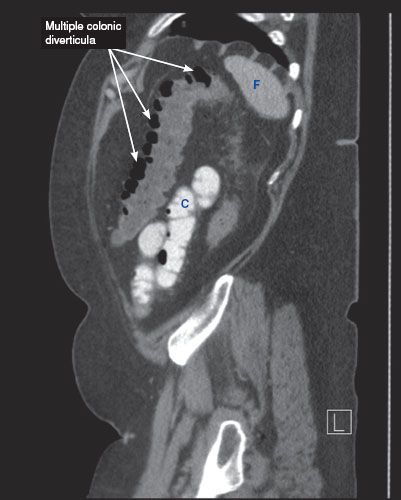
FIGURE 8.1 E
Diverticulitis
 Plain film findings
Plain film findings
• Usually normal, but may see thickened loops of colon
 US findings
US findings
• May reveal a pericolic abscess as a hypoechoic fluid collection with posterior acoustic enhancement near the bowel wall, surrounded by inflamed hyperechoic fat
 CT findings (Fig. 8.2)
CT findings (Fig. 8.2)
• Pericolonic fat stranding and edema
• May see a loculated, rim enhancing fluid collection, representing an abscess
• Colonic wall thickening secondary to inflammation
• Mild disease is characterized by minimal wall thickening and pericolonic inflammatory changes
• Moderate disease is characterized by the formation of pericolonic fluid collections, representing abscesses
• Severe disease is characterized by marked wall thickening, large amount of free air, large fluid collections, or marked phlegmonous changes
FIGURE 8.2 A,B
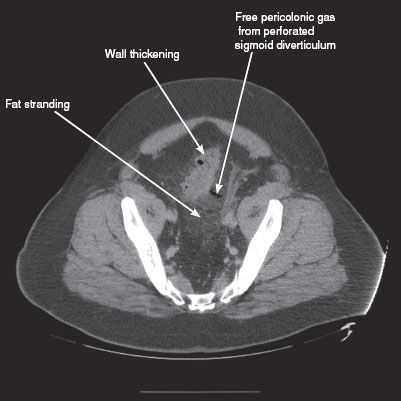
FIGURE 8.2 A
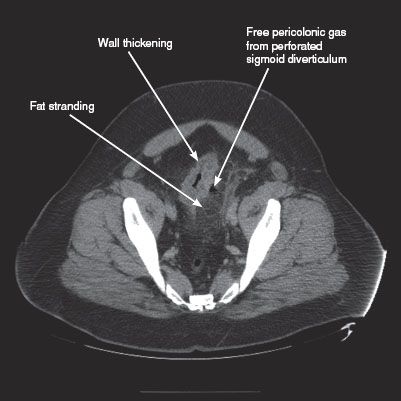
FIGURE 8.2 B
Perforated Diverticulitis
 CT findings (Fig. 8.3)
CT findings (Fig. 8.3)
• Free intraperitoneal air
• Pericolonic fat stranding surrounding the perforated diverticuli
FIGURE 8.3 A–D
A. Psoas muscle
B. Vertebra
C. Small bowel loops
D. Liver
E. Stomach
F. Bladder
G. Kidney
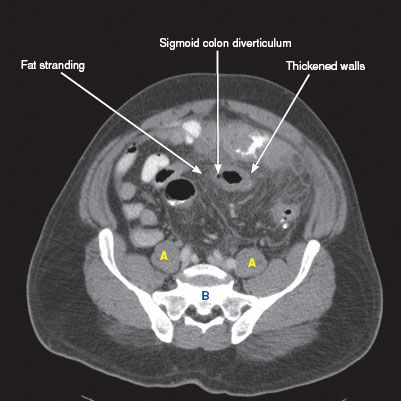
FIGURE 8.3 A
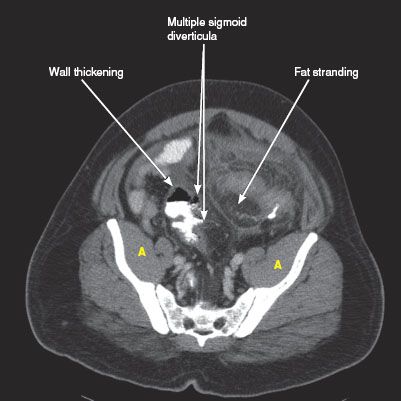
FIGURE 8.3 B
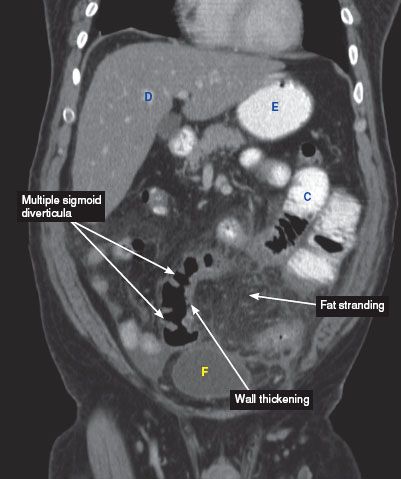
FIGURE 8.3 C
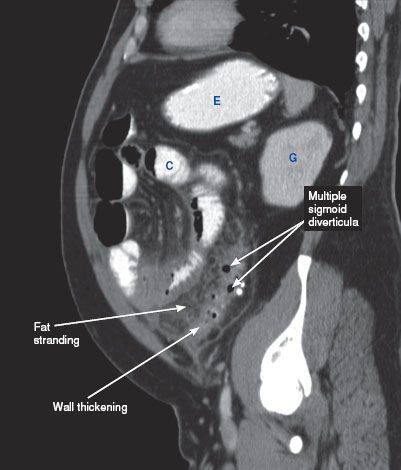
FIGURE 8.3 D
Diverticular Pelvic Abscess
 CT findings (Fig. 8.4)
CT findings (Fig. 8.4)
• Loculated, rim-enhancing fluid collection around the site of diverticulitis
• Extensive surrounding fat stranding
FIGURE 8.4 A–C
A. Sacrum
B. Ilium
C. Fat stranding
D. Liver
E. Small bowel loops
F. Bladder
G. Descending aorta
H. IVC
I. Portal vein
J. Vertebra
K. Uterus
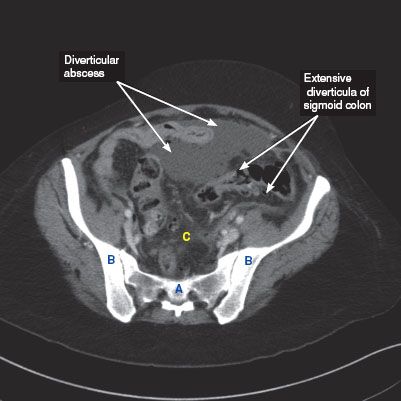
FIGURE 8.4 A
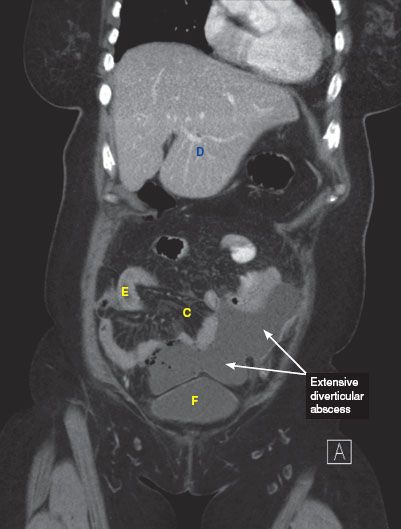
FIGURE 8.4 B
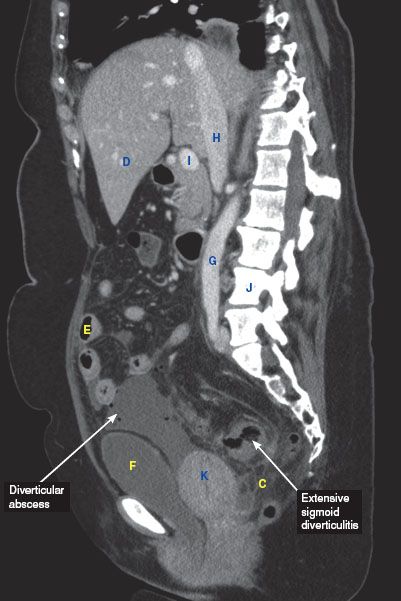
FIGURE 8.4 C
Colovesicular Fistula
RADIOLOGY
 CT findings (Fig. 8.5)
CT findings (Fig. 8.5)
• Gas within the bladder
• Focal wall thickening of the bladder
• Tethering of the colon to the bladder is usually seen. The fistula tract is usually not seen on CT
FIGURE 8.5 A–C
A. Rectum
B. Femoral head
C. Liver
D. Stomach
E. Small bowel loops
F. Urinary bladder
G. Superior mesenteric vein
H. Descending aorta
I. Vertebra
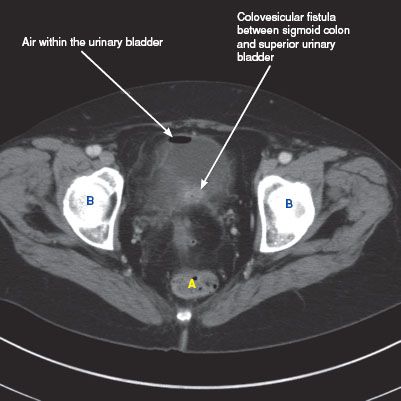
FIGURE 8.5 A
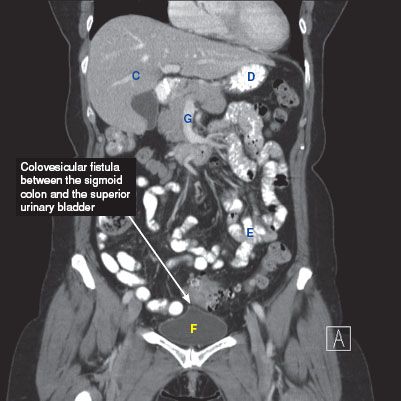
FIGURE 8.5 B
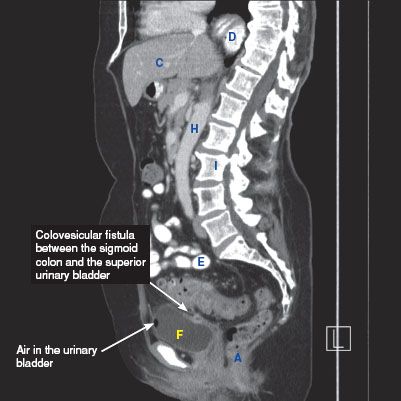
FIGURE 8.5 C
Colorectal Cancer
 Hereditary colorectal cancer syndromes
Hereditary colorectal cancer syndromes
• Make up 5% to 10% of all colorectal cancers
• Autosomal dominant
 Hereditary nonpolyposis colorectal cancer (HNPCC) also known as Lynch syndrome
Hereditary nonpolyposis colorectal cancer (HNPCC) also known as Lynch syndrome
• Most common inherited colorectal cancer (2% to 4% colorectal cancers)
• Amsterdam criteria
 Three relatives with histologically proven colorectal CA (one first degree)
Three relatives with histologically proven colorectal CA (one first degree)
 Two successive generations
Two successive generations
 One diagnosed prior to the age of 50 years
One diagnosed prior to the age of 50 years
• DNA mismatch repair
• 50% to 85% lifetime risk of colon cancer
• Extracolonic manifestation: Tumors of endometrium, ovaries, stomach, small bowel, hepatobiliary tract, pancreas, ureter, renal pelvis
 Familial adenomatous polyposis (FAP)
Familial adenomatous polyposis (FAP)
• Second most common familial colorectal cancer
• Hundreds to thousands of adenomatous polyps
• APC gene mutation chromosome 5
• Almost all patients will develop colon cancer
• Mean age polyposis at 15 years of age
• Extracolonic manifestation: Duodenal polyps (periampullary cancer), desmoid tumors, epidermoid cyst, mandibular osteomas (Gardner’s syndrome), central nervous system tumors (Turcot syndrome)
 Attenuated FAP
Attenuated FAP
• Fewer polyps
• Later age onset (30 years)
• 70% lifetime risk for colon cancer
 Peutz–Jeghers syndrome
Peutz–Jeghers syndrome
• Hamartomatous polyps
• Polyps of small intestine, rectum, colon
• Melanin spots in buccal surface
 Juvenile polyposis syndrome
Juvenile polyposis syndrome
• Hamartomatous polyps
• Hundreds of polyps in rectum or colon
• May degenerate into adenoma and carcinoma
Diagnosis
 Screening
Screening
• For average risk start screening at the age of 50 years
• More frequent screening if history of polyps, colon cancer, inflammatory bowel disease, family history of colon cancer
 Preoperative evaluation
Preoperative evaluation
• CT chest, abdomen, pelvis
• Colonoscopy (synchronous tumors ∼5%)
• Rectal cancer—endorectal ultrasound
• CEA level
Treatment/Management
 Resection
Resection
 Twelve lymph nodes required for adequate staging
Twelve lymph nodes required for adequate staging
 ± adjuvant chemotherapy
± adjuvant chemotherapy
RADIOLOGY
Colon Cancer
 Plain film/contrast enema findings
Plain film/contrast enema findings
• Annular cancers manifest as shouldering with an irregular narrow lumen
• Polypoid cancers usually present as intraluminal masses that protrude from the wall into the lumen of the colon
• Obstruction is much more common on the left due to its smaller caliber compared to the right hemicolon
 CT findings (Fig. 8.6)
CT findings (Fig. 8.6)
• Enhancement of cancer
• Heterogeneous enhancement with abscess formation (secondary to perforation)
• Calcification may be seen with mucinous adenocarcinomas
• Infiltration into the surrounding pericolonic fat can indicate extension of tumor outside of the colonic serosa and local invasion
• Retroperitoneal lymph nodes or pelvic nodes greater than 1 cm in the short axis, or clusters of intra-abdominal nodes may indicate regional lymph node metastases
FIGURE 8.6 A,B
A. Psoas muscle
B. Small bowel loops
C. Vertebra
D. Liver
E. Portal vein
F. Right common iliac artery
G. Stomach
H. Spleen
I. Bladder
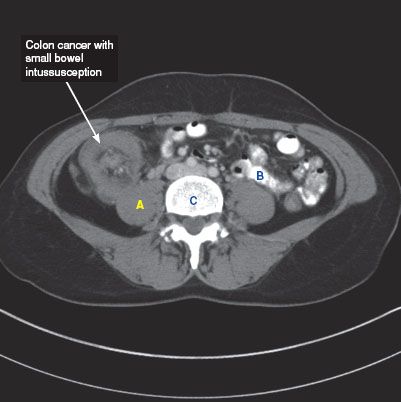
FIGURE 8.6 A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree