Fig. 20.1
The proper stenting technique for the treatment of left main ostial lesions
Guidance of Intravascular Ultrasound (IVUS)
IVUS provides much quantitative and qualitative information regarding coronary artery lesions. It is often difficult to evaluate the actual size of the LMCA via angiography. Often, the left main trunk is short and lacks a normal segment for comparison purposes. In addition, the contrast in the aortic cusp sometimes obscures the ostium, and “streaming” of the contrast may result in a false impression of luminal narrowing. Furthermore, angiography underestimates the stenosis severity. IVUS before stenting, therefore, provides useful information regarding the selection of the adequate size of balloons and stents and regarding the accurate amounts and extent of calcification, which contribute to the change in the treatment modality in 40 % of non-LMCA lesions.
Distal Bifurcation Lesions
Due to the technical difficulties involved, stenting for the ULMCA bifurcation disease should be performed only by highly skilled interventional cardiologist working with patients who understand the risk to benefit ratio of the percutaneous approach. During the procedure, the occlusion of the side branch resulting from plaque shifting or stent strut indicates the acute closure of the ostium of the left anterior descending artery or left circumflex artery, which can lead to disastrous clinical events. Park et al. reported that stenting with or without debulking for LMCA bifurcation stenosis was performed in selected patients with safety and technical feasibility.
Clinical Data
By contrast to excellent long-term angiographic and clinical outcomes of LMCA ostial/shaft lesions treated by PCI with stenting, distal LMCA bifurcation lesions are still challenging to the treating physician and showed less favorable outcomes with PCI. Cumulative evidence suggested that results are less favorable when distal LMCA lesions are treated by two-stent complex techniques as compared to single-stent crossover technique [23, 24]. Even with distal bifurcation treatment, single crossover techniques with optional kissing balloon showed favorable outcomes of low TLR rate less than 5 % equivalent to results obtained with DES for ostial or mid-left main lesions. In contrast, two-stent complex techniques are still challenging with a high TLR rate more than 20 %, mainly related to side-branch restenosis. In large observational study comparing the outcomes between ostial/shaft and distal bifurcation lesion in 1,111 patients with LMCA stenting with DES, distal left main bifurcations were associated with a 50 % excess risk of adverse outcomes, which was mainly driven by bifurcation lesions that were treated with complex stenting, as compared to ostial or midshaft lesions [25]. There was no difference in each and composite clinical outcomes were observed between patients with single-stent bifurcation treatment and those with ostial or midshaft LMCA lesions.
Techniques for Left Main Distal Bifurcation
For treating distal LMCA bifurcation lesions, the relative benefits of provisional stenting of bifurcation lesions, in which a single main-vessel stent is deployed and side-branch stenting is only used in cases of suboptimal angiographic results, as compared with a complex approach, in which stenting is performed in both the main and side branch, have been a long-standing debate for which there is now a general consensus [3]. A single-stent technique, in which a stent is placed across the side branch (usually the circumflex coronary artery), is preferred in patients with diminutive or normal-appearing side branches [26]. However, if the operators decide on a single-stent approach, it is almost always possible to place second stent on the side branch if stenting crossover does not yield an optimal result. A number of two-stent techniques, various levels of complexity and indications, can be used to treat distal LMCA bifurcation stenosis (Fig. 20.2).
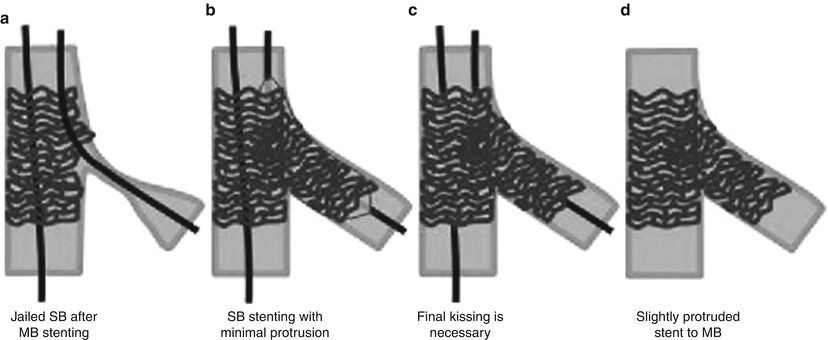
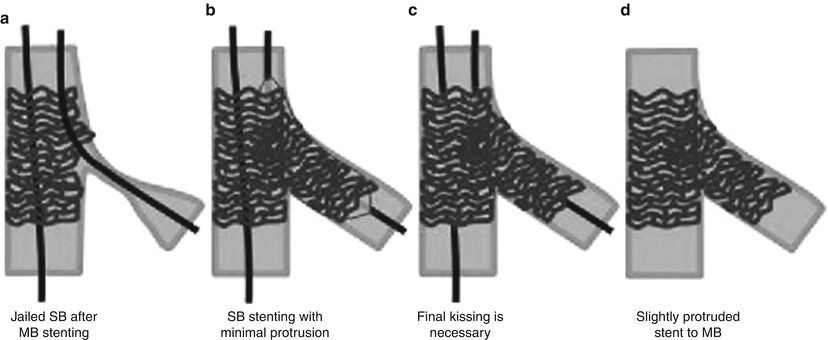
Fig. 20.2
Stenting crossover with optional T-stenting
Single-Stent Techniques with Optional T-Stenting
For bifurcation lesions, the single-stent technique, in which a stent is placed across the side branch (SB, usually the LCX), is preferred in patients with diminutive or normal-appearing side branches. If the operators decide to use the single-stent approach, however, there is almost always the possibility of placing a second stent on the LCX in case the result is not optimal or adequate. This condition is defined as provisional stenting. A wire in the LCX before stenting is usually needed in the cases with (1) narrowing at the ostial LCX; (2) severe stenosis of the main branch (MB), with a large plaque burden at risk for plaque shifting; (3) narrow angle of the SB origination; and (4) deterioration of the SB ostium after the predilatation of the MB. The predilatation of the MB is usually recommended to ensure optimal balloon expansion and easy stent delivery. The predilatation of the SB is performed only if it is diseased or if it significantly deteriorates after the dilatation of the MB (threatened SB occlusion). Many SBs without a significant disease do not require predilatation. If the procedural result of the SB after MB stenting is not satisfactory, dilatation of the SB and kissing balloon inflation are performed. If the results are not acceptable (suboptimal results, plaque shifting with 75 % residual stenosis, or flow-limiting dissection) after kissing balloon inflation, SB stenting is then performed. Like kissing balloon inflation, provisional stenting in the LCX is selectively used when suboptimal dilatation or significant dissection occurs after kissing balloon inflation. As a bailout procedure for suboptimal results or significant dissection at the ostial LCX, the provisional T-stenting and reverse-crush techniques are commonly used. The provisional T-stenting technique is a strategy involving T-stenting in the LCX with the second stent after MB stenting, as shown in Fig. 20.2. Final kissing balloon dilatation after T-stenting is a mandatory step for the optimal final result. Reverse crush is a variation of the crush technique, in which provisional LCX stenting with a T-shape configuration is performed after MB stenting, which is similar to provisional T-stenting (Fig. 20.3). After the removal of the LCX wire and the balloons, however, the LCX stent is crushed within the MB stent. The final step of kissing balloon inflation after sequential high pressure in both branches with noncompliant balloons is also mandatory for successful results. Furthermore, in both provisional SB stenting strategies, the minimal protrusion of the LCX stent into the MB may be beneficial to minimize the destruction and underexpansion of the stents. An attempt should also be made, however, to avoid incomplete lesion coverage.
Fig. 20.3
Stenting crossover with optional reverse-crush stenting
Complex Two-Stent Techniques
A number of two-stent techniques applicable to the treatment of distal LMCA bifurcation stenosis are available, with various levels of complexity and indications. These techniques fall mainly into four broad categories: T-stenting, crush stenting, culotte stenting, and simultaneous kissing stenting (SKS) or Y-stenting (Fig. 20.4 ). There is little consensus and data on which of these two-stent techniques is the best. As restenosis or stent thrombosis can be catastrophic in LMCA locations, all measures for achieving an optimal final result should be considered.
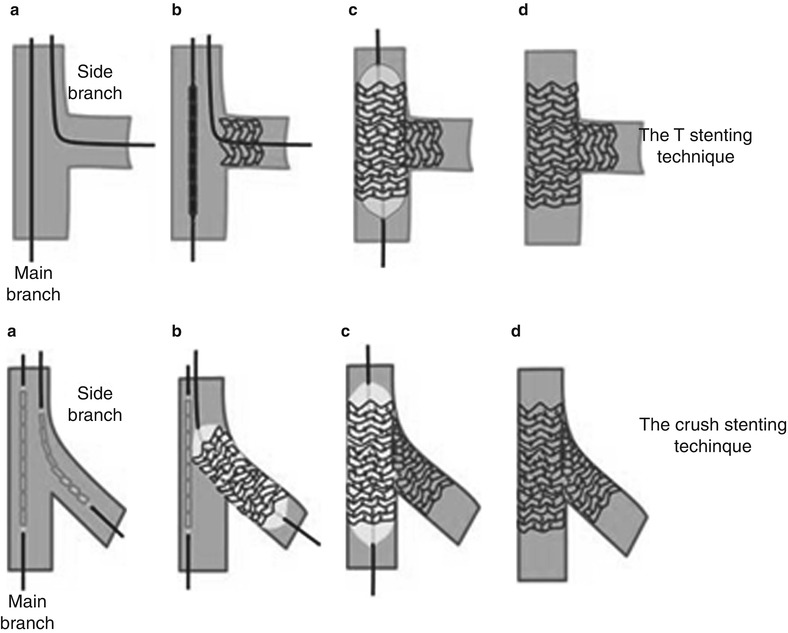
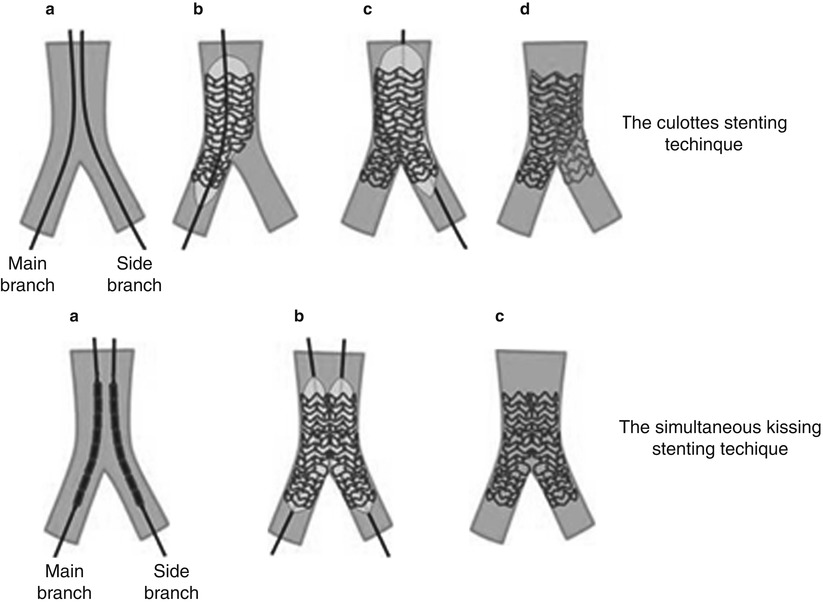
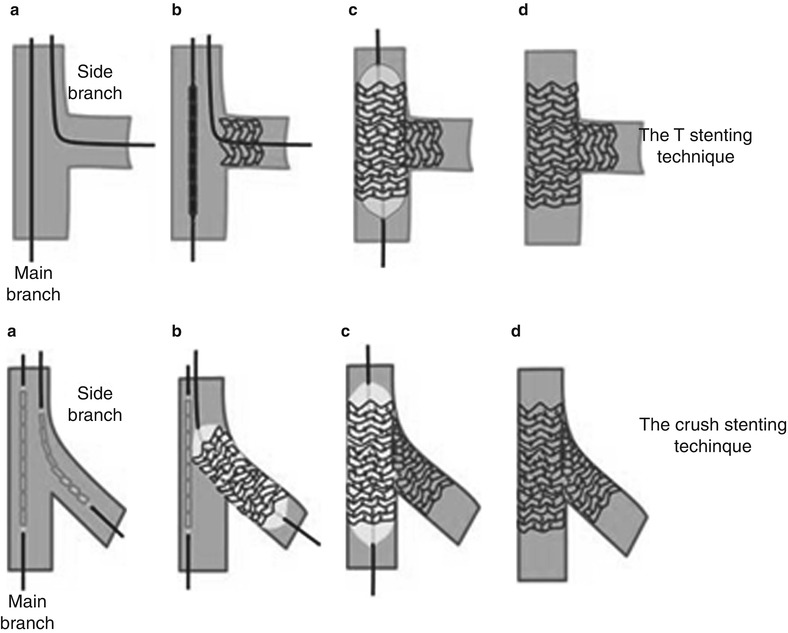
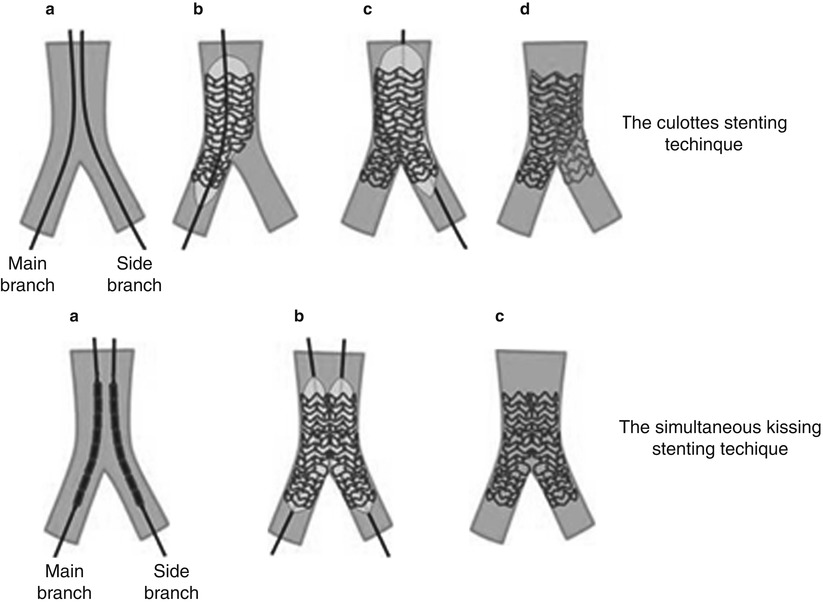
Fig. 20.4
Complex stenting techniques used to treat left main coronary artery stenosis involving distal true bifurcation lesions
The Classic T-Stenting Technique
The LAD and LCX are wired. A stent is positioned at the ostium of the SB (LCX) without protruding into the MB (LMCA to LAD). Once the SB stent is deployed, the balloon and wire are removed from the SB, and a second stent is deployed in the MB (LMCA to LAD). The SB is rewired, and final kissing balloon dilatation is performed. The modified T-stent technique involves the simultaneous placement of the stents in the two vessels, but with the SB stent being deployed first.
The Crush Techniques
The MB and SB are wired and predilated. Stents are placed in both vessels, with the SB stent slightly protruding (2–3 mm) proximal to its ostium and the LMCA stent extending into the MB to fully cover the lesion. The SB stent is deployed, the balloon and wire are removed from the SB, the MB stent is deployed, the SB is rewired, and final kissing balloon inflations are performed.
The Culotte Technique
The more angulated branch (usually the LCX) is stented first, with the stent protruding back into the LMCA; the MB (usually the LAD) is wired through the SB stent, the struts of the SB stent are dilated, and the MB is stented; the wire is removed from the SB and the SB is rewired; and final kissing balloon dilatations are performed. The disadvantage of this technique is that there is a heavy concentration of metal due to the double layer of stents in the LMCA proximal to the carina. The initial results of the use of the culotte technique with BMS were discouraging, but better results were achieved with DES.
The SKS Technique
This technique includes V- or Y-stenting. In V-stenting, stents are advanced into both the LAD and LCX and are pulled back to touch each other, forming a proximal carina. If the stents extend proximal to the bifurcation and into the LMCA, they form a double lumen; this is then considered SKS or Y-stenting, or double-barrel stenting. Sequential followed by final kissing balloon dilatation is performed for optimal results. The main advantage of this technique is that access to both branches is never lost during the PCI. On the other hand, its main disadvantages are (1) the difficulty of placing a stent (if necessary) proximal to this double barrel, (2) subsequently engaging the ostium of the LMCA with a diagnostic or guiding catheter, (3) rewiring the LAD or LCX, and (4) the large amount of metal that is left in the LMCA exposed to the free lumen without direct wall contact. Another variation is the skirt technique, which involves V-stenting the ostia of the LAD and LCX and placing a third stent in the distal LMCA. In the classical Y-stent approach, one stent is crimped over two balloons, but a gap is inevitable at the transition zone between the stents.
Dedicated Bifurcation Stents
Because of the measurable risk of restenosis and revascularization after complex stenting, the use of dedicated LMCA bifurcation stents is currently being explored [27]. The Axxess Plus LM system is currently an available dedicated LMCA device.
Current Evidence of CABG vs. Stents Therapy
Patient Selection: Possible Indication or Contraindication for PCI or CABG
The choice of PCI or CABG for treatment of unprotected LMCA disease depends on several clinical and anatomic features, making optimal patient selection crucial for appropriate treatment of LMCA disease and achievement of favorable long-term outcomes. In patients with very complex anatomic features, which are not feasible for stenting, and concomitant diffuse multivessel disease, CABG is preferred so as to avoid procedural and future thrombotic risks and to provide more complete revascularization. However, in patients with relatively simple LMCA disease, such as ostial/shaft LMCA disease or isolated LMCA disease (with or without one- or two-vessel involvement), PCI is an alternative and in some cases a preferred strategy in order to reduce surgical risks (e.g., stroke and in-hospital events following major surgery).
LMCA lesion characteristics (severe calcification, distal LMCA involvement with relation to major branches), the extent of extra LMCA (concomitant multivessel disease, the status of distal runoff), and patient clinical characteristics (age, diabetes, ejection fraction, and other comorbidities) are important in patient selection. Patient/physician preference is also influential. Several clinical and angiographic factors generally considered for proper choice of patients for the PCI or CABG treatment are listed in Table 20.1.
Table 20.1
Relative indication or contraindication of PCI and CABG for treatment of unprotected left main coronary artery disease
Possible indication of PCI |
Ostium or midshaft lesions |
Distal left main disease anatomically suitable for stenting with intact left ventricular function |
Isolated left main disease |
Unstable hemodynamic conditions requiring urgent revascularization: bailout procedure, acute myocardial infarction, or cardiogenic shock due to left main stenosis |
Serious comorbidity (high surgical risk): chronic lung disease, poor general performance status, advanced age such that major surgery cannot be tolerated, limited life expectancy, prior bypass surgery, unsuitable coronary anatomy for bypass grafting |
Patient refusal of surgery |
Strong recommendation of CABG |
Complex coronary anatomy unsuitable for stenting: severe calcification, severe tortuosity, total occlusions at other major epicardial coronary arteries (≥ 2), multiple and diffuse long coronary lesions, complex in-stent restenosis unsuitable for repeat stenting procedure |
Severely compromised left ventricular function |
Extensive peripheral vascular disease unsuitable for placement of a guiding catheter or intra-aortic balloon pump |
Contraindication to antiplatelet therapy including aspirin, heparin, or thienopyridine |
Patient refusal of stenting |
Registry and Meta-analysis Data
Several small-sized observational studies comparing stents and CABG for unprotected LMCA disease showed that in-hospital or early clinical outcomes favored for stenting due to relatively higher incidence of periprocedural MI or stroke by CABG, but mortality or composite hard end points (death, Q-wave MI, or stroke) were similar in the PCI and the CABG groups. The risk of TVR was consistently higher with PCI than with CABG [28–31]. The MAIN-COMPARE registry was the largest, multicenter observational study comparing stenting and CABG for unprotected LMCA disease [32], in which a total of 2,240 patients with unprotected LMCA disease who underwent stenting (BMS, 318, and DES, 784) or CABG (1,138) were analyzed. Up to 5 years, the adjusted, long-term risks of death and the composite outcome of death, Q-wave MI, or stroke were not significantly different for patients undergoing stenting vs. CABG, but repeat revascularization was significantly higher in patients receiving stenting [33]. Despite of these cumulative data, whether or not the results achieved with coronary stenting would be stable for 5–10 years remains to be determined in unprotected LMCA disease. Recently, very long-term comparative clinical data with follow-up durations of 5–10 years has been reported. The ASAN–MAIN (ASAN Medical Center–Left MAIN Revascularization) registry is the longest follow-up study to report 10-year results of BMS and 5-year results of DES as compared to concurrent CABG [34]. In these two follow-up cohorts, the adjusted risks of death and the composite of death, Q-wave MI, or stroke were similar between the two groups. However, the rate of TVR was significantly higher in the stenting group.
Several meta-analyses or merged analyses comparing two primary revascularization therapies for LMCA disease are currently available. Systemic review conducted by Taggart et al. suggested that early (in-hospital, to 30 days) and longer-term (1–2 year) mortality rates were better after CABG (early, 2–4 %, average 3 %; late, 5–6 %, average 5 %) than PCI with BMS (early, 0–14 %, average 6 %; late, 3–31 %, average 17 %) or DES (early, 0–10 %, average 2 %; late, 0–14 %, average 7 %) [35]. Takagi et al. reported a meta-analysis of 2,181 patients with unprotected LMCA disease who received stenting (n = 1,006) or CABG (n = 1,175) from six studies (one randomized and five observational studies) [36]. Analytic results demonstrated no significant difference in death rate between stenting and CABG, but a statistically significant increase in repeated revascularization with stenting. Lee et al. also performed a similar meta-analysis (2,905 patients from eight clinical studies; two randomized trials and six observational studies) comparing CABG and PCI with DES for unprotected LMCA disease [37]. Consistent with previous findings, there was no significant difference between the CABG and DES groups in the risk for death or the composite end point of death, MI, or stroke, but the risk for repeat revascularization was significantly lower in patients undergoing CABG.
Randomized Trials
Although there have been cumulative large data evidence comparing PCI and CABG for unprotected LMCA disease, most of these are derived from real-world registry database. In addition, results of systemic review and meta-analysis should be interpreted with caution and regarded as only exploratory findings, given the limited number of patients, selection or publication bias in the literature reviewed, and caveats on internal validity of the included clinical studies. Therefore, pure treatment effects among two primary revascularization methods can be achieved from randomized clinical trials, although the use of composite end point, the small number of patients, and the limited duration of follow-up have biased the study findings. Table 20.2 summarizes the currently available randomized trials comparing PCI with stent implantation and standard bypass surgery for unprotected LMCA disease [38–41]. In the future, over these available findings, larger, ongoing, international randomized trial of EXCEL (Evaluation of Xience Prime vs. Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) might provide more confirmative information regarding the relative efficacy and safety of PCI with DES and CABG for patients with unprotected LMCA disease.