Case presentation
A 15-year-old male presents to the Emergency Department with a complaint of “severe headaches” for the past week. He states he has had cough, which is worse at night, and congestion for the past 2 weeks. He has had minimal rhinorrhea that was initially clear, then green, and is now clear again. He initially had a temperature of 101 degrees Fahrenheit, but this resolved after 2 days. He denies vomiting, sore throat, ear pain, vision changes, weakness, difficulty ambulating, or neck pain. There is no report of trauma. He states that the headache has been waking him up from sleep and has been present in the morning for the past 3 days. There is minimal relief with over-the-counter ibuprofen. His physical examination reveals a well-appearing patient who is afebrile and has unremarkable vital signs. He is normocephalic and atraumatic. There is no photophobia and his extraocular muscles are intact without proptosis or conjunctival erythema. There is no cobblestoning. He has mild nasal congestion with rhinorrhea; the nasal turbinates are mildly edematous. There is no facial edema, tenderness, signs of trauma, or erythema. His neurologic examination is nonfocal.
Imaging considerations
Routine imaging for suspected routine sinusitis is not recommended, as this is a clinical diagnosis that follows strict criteria. The majority of children with uncomplicated upper respiratory tract infection who undergo imaging of the paranasal sinuses, whether plain radiography, noncontrast computed tomography (CT), or magnetic resonance imaging (MRI), will have abnormal findings, including air-fluid levels and mucosal thickening. , While the findings of clear paranasal sinuses may exclude sinusitis, abnormal findings do not secure a diagnosis of sinusitis. Imaging should be reserved for patients with potential sinusitis who have a suspected complication from sinusitis or if surgical intervention is planned.
Plain radiography
The American Academy of Otolaryngology and Head and Neck Surgery does not recommend the routine use of radiography for the diagnosis of uncomplicated acute bacterial sinusitis. , Plain radiographs have been reported to have a sensitivity of 76% in acute bacterial sinusitis. , ,
Computed tomography
The sinuses can be visualized with non–contrast-enhanced CT, which provides an excellent assessment of bony detail. However, routine use is not indicated to diagnose clinical sinusitis. Rather, this modality should be reserved for patients with suspected complications from sinusitis, and intravenous contrast–enhanced CT is appropriate in these cases. The most common complication from acute bacterial sinusitis involves the orbit and occurs in children younger than 5 years of age who have ethmoid sinusitis. , , Intracranial complications, such as subdural empyema, epidural empyema, venous thrombosis, and brain abscess, have been described in the literature and should be considered in patients who present with severe headache, photophobia, or focal neurologic findings. , , , Non–contrast-enhanced CT may be utilized when planning sinus surgical procedures.
Magnetic resonance imaging
This imaging modality is not usually utilized in imaging acute sinusitis. However, in patients with suspected intracranial complications, intravenous contrast–enhanced MRI is an appropriate imaging modality to utilize. ,
CT versus MRI
Intravenous contrast–enhanced CT has been the most commonly utilized imaging modality in patients with sinusitis who have suspected complicatons. However, in cases of suspected intracranial complications, MRI is preferred. ,
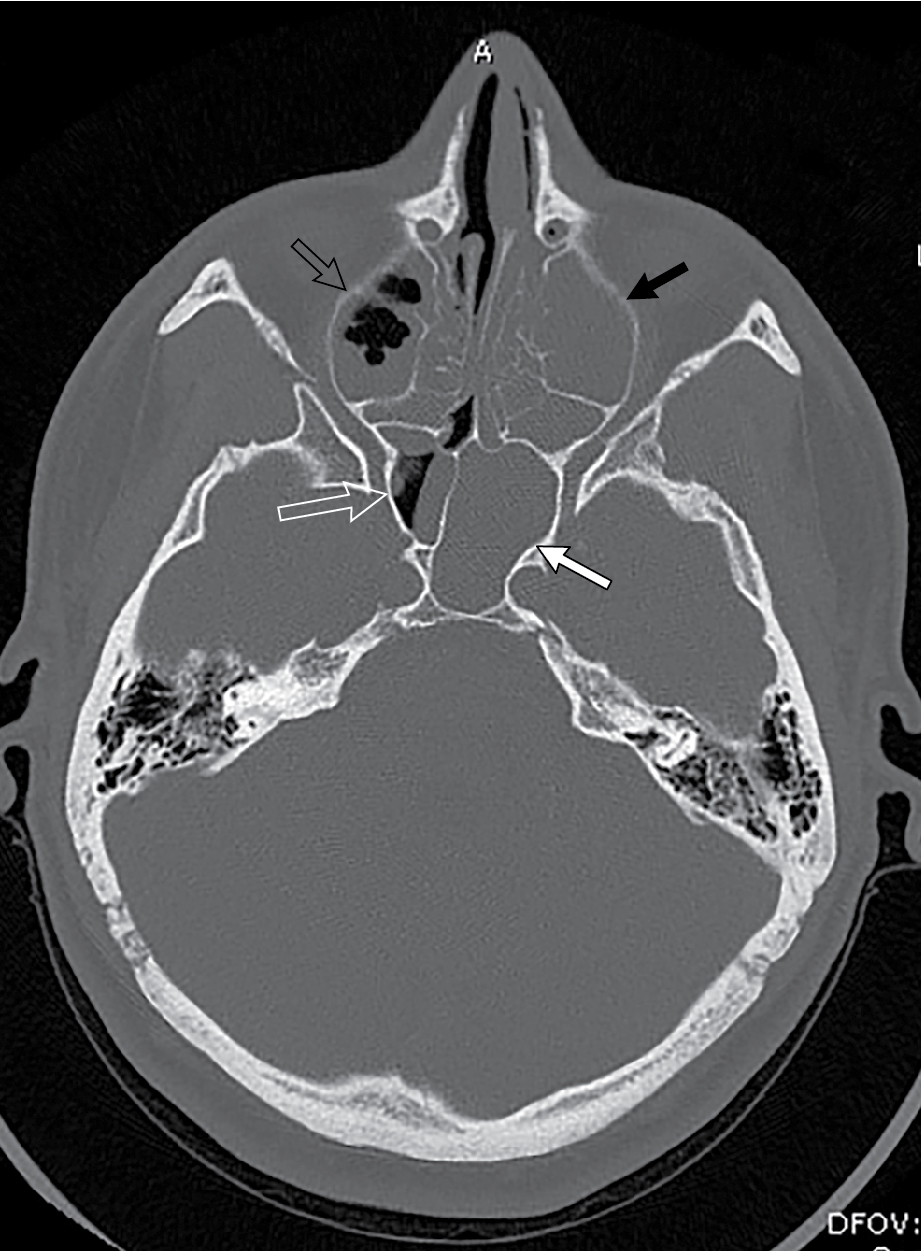
Imaging findings
Given the patient’s concerning history of wakening in the middle of the night and first morning headache, there was concern that the headache was not related to the patient’s apparent upper respiratory tract infection. The physical examination was not suggestive of an infectious complication, such as orbital cellulitis or brain abscess. It was decided to obtain a non–contrast-enhanced CT scan of the head. Selected images are provided here. There is extensive mucosal thickening and areas of sinus opacification throughout the paranasal sinuses ( Figs. 72.1 and 72.2 ), but the brain, ventricles, and skull are all unremarkable on imaging.