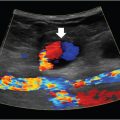
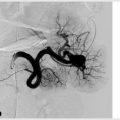
4 Lines, Tubes, and Drains Familiarity with lines and drains is a must for IR trainees. These procedures, while considered bread and butter by many, have the potential to create headaches if not approached with diligence. Take some time to learn about the different types of equipment, the indications for each, and the complications which may arise. While many different specialties can place central lines, those placed by IR have greater technical success and are associated with fewer complications. The use of imaging guidance decreases the risk of procedural complications, and adhering to sterile technique in the controlled environment of the IR suite reduces the risk of infection. Practices vary a great deal from hospital to hospital, both by the preferences of referring physicians and the policies of the IR department. The guidelines presented in this chapter should be taken with a grain of salt, as they may vary depending on your practice setting. Referrals for central venous access are common in IR. Given the volume of requests, many centers will allow these procedures to be scheduled without a formal consultation. Central line placement is relatively straightforward and does not require an extensive work-up (Procedure Box 4.1). However, there are some important preprocedural steps that must not be overlooked. Peripherally inserted central catheters (PICCs) can be placed bedside without fluoroscopic guidance, however, the malposition rate is higher as a result. After accessing a peripheral vein, a peel-away introducer is inserted. The wire is positioned at the junction of the SVC and right atrium under fluoroscopy, and clamped with a hemostat at the hub of the introducer. The catheter is then cut to the appropriate length and inserted through the introducer. The introducer is peeled away, leaving the catheter in place. The hub can then be secured to the skin. Tunneled catheters and ports placed by IR are typically inserted via the IJV, using ultrasound guidance. Ideal IJ access for tunneled catheters and ports is just above the clavicle. The desired catheter course includes a gentle curve of the catheter from the skin insertion site to the termination in the right atrium. Depending on the line type, the catheter is either cut to the desired length, or a predetermined length is used. Over the wire, a peel-away introducer is inserted. For a tunneled catheter, a skin nick is created approximately 2 to 3 fingerbreadths below the clavicle, through which the catheter is tunneled. After placing the cuff beneath the skin at the skin nick site, the tip of the catheter is inserted all the way into the sheath, which can then be peeled away. After ensuring the tip is in the correct location, the catheter is flushed with heparin solution and secured to the skin with suture. When a port is placed, a subcutaneous pocket is created at the distal end of the tunnel where the port will reside. The pocket will need to be made just big enough to fit the reservoir, and no greater, as ports can flip if not snug in the pocket. The catheter portion is placed in the same way as a tunneled catheter. The catheter is cut to length, attached to the reservoir, flushed, and then inserted under the skin, after which the skin can be closed with absorbable sutures. In patients with a history of multiple line placements, review the prior imaging to assess vein patency and history of access complications. Patients who have had prior central lines will often have occluded or thrombosed veins, and will require scrutiny when choosing an appropriate access site. It should also be determined whether a reason exists for a line to not be placed in a specific location. This is especially important when placing PICCs or subclavian vein lines in patients with renal insufficiency, when there may be an anticipated need for dialysis access creation. These types of lines should be avoided in patients who may eventually require a fistula, but if one is absolutely necessary, it should go contralateral to the arm selected for fistula creation. A fistula is most commonly placed in the nondominant extremity, so a PICC/subclavian line should be inserted into the dominant arm. Venous access is broadly divided into four types: PICC, nontunneled central line, tunneled central line, and implantable ports. A PICC is placed via a peripheral vein (basilic, cephalic, or brachial). Indications for a PICC include a long-term need for intravenous antibiotics, total parenteral nutrition (TPN), fluids, and other medications. In many hospitals, these can be placed on the floor by a team of specially trained nurses and physician extenders. IR is typically consulted for challenging cases, including patients with history of prior occlusions, failure of bedside placement, those requiring sedation, and neonates/infants. A PICC can remain in place for a duration of weeks to months. Nontunneled central lines are commonly placed in the internal jugular (IJ), subclavian, or femoral veins for access in emergent situations. These temporary lines are at increased risk for dislodgement and infection the longer they remain in. When long-term central access is necessary, IR may be consulted for tunneled central line placement. Tunneling increases the lifespan of a central line by securing it in place and decreasing the risk of a catheter-related infection. Most tunneled catheters have a cuff that resides in the subcutaneous tunnel, which promotes tissue ingrowth, securing the line in place and limiting migration of bacteria from the skin entry site to the venotomy (▸Fig. 4.1). Fig. 4.1 (A) Tunneled dialysis catheter. The catheter is sutured to the skin at the hub using the two holes. The cuff (arrowhead) is designed to be tucked into the subcutaneous tunnel where it promotes scar formation, securing the catheter within the tunnel. (B) Nontunneled trialysis catheter. Note the lack of a cuff. Both devices are large-caliber catheters which allow for the high-flow rates necessary for dialysis. You may encounter several named tunneled central catheters, including the Hickman catheter, Groshong catheter, and Broviac catheter. These are all small-bore single or multilumen catheters used for central access. While they are very similar in functionality, the key difference is that a Groshong catheter has a three-way valve at its tip that prevents back-bleeding into the catheter as well as prevents air from escaping into the blood. The Hickman catheters need to be flushed with heparin after use, while normal saline flushes suffice for the Groshong catheters. Broviac catheters are also very similar to Hickman catheters. A PowerLine (Bard Access Systems, Salt Lake City, UT) is another type of tunneled catheter which appears similar to a PICC, and is frequently mistaken for one, but is inserted in the chest and has a cuff. The word “power” implies that the line is power injectable, which indicates the catheter can tolerate flow rates necessary for large volume injections, such as those required for intravenous contrast during CT scans. Large-bore tunneled central catheters are necessary for dialysis access and apheresis, which require higher-flow rates (▸Fig. 4.1). A port, also known as “mediport” or “port-a-cath,” is a completely subcutaneous central venous access device, which consists of a reservoir inserted into the subcutaneous tissues of the chest wall connected to a tunneled catheter (▸Fig. 4.2). The reservoir is accessed with the use of a needle when the patient requires blood draws, medication, or fluid administration. These are ideal for cancer patients who require central access for frequent outpatient chemotherapy sessions. Ports vary in size, number of lumens, and flow capabilities, but all function in a similar fashion. Given the lack of any exposed components, these devices carry the lowest risk of infection. Tunneled catheters can be left in place for months, while some ports are left in for years. Aside from PICCs, the hierarchy of vein preference for central venous catheter placement is as follows: right internal jugular > left internal jugular > right external jugular > left external jugular > right subclavian vein > left subclavian. The right internal jugular vein (IJV) is preferred given the straight path down towards the heart. While the subclavian vein has been demonstrated to yield lower rates of infection for nontunneled catheters, this approach carries additional risks during placement, including pneumothorax and the inability to compress any potential bleeding due to the overlying bony clavicle (particularly dangerous if the subclavian artery is inadvertently traumatized). Catheters placed via the subclavian vein are also susceptible to “pinch-off syndrome,” which is when the catheter becomes pinched and occluded as it crosses over the first rib. This condition can eventually lead to catheter fracture, allowing the free tip to travel into the heart. Lower extremity veins, such as femoral or greater saphenous, can be utilized, however these are generally considered higher risk sites for infection, and as such are rarely utilized for long-term access. If all suitable veins are unavailable for use, translumbar, transhepatic, and transrenal access is an option, though these are rarely used. For all central catheters, it is generally recommended to place the line such that the tip terminates in the lower SVC, near the cavoatrial junction. The tip of a tunneled catheter or port can migrate upward by 3 to 4 cm when the patient is standing upright (particularly in women, where breast tissue can pull the catheter hub downward, and thus the tip upward). When the catheter is being placed, the tip should be in the upper to mid part of the right atrium while the patient is in the supine position to account for this migration. Catheter tips placed too high in the SVC are at risk for tip migration (into the contralateral brachiocephalic vein, jugular vein, or azygos vein), as well as greater rate of thrombosis and catheter dysfunction. Catheter tips placed too low in the right atrium can precipitate arrhythmias. Fig. 4.2 The port reservoir resides within a chest wall subcutaneous pocket and can be accessed with a needle. IR generally does not maintain involvement in the care of patients after a line is placed, unless there are complications. Immediate complications are those encountered during the procedure, and are uncommon due to the use of image guidance. Late complications typically involve malfunction of the catheter in some way or another. The risk of pneumothorax is greatest when accessing the subclavian vein, and lowest with ultrasound-guided internal jugular access. A pneumothorax may be recognized during fluoroscopy or on a postinsertion chest radiograph, and only rarely are they large enough for the patient to become symptomatic. If small and incidentally noted, close observation is often sufficient. Larger pneumothoraces may require chest tube placement. If not recognized by the pulsatility of blood return during the initial access steps, an inadvertent arterial puncture is quickly recognized under fluoroscopy when the guidewire courses along the aortic arch (left of the vertebral bodies). As long as only the guidewire is inserted, the needle and guidewire can simply be taken out and pressure held over the arteriotomy before reattempting. If an arterial puncture goes unrecognized and a sheath/dilator is inserted into the artery, this becomes a more serious problem. Depending on the size and location of the inadvertent arterial access, consideration of most appropriate repair should include both endovascular and open surgical options. Although rare, an air embolism can be fatal. This usually occurs after the peel-away sheath’s inner dilator is removed, before the catheter is inserted. Some sheaths have a one-way valve that prevents air from entering, but a good practice is to simply cover the sheath with a finger whenever the dilator is out so air doesn’t get sucked in. In the rare event it occurs, the patient may become short of breath, hypotensive, tachycardic, confused, or experience chest pain. If suspected, place the patient in the left lateral decubitus position and provide 100% oxygen. Severe cases may require hyperbaric oxygen therapy or extracorporeal oxygenation (ECMO) until the air has resolved. Until you have put in many lines and become proficient, one of the challenges of the procedure is ensuring that the catheter runs smoothly in its course. When the catheter bends at an acute angle, it can kink and malfunction. For tunneled catheters, this can be minimized by making sure that the subcutaneous tunnel is an adequate distance lateral to the vein, and that the venotomy where the catheter courses downward is made just about a centimeter above the clavicle. Kinks may be correctable using fluoroscopic manipulation to straighten or reposition the catheter, but sometimes it is just easier to remove it and place a new line. In the rare event of a fracture, as can happen with pinch-off syndrome, the distal fragment may embolize to the heart. An embolized catheter tip should be retrieved if possible. In some cases the risk of retrieval is greater than the risk of leaving the fragment in place. These patients need to be referred to a center experienced in difficult retrievals, and counseled on the risks of removal versus simply leaving it alone before an attempt is made. Infection is a problem which becomes more common the longer the line has been in place. A catheter serves as a nidus for infection, and if left untreated can lead to sepsis. The reported incidence of infected catheters varies widely in the literature. A catheter-related bloodstream infection (CRBSI) should be suspected in the setting of fevers, chills, hypotension, and erythema or purulence around the site of line insertion. Fever is the most sensitive clinical sign. Purulence around the venous line insertion site has a high specificity, but poor sensitivity. CRBSI is diagnosed with blood cultures, ideally two blood samples from the central line and one from a peripheral intravenous. If the culture comes back positive for microbial growth that is not explained by another infectious source (concurrent pneumonia, urinary tract infection, etc.), the diagnosis of CRBSI can be made. Catheter removal is necessary when a line infection is the presumed cause of severe sepsis, hemodynamic instability, or infective endocarditis. Erythema or purulence around the catheter insertion site, even in the absence of culture confirmation, is an indication to remove a catheter. In cases of suspected CRBSI, empiric vancomycin and piperacillin–tazobactam are started after blood cultures are drawn. Antibiotics are deescalated based on the results of blood cultures and sensitivities. Blood cultures are also drawn daily until they are cleared and the patient is afebrile. Catheter salvage may be attempted in select cases. Antimicrobial lock therapy is a method of instilling a high-concentration antibiotics into the catheter lumen and is done in tandem with systemic antibiotics. The patient must not have any purulence or other signs of infection at the exit/tunnel site, otherwise this strategy will not be helpful. Certain microbes including Staphylococcus aureus and Candida are also a relative contraindication. If cultures remain positive for more than or equal to 72 hours after attempted salvage therapy, the catheter must be removed. Exchanging catheters over a guidewire at a venous insertion site is a relatively common practice in cases of uncomplicated CRBSI. If the tip of the removed catheter tip shows evidence of phlebitis, thrombus, or purulence, then exchange is inappropriate and a new catheter must be inserted at a different site. Sometimes a line will malfunction due to a layering of material that accumulates around the catheter. A fibrin sheath can form at the catheter tip, which may impair blood return (common) or cause difficulty flushing (less common). The fibrin sheath acts as a ball valve, which interferes with aspiration. One solution is to infuse tissue plasminogen activator (tPA) into the device, in an attempt to disrupt thrombus at the tip. If this fails, the device can be injected under fluoroscopy, which will often reveal contrast flowing retrograde along the catheter, confirming a fibrin sheath (▸Fig. 4.3). There are three options for fibrin sheath management for tunneled dialysis catheters: (1) catheter exchange, (2) catheter exchange and fibrin sheath maceration with a compliant balloon, or (3) fibrin sheath stripping. Several maneuvers can be performed to strip the fibrin sheath. For example, a snare can be inserted from the groin and the sheath stripped off the catheter from below.
4.1 Central Venous Access
Line Complications
Radiology Key
Fastest Radiology Insight Engine