FIGURE 10.3 Tendons of the ankle and foot. The attachment of various tendons of the ankle and foot are depicted, as viewed from the dorsal aspect (A), lateral aspect (B), and medial aspect (C). |
disrupted. Fracture of the fibula above the level of the ankle joint without accompanying fracture of the medial malleolus indicates rupture of the deltoid ligament. Transverse fracture of the medial malleolus indicates that the deltoid ligament is intact. High fracture of the fibula associated with a fracture of the medial malleolus or tear of the tibiofibular ligament, the so-called Maisonneuve fracture (see later), indicates rupture of the interosseous membrane up to the level of the fibular fracture.
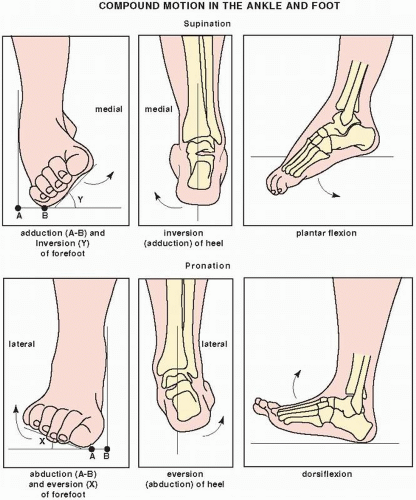
This angle helps diagnose tears of the lateral collateral ligament. However, the wide range of normal values for these measurements may make interpretation difficult, and thus comparison studies of the contralateral ankle should be obtained. Even this method is not always accurate; up to 25 degrees of talar tilt has been reported in people with no history of injury, and occasionally there will be a patient whose ankles exhibit considerable variation in measurement. Many authorities advise that with forced inversion, tilt less than 5 degrees is normal, 5 to 15 degrees may be normal or abnormal, 15 to 25 degrees strongly suggests ligament injury, and more than 25 degrees is always abnormal. With forced eversion, talar tilting of more than 10 degrees is probably pathologic.
by using reformation technique, although direct sagittal sections can also be obtained by placing the patient in the lateral decubitus position. Images in all planes are usually acquired using 3- or 5-mm thin contiguous sections. For three-dimensional (3D) reconstruction, 1.5- or 2-mm contiguous sections are required, although 5-mm sections with a 3-mm overlap can also be used.
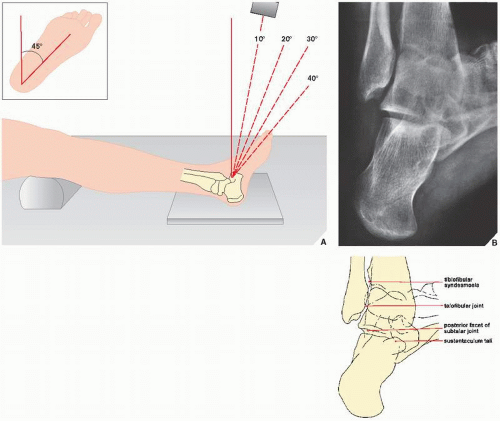
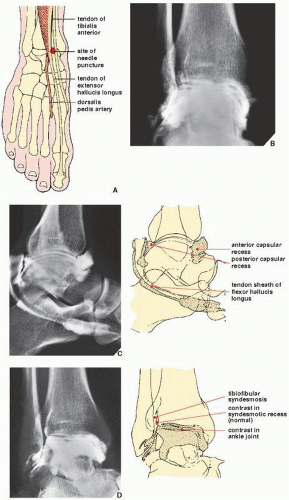 FIGURE 10.12 Arthrography of the ankle joint. (A) For arthrographic examination of the ankle, the patient is supine on the table, with the foot in the neutral position (see Fig. 10.5A). Under fluoroscopic control, the injection site between the tendons of the tibialis anterior and the extensor hallucis longus is marked. Care should be taken to avoid puncturing the dorsalis pedis artery, which should be located by palpation and its site marked on the skin. The needle (preferably 21-gauge) is directed slightly cephalad to avoid the overhanging anterior margin of the tibia. After the joint is entered, approximatley 5 to 7 mL of 60% meglumine diatrizoate or a similar contrast agent is injected for a single-contrast arthrogram. For a double-contrast study, 1 to 2 mL of positive contrast agent and 6 to 8 mL of room air are injected. Films are then obtained in the standard anteroposterior, lateral, and oblique projections. (B) The normal anteroposterior view shows contrast agent outlining the ankle joint, coating the articular surface of the talus and extending into the syndesmotic recess, which normally should not exceed 2.5 cm. (C) On the lateral view, the anterior and posterior capsular recesses are outlined. Filling of the posterior facet of the subtalar joint represents a normal variant, occurring in approximately 10% of cases (see Fig. 10.61C). In approximately 20% of cases, the tendon sheaths of the flexor hallucis longus and flexor digitorum longus opacify on the medial aspect of the ankle. When this occurs, the full extension of the flexor hallucis longus should be noted as it passes proximal to the groove in the talar tubercle and into the groove beneath the sustentaculum tali. Under normal conditions, no tendon sheath opacification should occur on the lateral side of the ankle. (D) Oblique radiograph demonstrates the tibiofibular syndesmosis. No contrast agent should be seen in this area except for normal opacification of the syndesmotic recess. |
 FIGURE 10.14 Anatomic and imaging planes. (A) Anatomic planes of the ankle and foot and (B) CT imaging planes. |
 FIGURE 10.15 Schematic representation of ankle tendons on axial MRI. (Modified from Helms CA et al., 2009.) |
 FIGURE 10.16 MRI of the anterior talofibular ligament. Axial spin-echo MR image (SE; TR 2000/TE 20 msec) through the lateral malleolus and talus demonstrates normal anterior talofibular ligament. (From Beltran J, 1990, with permission.) |
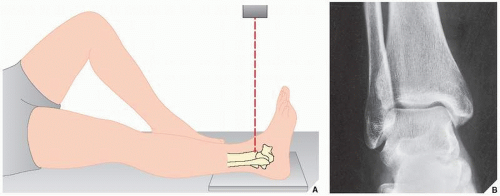
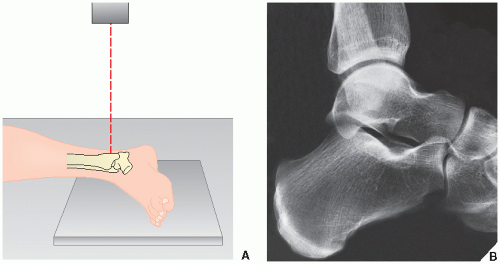
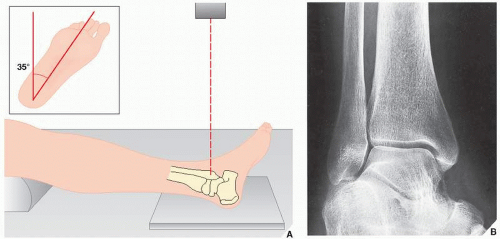
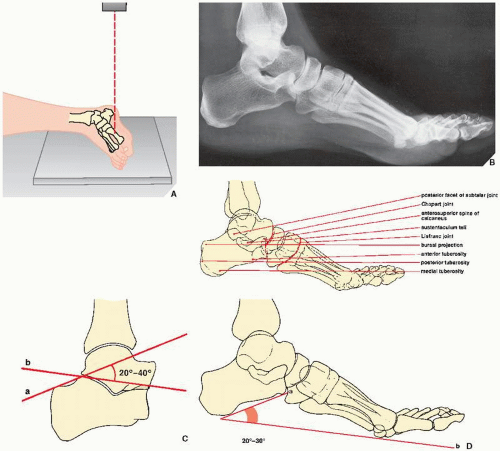
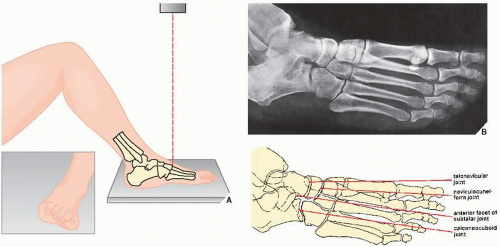
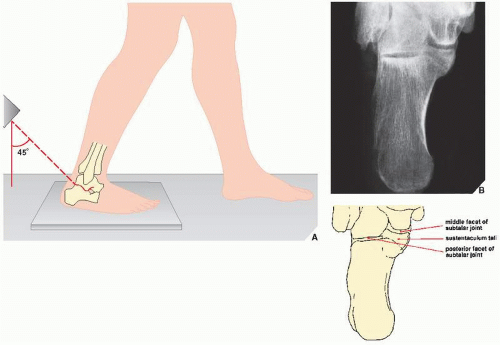
is an important factor in the evaluation of forefoot deformities, because it represents a way to quantify the amount of metatarsus primus varus associated with hallux valgus. On the lateral projection (Fig. 10.22A,B), Boehler angle, an important anatomic relation of the talus and the calcaneus, can be appreciated (Fig. 10.22C). In fractures of the calcaneus, this angle, which normally ranges from 20 to 40 degrees, is decreased because of compression of the superior aspect of the bone (see Fig. 10.73B). This measurement also aids in the evaluation of depression of the posterior facet of the subtalar joint. On the lateral view, calcaneal pitch can also be evaluated. This measurement is an indication of the height of the foot and normally ranges from 20 to 30 degrees (Fig. 10.22D). Higher values indicate a cavus foot deformity. An oblique view of the foot is also obtained as part of the standard radiographic examination (Fig. 10.23). Injuries to the subtalar joint occasionally require special, tangential projections such as the posterior tangential (Harris-Beath) view (Fig. 10.24) or oblique tangential (Broden) view (Fig. 10.25). A tangential view of the sesamoid bones of the great toe (Fig. 10.26) may also be necessary.
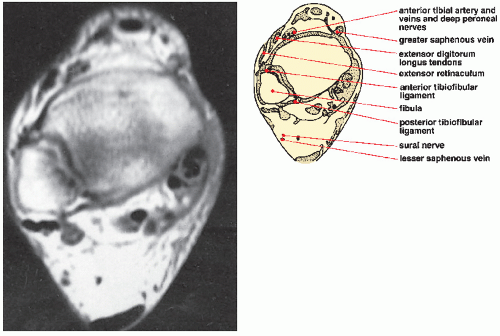 FIGURE 10.17 MRI of the anterior and posterior tibiofibular ligaments. Axial spin-echo MR image (SE; TR 2000/TE 20 msec) shows normal anterior and posterior tibiofibular ligaments. (From Beltran J, 1990, with permission.) |
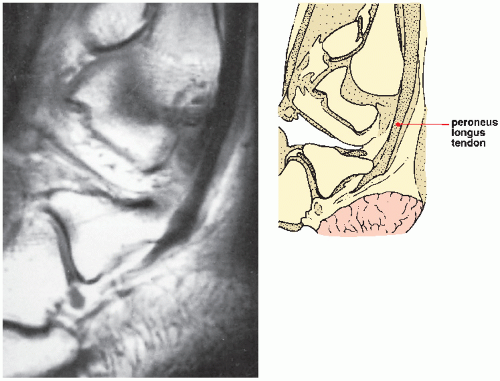 FIGURE 10.18 MRI of the peroneus longus tendon. Sagittal spin-echo MR image (SE; TR 800/TE 20 msec) through lateral malleolus shows normal appearance of peroneus longus as it curves around the lateral malleolus. (From Beltran J, 1990, with permission.) |
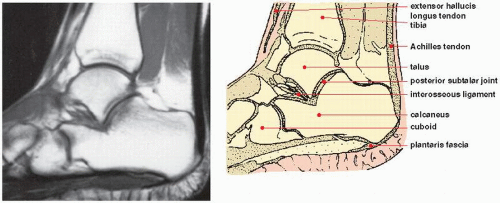 FIGURE 10.19 MRI of the Achilles tendon. Midline sagittal spin-echo MR image (SE; TR 800/TE 20 msec) demonstrates normal Achilles tendon. Note the uniformly low signal intensity of the tendon contrasting with the high signal intensity of the anterior fat pad. (From Beltran J, 1990, with permission.) |
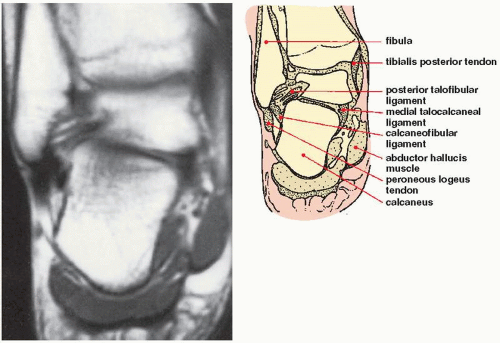 FIGURE 10.20 MRI of the posterior talofibular and calcaneofibular ligaments. Coronal spin-echo T1-weighted MR image of the ankle shows normal posterior talofibular and calcaneofibular ligaments. (From Beltran J, 1990, with permission.) |
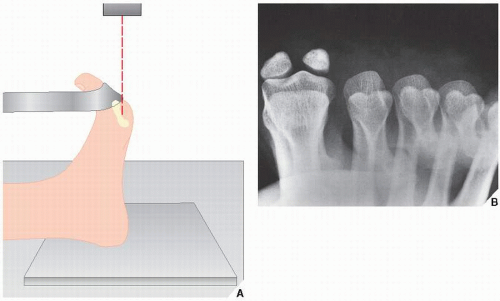
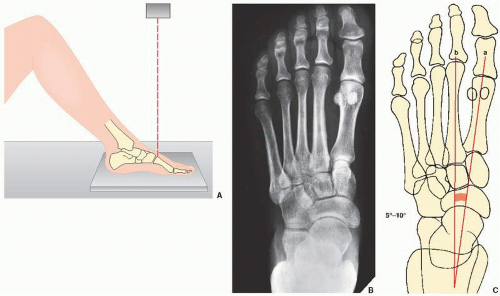 FIGURE 10.21 Anteroposterior view. (A) For the anteroposterior (dorsoplantar) view of the foot, the patient is supine, with the knee flexed and the sole placed firmly on the film cassette. The central beam is directed vertically to the base of the first metatarsal bone. (B) On the radiograph obtained in this projection, injury to the metatarsal bones and phalanges can be adequately assessed. Note that 75% of the talar head articulates with the navicular bone. (For identification of the bones of the foot, see Fig. 10.2.) (C) The first intermetatarsal angle is formed by the intersection of the lines bisecting the shafts of the first (a) and second (b) metatarsals. |
foot injuries that are not always obvious on the standard radiographic examination. CT is especially effective in assessing complex fractures, particularly of the calcaneus. Tenographic examination may also be required to evaluate injury to the tendons of the foot (see previous text and Figs. 10.13 and 10.69B). MRI is now frequently used to evaluate trauma to the foot. During evaluation of MRI of the ankle and foot, it is helpful to use checklist as provided in Table 10.1.
 FIGURE 10.27 Accessory ossicles. (A,B) The numerous accessory ossicles of the foot and ankle can complicate the evaluation of foot injuries by mimicking fracture. Fractures, however, may go undetected when misinterpreted as ossicles, as seen here on the anteroposterior (C) and sesamoid (D) views of the foot, which demonstrate a fracture of the lateral (fibular) sesamoid (arrows) (compare with Fig. 10.26B). |
TABLE 10.1 Checklist for Evaluation of MRI of the Foot and Ankle | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
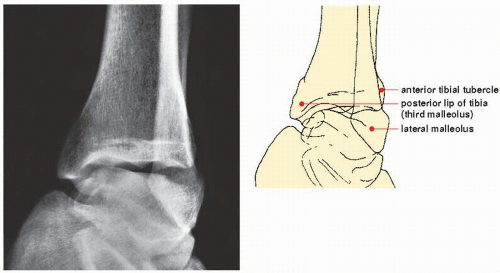
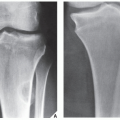
Unimalleolar, when the fracture involves the medial (tibial) or lateral (fibular) malleolus (Fig. 10.32)
Bimalleolar, when both malleoli are fractured (Fig. 10.33)
Trimalleolar, when fractures involve the medial and lateral malleoli as well as the posterior lip (or tubercle) of the distal tibia (the third malleolus) (Fig. 10.34)
Complex fractures, known also as pilon fractures, when comminuted fractures of the distal tibia and fibula occur (Fig. 10.35).
confused with trimalleolar fractures. The following features distinguish pilon fractures from the trimalleolar fractures: the presence of profound comminution of the distal tibia; intraarticular extension of tibial fracture through the dome of the plafond; usual association of fracture of the talus; and usual preservation of tibiofibular syndesmosis. This fracture’s significance comprises the intraarticular extension of the fracture line and its consequent potential to cause late complications of posttraumatic arthritis, as well as nonunion and malunion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree