Stage I
Involvement of a single lymphatic site (I) or a single extralymphatic organ (IE)
Stage II
Involvement of two or more lymph node regions (II) or localized involvement of a single extralymphatic site in association with regional lymph node involvement on the same side of the diaphragm (IIE)
Stage III
Involvement of lymph node on both sides of the diaphragm (III), with extralymphatic involvement (IIIE) or with involvement of the spleen (IIIS) or both (IIIE, S)
Stage IV
Diffused or disseminated involvement of lymphatic or extralymphatic organs including any involvement of the liver or bone marrow, lungs (other than by direct extension from another site), or cerebrospinal fluid
In general HD patients show an overall good prognosis, especially in case of limited-stage disease and absence of unfavorable factors, with a 5-year event-free survival superior to 98 %. More advanced forms and high-risk patients still benefit by the combination of multiagent chemotherapy regimens and radiotherapy, being HD a highly chemo- and radiosensitive disease [5]. The nodular lymphocyte predominant type tends to be more indolent than the classical form, with a propensity for multiple late relapses and risk for transformation into diffuse large B cell lymphoma (DLBCL) [4]. Anyhow, the overall prognosis of this HD subtype remains favorable [10]. Thus, the excellent results yielded so far have led to the necessity for new therapeutic protocols, focusing on the optimization and reduction in treatment-related sequelae in early-stage disease and improvement in survival rate in patients with advanced-stage disease and unfavorable risk stratification.
In this context, instrumental imaging becomes crucial either for disease staging or for a proper treatment response assessment. This fact is confirmed by the introduction of early response to chemotherapy as a predictor to disease outcome in the Children’s Oncology Group (COG) studies [3, 4].
12.1.1 Staging HD
18F-FDG PET has been increasingly incorporated into the diagnostic and therapeutic work-flow of many pediatric malignancies. This imaging modality allows an earlier identification of primary tumors as well as their metastatic spread, thus significantly improving treatment planning and overall survival. In particular, 18F-FDG PET is a well-established modality for the initial assessment of adult and pediatric HD. As a noninvasive imaging technique, it allows for a whole-body detection of all lymphatic and extralymphatic sites of disease. At initial staging 18F-FDG PET/CT shows a sensitivity, specificity, and accuracy of 96.5 %, 100 %, and 96.7 %, respectively, markedly superior to conventional imaging, including computed tomography (CT) [11–13]. This performance is maintained throughout the entire range of histological subtypes of HD that are in general characterized by a high avidity for the tracer [14]. The use of morphological imaging such as CT or even MRI should be anyhow considered in the initial evaluation of HD patients in case of unusual extralymphatic involvement or when bulky masses are detected, in order to better define structural infiltration and plan consolidation radiotherapy.
In HD staging, a crucial site of disease localization is represented by bone/bone marrow. Although the rate of bone marrow involvement is not as high as in adult population, still there is an incidence of 4–6.5 % in more advanced HD stages in pediatric population [15, 16]. Traditionally, bone marrow biopsy (BMB) at the level of the iliac crests was considered as gold standard and should still be performed in case no advanced imaging with PET is available prior to treatment start. Nowadays, the results obtained by 18F-FDG PET/CT in defining bone marrow involvement guarantee a better detection of HD extent and overcome completely the necessity to perform a BMB in case of positive findings [5, 17]. The patterns of bone marrow involvement are variegate and comprise either a multifocal pattern, with three to more lesions located in the axial skeleton or proximal limbs, single foci of 18F-FDG uptake, or diffused heterogeneous uptake with sites of more intense focal involvement [15, 17]. This later pattern should not be confused with the homogenously increased bone marrow activation present in advanced HD cases and consistent with systemic/paraneoplastic symptoms [15]. Recent recommendations in adult lymphoma imaging also support the superior performance of 18F-FDG PET/CT in bone marrow assessment either at an early stage, when the risk of bone marrow infiltration is very low, or in advanced HD, given the high positive predictive value of the modality [18].
As a consequence of the better assessment of HD, 18F-FDG PET/CT determines a significant impact in patient treatment, either by upstaging or downstaging the disease. The percentage of change varies from 9 to 50 % of the cases, but by summarizing the results from different papers [19–25], the cumulative change can be estimated around 20 %.
12.1.2 Treatment Response and Follow-Up
Posttreatment evaluation with 18F-FDG PET/CT is known to be significantly correlated with patient outcome [26]. Its proper application during the course of treatment or after completion of chemotherapy can help identify patients who could benefit from additional therapy and avoid unnecessary treatment in patients with a low risk of relapse and a complete metabolic response [27]. In clinical practice the imaging response, including qualitative criteria such as the metabolic response to treatment, is used as a surrogate for patient outcome [28]. In limited-stage HD, the PET evaluation at the end of treatment has been reported to be highly predictive of PFS and overall survival [29]. Also in advanced-stage HD, consolidation radiotherapy can be safely omitted in PET-negative patients after completion of chemotherapy. In response assessment, a negative 18F-FDG PET after chemotherapy anticipates an excellent prognosis in contrast to a positive scan where the risk of disease recurrence increases significantly [21, 30]. No significantly increased risk of early relapse or progression has been reported in these patients even in those with residual masses on CT, but metabolically silent on 18F-FDG PET [31]. The abovementioned results have led to the new recommendations for the assessment of lymphoma, also known as the Lugano classification [18]. For response assessment in FDG-avid lymphoma, the criteria suggested are based on the 5-point scale (Deauville score) [32], both for clinical practice and research trials including interim and end-treatment evaluation.
In pediatric population response assessment can be obtained either after two cycles of chemotherapy, thus defining the early response, or at the end of treatment (Figs. 12.1, 12.2 and 12.3). In the first case the information is regarded as crucial for the planning, and in different multicenter protocols, the achievement of a complete metabolic response early in time could safely lead to reduction in chemotherapy exposure and/or the omission of radiotherapy [33, 34]. In other cases, response-adapted therapy from the Children’s Cancer Group (CCG) followed a gender-tailored consolidation protocol in advanced HD based on early response on PET [35].
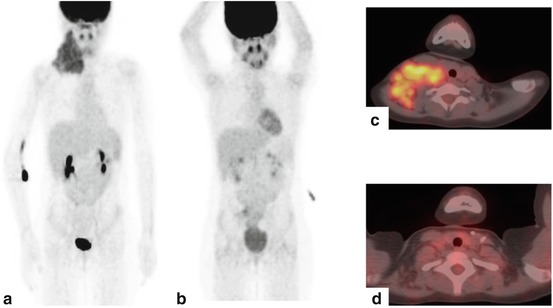
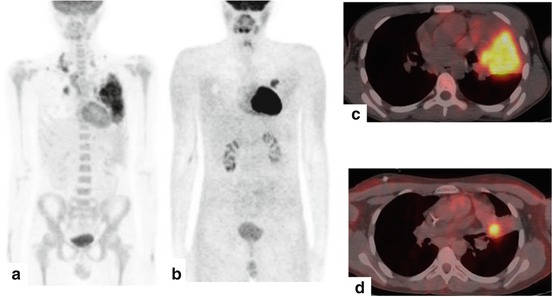
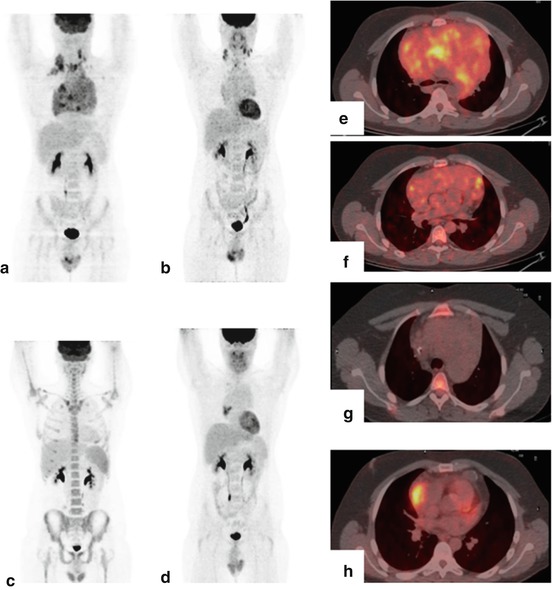
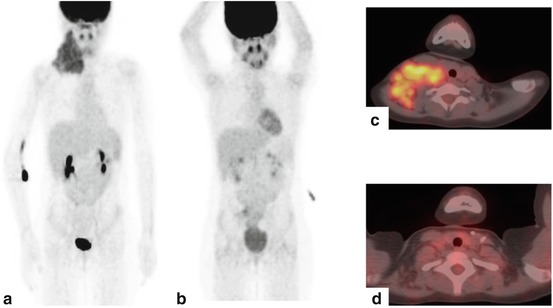
Fig. 12.1
A 12-year-old female affected by Hodgkin’s lymphoma. PET/CT scan on initial staging showed a big lymph-node cluster characterized by intense FDG uptake in the right supraclavicular region (a and c). Repeated study was done after a 2 cycles of chemotherapy (b and d), which showed complete metabolic response to therapy
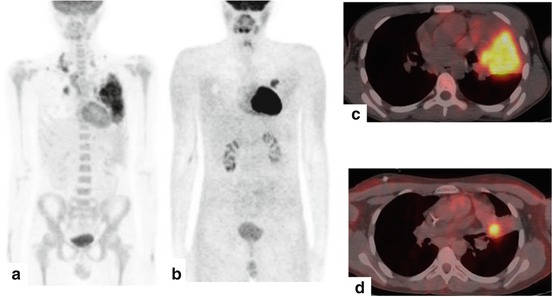
Fig. 12.2
A 11-year-old male affected by Hodgkin’s lymphoma. PET/CT scan on initial staging showed a left lung localization of disease characterized by intense FDG uptake (a and c). Repeated study was done after a 2 cycles of chemotherapy (b and d), which showed an incomplete metabolic response to therapy
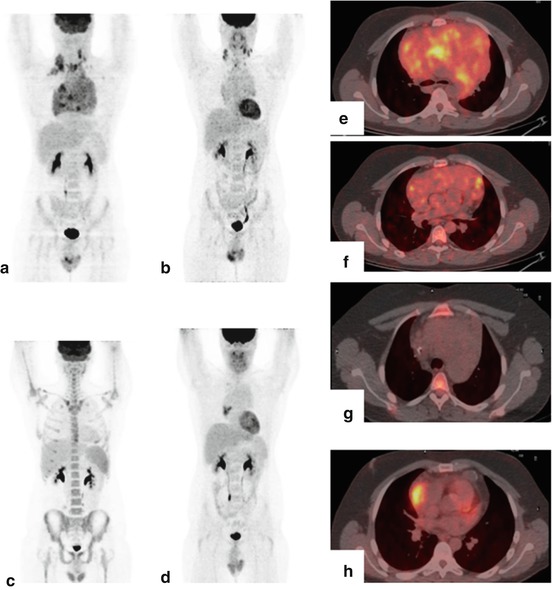
Fig. 12.3
This is a 17-year-old male affected by Hodgkin’s lymphoma. PET/CT scan on initial staging showed increased FDG uptake in a large right mediastinal mass and in laterocervical lymph-nodes. (a and e). Repeated study was done after a 2 cycles of chemotherapy, which showed an incomplete metabolic and morphological response to therapy (b and f). At the end of treatment, PET/CT scan showed a complete metabolic response to therapy (c and g). Six months later, PET/CT showed a mediastinal recurrence of disease (d and h)
As for response criteria in pediatric HD, no universally accepted criteria have been reported. However, many attempts have been done, either by applying the International Harmonization criteria for assessment of FDG PET response or by investigating the 5-point scale [5, 36, 37]. An alternative method to define metabolic response on PET has been proposed by the study group of the EuroNet-PHL-C1 trial (EudraCT 2006-000995-33), after dedicated evaluation of 898 patients [38]. The method gives a quantitative analysis (qPET) computed as an extension of the Deauville scale, resulting more consistent with the continuum in metabolic response observed in reality. This quantification however requires dedicated software, and upon the availability of the nuclear medicine center, qPET can be used as a reliable method for early response assessment in pediatric HD. Otherwise, as for adult lymphoma, the 5-point scale suggested by the Lugano classification is recommended [18].
At the end of chemotherapy, 18F-FDG PET is carried out to determine the need for consolidative radiation therapy and is reported a have a very high and independent prognostic role [3, 26]. Especially in case of positive findings after two cycles of chemotherapy, the use of end-treatment PET is almost mandatory. What is considered to be very high at this point in time is the negative predictive value of the method, whereas the positive predictive value is reported rather variable and can lead to false-positive findings [39]. Therefore, the proper timing for the scanning is defined by the day of the last cycles of chemotherapy and should be comprised between 3 and 4 weeks after the completion of therapy [36].
No consolidated use of 18F-FDG PET/CT exists in the follow-up of pediatric HD, unless end-treatment evaluation shows equivocal findings or noncomplete metabolic response. On counterpart, the integration of PET/CT into radiation treatment planning is advised because of the substantial impact it can have on treatment volumes within the target definition by reducing the risk of acute radiation-induced toxicity and potentially lowering the rate of long-term sequelae, including secondary malignancies [40].
12.2 Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma (NHL) accounts for 60 % of childhood lymphomas and represents about 7.5 % of pediatric cancer; it is rare in infants and has its peak incidence at the age of 7 years [1]. NHL includes a large and very heterogeneous group of systemic malignancies but in childhood and adolescence is an aggressive systemic disease characterized by mature B cell immunophenotype. In particular most pediatric NHL cases belong to one of four categories: Burkitt lymphoma and B cell acute lymphoblastic leukemia (40–50 % of cases), followed by lymphoblastic lymphoma (20–25 %), anaplastic large-cell lymphoma (10–15 %), and diffuse large B cell lymphoma (10 %) [41, 42]. In addition, unlike in Hodgkin lymphoma with only few tumor cells, NHL consists of about 85–99 % of highly proliferative neoplastic cells (Fig. 12.4).
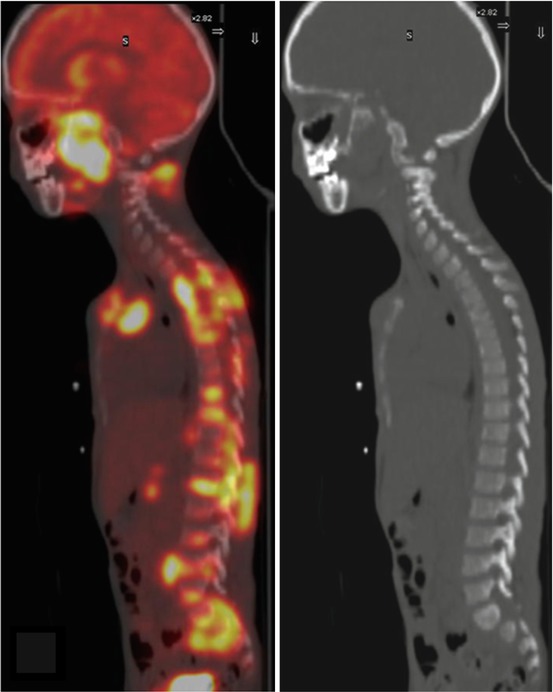
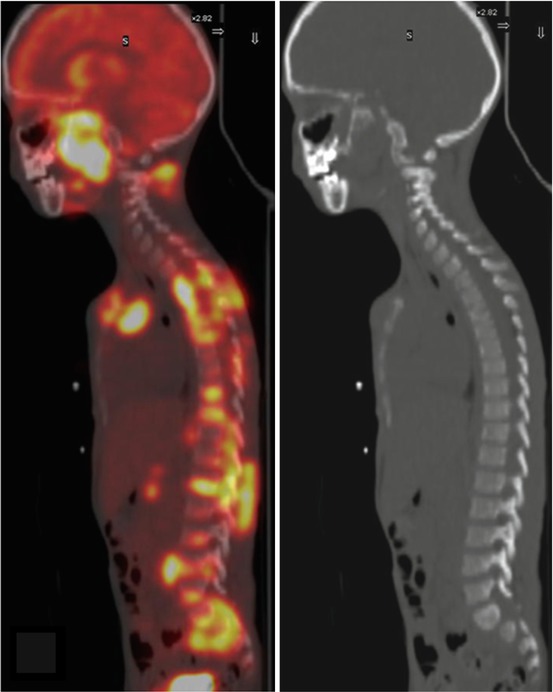
Fig. 12.4
This patient was a 16-year-old male who had Non-Hodgkin’s lymphoma. PET/CT scan on initial staging showed multiple areas of increased FDG uptake in the spine and sacrum, but no abnormal findings on the corresponding CT images
Burkitt lymphoma is an aggressive and rapidly proliferating tumor and doubles within 12–48 h [43, 44], and it often leads to gastrointestinal and urogenital obstructions.
The most common localization of lymphoblastic lymphomas is the mediastinum (large mediastinal mass) followed by the spleen, bone marrow, central nervous system, and peripheral lymph nodes [45].
Anaplastic large-cell lymphomas are characterized by peripheral adenopathy but often show extranodal involvement such as the skin, soft tissues, lungs, and cortical bone [45, 46]. Most children affected by anaplastic large-cell lymphomas carry the ALK-gene translocation. The prognosis of ALK+ patients is better than that of ALK− [47].
Diffuse large B cell lymphoma (DLBCL) is rare in pediatric patients. However, it is the most common lymphoma subtype in patients with congenital, iatrogenic, or acquired immunodeficiency. DLBCL is often characterized by nodal and extranodal localizations, but a solely gastrointestinal presentation is not uncommon.
12.2.1 Staging
The staging system in childhood NHL is defined according to the Murphy (St. Jude) criteria (Table 12.2) [48]. At this time, it seems to be important to consider that the bone marrow infiltration in NHL is frequent (30–50 %) compared to Hodgkin lymphoma [15, 49]. Moreover considering that NHL aggressive behavior is the most prevalent type found in children, the limited 18F-FDG PET and PET/CT sensitivity in low-grade NHL is not relevant in this age group.
Stage I | A single tumor localization (nodal or extranodal) on one side of the diaphragm with the exclusion of the mediastinum and abdomen |
Stage II | Two or more nodal or extranodal localizations on one side of the diaphragm |
Stage III | With nodal/extranodal involvement of both sides of the diaphragm or primary intrathoracic or intra-abdominal tumors |
Stage IV | Any of the above with initial of the central nervous system, bone marrow, or both |
In this setting 18F-FDG-avidity was reported to be 100 % in Burkitt lymphoma (18/18), 100 % in anaplastic large-cell lymphoma (14/14), 100 % in lymphoblastic lymphoma (6/6), and 97 % in diffuse large B cell lymphoma (216/222) [14]. Overall, PET/CT may show more nodal and extranodal lesions in patients with lymphomas when compared with contrast CT [50] and consequently may change disease stage [22]. London et al. found that PET/CT performed better than conventional imaging in the detection of malignant lesions with significantly improved sensitivity (95.6 % vs. 70.1 %) [12].
In particular 18F-FDG PET seems to be more effective in anaplastic large-cell lymphomas, diffuse large B cell lymphomas, and Burkitt lymphoma when extranodal involvement is frequent [51, 52]. In this field the spleen involvement may be easily recognized by using 18F-FDG PET or PET/CT [53].
However, some physiological tracer uptakes can affect 18F-FDG PET/CT sensitivity at the time of first staging in children. In particular in NHL organs with high physiological uptake such as brain or kidneys might be primarily involved [45]. Moreover, lymphoblastic lymphoma is often associated with diffuse bone marrow infiltration.
Consequently, the differentiation between generalized bone marrow activation from bone marrow infiltration can be sometimes impossible, thus false-positive or false-negative 18F-FDG PET/CT results can be reported [49].
12.2.2 Treatment Response and Follow-Up
In non-Hodgkin entities, tumor masses consist of more than 85 % tumor cells. In contrast to Hodgkin lymphoma, the reduction of the FDG uptake under chemotherapy in non-Hodgkin disease mainly reflects the reduction of the number of living tumor cells [54]. However, because of the limited resolution of PET scanners (about 0.4 cm with modern detector systems), eradication of tumor cells cannot be assumed if 18F-FDG PET is negative during or at the end of treatment [55]. Therefore, evaluation of chemosensitivity early in the course of chemotherapy might be of higher predictive value than at the end of treatment [5].
Children and adolescents with non-Hodgkin lymphoma are usually treated with chemotherapy and without radiotherapy, therefore late effects caused by radiation exposure are not a matter of consideration as they are in Hodgkin lymphoma [5]. However, the risk of inadequate response to chemotherapy might be higher than in Hodgkin lymphoma. The main challenge therefore is to differentiate good responders with a high probability to be cured from poor responders who require treatment intensification.
Reduction of chemotherapy to avoid late effects in very good responders might be relevant in well-defined subpopulations.
On the other hand, considering the data recently reported in NHL adults patients, the positive predictive value (PPV) of interim PET seems to be not very high [56, 57]. Thus, negative 18F-FDG PET/CT scan may predict adequate response, but positive results do not justify treatment intensification.
In this field improvement of response criteria to increase the prognostic value of PET is crucial. Some authors [56] performed additional semiquantitative analyses of interim PET scan, and they found that a reduction of maximum standardized uptake value (Δ SUV max) by >70 % is related to a significantly better progression-free survival and overall survival rates.
More in general, for adults with NHL, results concerning interim 18F-FDG PET are heterogeneous. Negative predictive value (NPV) depends on the histological subtype. It is high in diffuse large B cell lymphoma and therefore suggests excellent prognosis. In contrast, NPV in anaplastic large-cell lymphoma is variable in correlation to ALK status (high in ALK+) [17]. Semiquantitative methods or even biopsy of PET-positive sites seems to improve the PPV of interim 18F-FDG PET in diffuse large B cell lymphoma [57].
Prospective trials are being planned to understand the role of interim 18F-FDG PET in pediatric non-Hodgkin lymphomas. However, some authors [58, 59], investigating a small number of patients, reported high negative predictive value of 18F-FDG PET after two courses of chemotherapy because none of the patients with negative interim 18F-FDG PET relapsed after the end of therapy. On the other hand, it was reported [12] a high specificity level (99.2 %) for 18F-FDG PET/CT as a predictor of poor treatment response in children with non-Hodgkin lymphoma.
However, the role of interim PET/CT in pediatric NHL is not fully clarified. In this field the prognostic role of a negative interim PET and PET/CT has been questioned [19, 60], and more recently Bakhshi et al. [61] did not find any correlation between interim PET/CT findings and outcome in pediatric NHL.
When taking into account the role of 18F-FDG PET at the end of the treatment, a high NPV in patients affected by Burkitt lymphoma was reported [62]. In this field no patient with negative 18F-FDG PET relapsed or turned 18F-FDG PET positive on surveillance. On the contrary when the positive 18F-FDG PET results at the end of treatment have been compared with histopathological findings after biopsy, Riad et al. [63] reported a very low 18F-FDG PET PPV (25 %). Therefore, the authors recommended biopsy if 18F-FDG PET is positive at the end of treatment [5].
12.3 Technical Aspects
12.3.1 Timing of FDG Imaging Related to Chemotherapy
It is suggested that 18F-FDG PET/CT should be performed immediately before the first course of chemotherapy and more in general immediately before a new course [65].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree