Key Facts
- •
Clinical magnetic resonance imaging (MRI) measures the spatial distribution of protons in the body.
- •
Gradient coils are used to provide spatial information. The changing gradients are associated with noise produced during imaging.
- •
Relaxation times T1, T2, and T2* are important tissue characteristics for imaging.
- •
Low-field magnets have lower signal to noise ratio (SNR); longer scan times, making patient motion a potential problem; decreased resolution; decreased sensitivity to old blood and calcified lesions; lower gadolinium enhancement; and difficulty in spectral fat suppression.
- •
Gadolinium contrast medium is often used combined with fat-suppressed T1-weighted imaging to increase contrast between enhanced tissue and surrounding tissue.
- •
Artifacts are numerous in MRI and can lead to erroneous diagnosis if not understood or eliminated. The magic angle phenomenon produces increased signal in portions of tendons oriented at approximately 55 degrees to the main magnetic field. These areas will appear bright on short TE sequences (e.g., T1) and can lead to an erroneous diagnosis of degeneration or tear.
- •
Patient safety is paramount and can be maximized by thorough prescreening and other safety measures.
GENERAL PRINCIPLES
Imaging Principles
Magnetic resonance imaging (MRI) measures the spatial distribution of specific nuclear spins (usually those of protons) in the body. Electric signals from the spins are measured using precessional motion of the proton spins after they are excited by radiofrequency (RF) pulses irradiated in a static magnetic field.
Precession refers to a change in the direction of the axis of a rotating object.
The phenomenon in which the nuclear spins generate or emit electric signals of a specific frequency (Larmor frequency) in a static magnetic field is called nuclear magnetic resonance (NMR).
The electric signal (NMR signal) itself carries no spatial information. The spatial information necessary to generate an image is given by magnetic field gradients that are generated by gradient coils. Because they are driven by pulsed electric currents in a strong magnetic field, the coils receive a repetitive strong force, and a loud sound is produced during the MRI scan.
NMR Signal: Free Induction Decay and Spin Echo
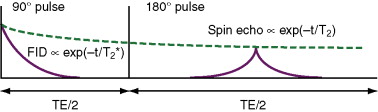
Two kinds of NMR signal are generally used in MRI: free induction decay (FID) and spin echo. FID is elicited by a single RF pulse (e.g., 90 degrees) ( Figure 3-1 ). The FID decays with the time constant T2*. The decay of the NMR signal can be recovered by applying a second RF pulse, called a 180-degree pulse . At a specific time (TE/2) after the second RF pulse, the spin echo signal is observed. The intensity of the spin echo signal decays with the time constant T2.
Relaxation Times
The relaxation times of proton spins are the most important parameters in MRI. Three kinds of relaxation times are generally used: T1, T2, and T2*. T1 or longitudinal relaxation time is the time by which nuclear spins return to thermal equilibrium (initial state) after irradiation by an RF pulse(s). T1 is generally used to visualize the degree of saturation or suppression of NMR signal or image intensity because tissues with longer T1 give suppressed NMR signal in T1-weighted sequences, as described below.
Tissues with long T1 are dark on T1-weighted images.
T2, or transverse relaxation time, describes the lifetime of spin echo signal, as shown in Figure 3-1 . T2 is generally used to distinguish pathologic tissues from normal tissues, because proton spins of pathologic tissues usually have longer T2.
Tissues with a long T2 appear bright on T2-weighted images.
T2* describes the decay rate of FID signal, as shown in Figure 3-1 . Although T1 and T2 depend on NMR frequency (magnetic field strength), typical T1 and T2 values of water content in normal tissues are roughly 1000 ms and 50 ms, respectively. T1 and T2 of pathologic tissues usually become longer than those of normal tissues, making MRI very useful in diagnosis of various diseases.
PULSE SEQUENCES AND IMAGE CONTRAST
The contrast of magnetic resonance (MR) images is determined by combinations of relaxation times and pulse sequences. The pulse sequences are divided into two major categories: spin echo and gradient echo sequences.
Spin Echo Sequence
Spin echo (SE) sequences utilize spin echo signal and produce spin echo images, in which image intensity, I(x,y) , is expressed as:
I ( x , y ) = k ρ ( x , y ) { 1 – exp ( – TR / T1 ( x , y ) ) } exp ( – TE / T 2 ( x , y ) ) ,
| TR << 1000 ms | 1000 ms << TR | |
|---|---|---|
| TE << 50 ms | T1WI | PDWI |
| 50 ms << TE | Not used | T2WI |



Because imaging appearances vary depending on the imaging parameters used, attention should be directed to the parameters listed on the image itself. The TR and TE, among other parameters, are indicated adjacent to the MR image ( Figure 3-3 ).



Table 3-2 explains the appearance of common tissues on SE imaging. The signal may change depending on the combination of the TR, TE, and inversion time (TI) used for obtaining the sequence.
| T1 weighted | T2 weighted | STIR | |
|---|---|---|---|
| Bone cortex, calcification | Very low signal | Very low signal | Very low signal |
| Bone marrow | High signal | High signal | Low signal |
| Cartilage | Iso-signal | Slightly low signal | Iso-signal |
| Joint effusion | Iso-signal | High signal | High signal |
| Acute hemorrhage | Low to iso-signal | Low to iso-signal | Low to iso-signal |
| Subacute hemorrhage | High signal | High signal | Various signal |
| Hemosiderin | Very low signal | Very low signal | Very low signal |
| Fat | High signal | High signal if FSE | Low signal |
In actual clinical settings, SE sequences are usually performed as fast spin echo (FSE) sequences to shorten the imaging time by using multiple spin echoes. Basic image contrasts are similar to those obtained by the traditional or conventional spin echo sequences described above. However, fat tissue is of higher signal on FSE T2-weighted imaging than on spin echo T2-weighted imaging.
Gradient Echo Sequence
Gradient echo (GRE) sequences utilize FID signal and are characterized by sequence parameters TR, TE, and FA (flip angle). The FA is the angle by which nuclear spins are rotated from the direction of the static magnetic field. However, the image contrasts of GRE images are not determined solely by the sequence parameters but are strongly affected by the pulse sequence design.
Regarding the pulse sequence design, GRE sequences are categorized into three groups: incoherent acquisition sequence (e.g., FLASH, SPGR), partially coherent acquisition sequence (e.g., GRASS, FISP), and coherent acquisition sequence (e.g., TrueFISP, SSFP). MRI manufacturers use different names for their own GRE sequences. However, for simplicity, we use the terms FLASH, GRASS, and TrueFISP to represent the three acquisition methods described above. FLASH is mainly used as a T1-weighted sequence. GRASS is used as a T2*-weighted or T1-weighted sequence. FLASH and GRASS are faster than the spin echo T1-weighted sequence, but the image contrasts are slightly different ( Figure 3-4 ). TrueFISP is a very fast sequence and is mainly used for visualization of fluids such as blood.











