Fig. 8.1
Normal fetus at 32 weeks of gestation. (a) Axial SSFP shows upper lip (arrow) and alveolus (arrowheads) without filling defects. (b) Coronal T2WI shows normal palate with hypointense signal (arrow). (c) Sagittal T2WI demonstrates a normal and continuous palate with hypointense signal (arrowheads)
Fig. 8.2
Fetal MRI in a 20-week fetus with unilateral cleft lip and palate. (a) Axial T2WI shows disruption of the lip and alveolus ridge (arrow). (b) Coronal T2WI shows cleft of the lip and palate
Fig. 8.3
Different fetuses at (a) 26 weeks of gestation and (b) at 25 weeks of gestation. (a) Echo planar sequence shows a normal hypointense signal of the palate (arrow). (b) Echo planar sequence shows cleft palate with the absence of normal hypointense signal (arrowhead)
8.3.2 Abnormal Orbits
The analysis of the fetal face by MRI must include the fetal orbits and eyes. Malformations of these structures are often associated with other congenital abnormalities [26]. Congenital eye and orbit abnormalities that can be found on the MRI examination include anophthalmia, microphthalmia, hypertelorism, hypotelorism, and proptosis and exophthalmos.
8.3.2.1 Anophthalmia
Anophthalmia is a rare condition characterized by the absence of the eyeball. It can be unilateral or bilateral. The affected orbit can be absent or, more frequently, hypoplastic (Fig. 8.4). The cause of anophthalmia is the failure of development of the optic vesicle (primary anophthalmia) or the anterior neural tube (secondary anophthalmia). It is usually associated with trisomy 13, triploidy, Klinefelter syndrome, and severe craniofacial abnormalities [27].
Fig. 8.4
Fetal MRI in a 22-week fetus with left anophthalmia. (a) Axial and (b) coronal T2WI show absent left eyeball (arrows)
8.3.2.2 Microphthalmia
In microphthalmia, the eyeball has a smaller diameter than expected for gestational age. It can also be unilateral or bilateral and may be associated with many conditions, including triploidy, trisomy 13, Aicardi syndrome, Walker-Warburg syndrome, and CHARGE (coloboma, heart defects, choanal atresia, retarded growth and development, genital anomalies, and ear anomalies) syndrome [16, 27].
8.3.2.3 Hypertelorism
Hypertelorism is the abnormally increased distance between eyes. It can be recognized when the interocular distance is larger than a single orbit width. Isolated primary hypertelorism is rare; hypertelorism is usually associated with other anomalies such as anterior encephalocele, midline facial masses, craniosynostosis, and chromosomal abnormalities.
8.3.2.4 Hypotelorism
Hypotelorism is the abnormally decreased distance between the eyes resulting in a decreased interocular diameter and binocular diameter (Fig. 8.5). A simple approach to assess for hypotelorism is to make sure the interocular distance is not smaller than a single orbit width. Similar to hypertelorism, hypotelorism is rarely seen as an isolated condition and is often associated with severe malformations in the holoprosencephaly spectrum.
8.3.2.5 Proptosis and Exophthalmos
Proptosis is the forward displacement of the eyeball. The forward displacement of both eye globes is called exophthalmos. These entities usually are associated with craniosynostosis, encephalocele, or rarely, with an orbital mass.
MRI Examination
The visualization of orbital abnormalities using MRI primarily depends on the T2WI axial and coronal views, although T2WI sagittal views can also be useful. No specific sequences for the orbit are regularly used, because the sequences utilized in the brain or craniofacial region are adequate for the assessment of the eyeballs. With T2WI technique, the eyeballs are easily recognized because of their water content as two hyperintense spheres. Distinctive findings in anophthalmia are poorly formed shallow orbits with only rudimentary orbital tissue or a congenital cystic eyeball [28].
The qualitative analysis of the eye size and distance between eyeballs is acceptable for trained radiologists, but in the case of any anomaly of the orofacial anatomy or a midline brain defect, a quantitative measure must be performed to detect minor eye abnormalities. Measurements used for the assessment of the eye size are the anteroposterior ocular distance (APD) and latero-lateral ocular distance (LLD). The APD is measured between the anterior and posterior margins of the eyeballs through the lens, and the LLD is measured between the ethmoidal and malar margins of the eyeballs (Fig. 8.6). The APD and LLD are perpendicular. Measurements used for the detection of hypotelorism and hypertelorism are the interocular distance (IOD) and binocular distance (BOD) (Figs. 8.5 and 8.6). The BOD is measured between the two malar margins of the hyperintense vitreous on the coronal MRI image. Also in coronal T2WI views, the IOD is measured between the two ethmoidal margins of the vitreous. Every measurement obtained must be compared with normative data from fetal MRI according to the gestational age [26]. If the fetus has intrauterine growth restriction, the use of nomogram is not recommended because all eye measurements in these fetuses will be significantly different from normally grown fetuses [26].
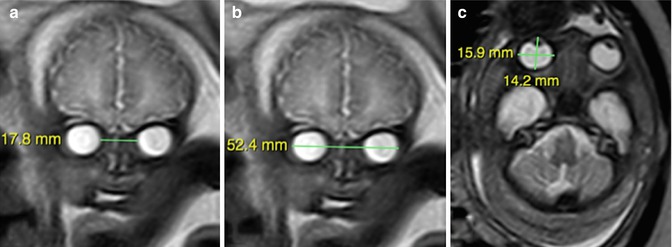
Fig. 8.5
Fetal MRI in a 31-week fetus with semilobar holoprosencephaly and hypotelorism. (a) T2WI shows the absence of the anterior interhemispheric fissure and fusion of the frontal lobes (arrow). (b) The binocular distance measurement (42.7 mm) is below the fifth percentile (44.7 mm). (c) The interocular distance measurement (11.2 mm) is below the fifth percentile (15.8 mm)
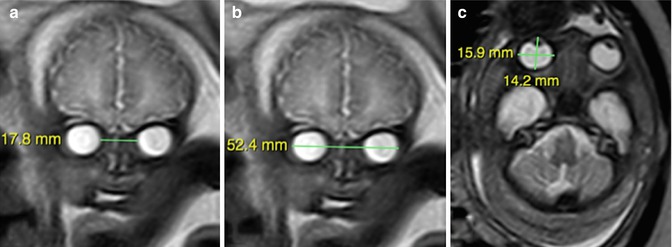
Fig. 8.6
Ocular biometry using T2WI sequence. (a) Measurement of interlocular and (b) binocular distances on coronal view. (c) Measurement of anteroposterior ocular distance (14.2 mm) and latero-lateral ocular distance (15.9 mm) on axial plane
8.3.3 Abnormal Mandible
Mandibular development begins after the sixth gestational week. During embryogenesis, interactions between the ectoderm of the branchial arches and neural crest cells from the dorsal neural tube develop into the mandible [29, 30]. This process is susceptible to genetic insult and environmental factors [31, 32]. Among the environmental causes, neuromuscular conditions such as fetal akinesia deformation sequence can lead to severe micrognathia [30].
8.3.3.1 Micrognathia and Retrognathia
Micrognathia results from hypoplasia of the neural crest cell population. It is rarely isolated and often associated with other abnormalities, such as hemifacial microsomia, Pierre Robin sequence, and Treacher Collins syndrome (see Chap. 6). It may also be part of a syndrome, skeletal dysplasia, or a fetal akinesia deformation sequence. Chromosomal abnormalities have been reported in 66 % of fetuses with micrognathia, usually triploidy, trisomy 13, and trisomy 18 [31, 32].
The terms micrognathia and retrognathia are usually indistinctive in clinical practice. However, micrognathia refers to a small mandible, and retrognathia to an abnormal mandibular position. Micrognathia is often seen in association with retrognathia (receding chin) [30]. In contrast, true retrognathia is rarely found. Distinguishing between these two conditions based on subjective assessment can be difficult. Therefore, objective measurements (inferior facial angle and jaw index) have been developed to assist in differentiating between micrognathia and retrognathia [33, 34].
2D or 3D ultrasound examination of the fetal mandible is important because mandibular anomalies may lead to the diagnosis of major aneuploidy or genetic syndromes. Fetal MRI has proven to be useful for prenatal diagnosis and postnatal surgical management of craniofacial abnormalities and may be used as a complementary method in the assessment of micrognathia and retrognathia [35, 36].
MRI Examination
Sagittal and axial T2WI views are mandatory to the prenatal assessment of the mandible. The sagittal view, specifically, is required for the subjective as well as the quantitative assessment of the position of the mandible. Fetal MRI of the mandible is usually based on subjective evaluation of the facial profile, and micrognathia may be diagnosed by detecting a receding chin. Although diagnosis of micrognathia is usually based on the subjective finding of a receding chin in the of profile view (Fig. 8.7), a recent study showed that subjective evaluation may lead to undiagnosed mandibular conditions in fetuses in which the mandicular recession is not severe [36].
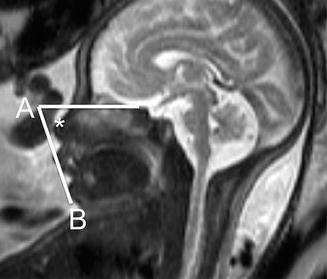
Fig. 8.7
Fetal MRI in a 25-week fetus with severe micrognathia. Sagittal T2WI shows a receding chin easily recognized by subjective assessment. Note associated glossoptosis due to isolated cleft of the soft palate
To quantitatively assess mandibular growth, measurements of the anteroposterior diameter (APD) of the mandible in axial T2WI views are required. Because the APD cannot be directly visualized due to signal superposition of the surrounding anatomic structures, an auxiliary line is draw from the posterior border of the masseter muscle at the mandibular insertion from one side to the other, connecting the presumed mandibular angles. The APD is then measured from the auxiliary line to the symphysis menti (Fig. 8.8). Because in micrognathia the most impaired growth is on the longitudinal plane of the mandibular body, the APD is adequate for assessing the mandibular growth. In addition, transverse growth of the mandible cannot be clearly measured on T2WI because of similar signal intensity of the adjacent structures [36].
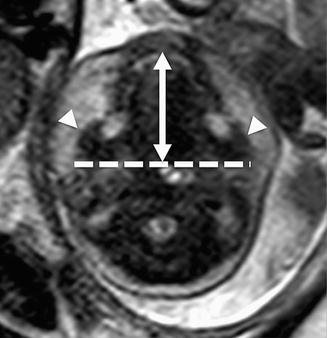
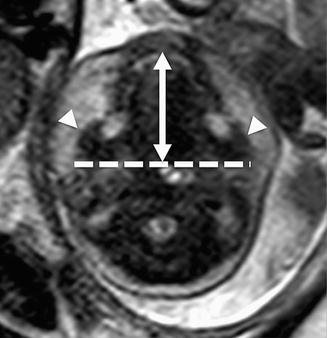
Fig. 8.8
Anteroposterior diameter (APD) on an axial T2WI view. The APD (long double arrow) is measured from the symphysis menti to the line (dotted line) which connects the posterior borders of the masseter muscles (arrowheads)
To assess the mandibular position, the inferior facial angle (IFA), T2WI views are required. IFA is defined as the angle formed between the line perpendicular to the vertical part of the forehead at the level of the nasal root and the line tangential to both the tip of the mentum and the anterior border of the upper lip (Fig. 8.9). The IFA must be performed with either a closed or slightly opened mouth (open lips with a slight fluid in the oral cavity). Fetuses with either micrognathia or retrognathia have an IFA <50° [36]. To differentiate micrognathia from retrognathia, the combined assessment of IFA and jaw index is required. Jaw index is calculated as follows: APD/biparietal diameter ×100 [33]. Micrognathia is diagnosed when the IFA is <50° with a jaw index less than the fifth percentile, whereas retrognathia is diagnosed when the IFA is <50° with a normal jaw index. Although micrognathia defined by IFA <50° is the same whether measured on MRI or ultrasound, different jaw indices based on the two modalities have been reported [36]. On the other hand, IFA by MRI has the same threshold of <50° that defines an abnormal profile by ultrasound.