The utility of MR imaging in evaluating abdominal and pelvic pain in the pregnant patient is discussed. Details regarding the indications, technical aspects, and imaging findings of various common abdominal and pelvic abnormalities in pregnancy are reviewed.
Key points
- •
Evaluating the acute abdomen in pregnancy is complex because of altered physiology and the need to avoid radiation exposure.
- •
MR imaging is a safe and efficacious tool for accurate evaluation of the pregnant patient due to the lack of radiation exposure and its intrinsic high soft-tissue contrast.
- •
Developing dedicated protocols for evaluating the acute abdomen in pregnancy and institutional guidelines on issues including patient informed consent and IV contrast administration is important.
- •
Most acute abdominal and pelvic abnormalities can be diagnosed in a safe and timely manner using MR imaging.
Evaluation of the acute abdomen in a pregnant woman poses special challenges for both the radiologist and the referring physician for several reasons. The most appropriate imaging modality should be selected, balancing the risks of fetal radiation exposure with the potential benefits of establishing a prompt and accurate diagnosis. Imaging protocols vary from institution to institution, with a broad consensus slowly evolving over time. This review discusses the role of MR imaging in evaluating the common nonfetal causes of acute abdominal and pelvic abnormalities in the pregnant woman.
Potential risks of radiation exposure to the fetus
The potential effects of radiation exposure to the fetus have been discussed extensively in the literature. As always, the most important principle in imaging the pregnant patient is that of ALARA (as low as reasonably achievable). The potential clinical benefits must be considered against the potential risk of radiation exposure when selecting the appropriate imaging modality. According to the most recent guidelines from the American College of Radiology (ACR), the risk of radiation-induced deterministic effects are thought to be minimal for exposure less than the 50 mGy threshold (5 rad).
The average radiation exposure of a single abdominal and pelvic computed tomographic (CT) examination performed with current equipment using an appropriate protocol should be much less than the 50-mGy threshold. However, if ionizing radiation can be completely avoided, and diagnostic accuracy can be maintained at a high level, then the use of imaging modalities that do not impart ionizing radiation to the fetus, particularly in the earlier stages of gestation, would be preferable.
Potential risks of radiation exposure to the fetus
The potential effects of radiation exposure to the fetus have been discussed extensively in the literature. As always, the most important principle in imaging the pregnant patient is that of ALARA (as low as reasonably achievable). The potential clinical benefits must be considered against the potential risk of radiation exposure when selecting the appropriate imaging modality. According to the most recent guidelines from the American College of Radiology (ACR), the risk of radiation-induced deterministic effects are thought to be minimal for exposure less than the 50 mGy threshold (5 rad).
The average radiation exposure of a single abdominal and pelvic computed tomographic (CT) examination performed with current equipment using an appropriate protocol should be much less than the 50-mGy threshold. However, if ionizing radiation can be completely avoided, and diagnostic accuracy can be maintained at a high level, then the use of imaging modalities that do not impart ionizing radiation to the fetus, particularly in the earlier stages of gestation, would be preferable.
Safety of MR imaging in pregnancy
Because of the absence of exposure to ionizing radiation, its multiplanar imaging capabilities, and excellent imaging quality and soft-issue contrast, MR imaging has been shown to be an excellent option for imaging the pregnant patient with acute abdominal and pelvic disorders. The primary concerns for fetal exposure to MR imaging are the heating effects of the radiofrequency pulses and the effects of acoustic noise on the fetus. Higher strengths of the magnetic field, use of a higher flip angle, an increased number of radiofrequency pulses, and decreased spacing between them, are all associated with a higher specific absorption rate, leading to potentially higher fetal tissue heating. Sequences including single-shot fast spin-echo (SSFSE) are single acquisition echo-train spin-echo sequences and use 180° refocusing pulses. They are associated with higher fetal heating than gradient-echo sequences, which do not use the refocusing pulse. Tissue heating is however maximum at the maternal body surface and decreases near the center of the body, making fetal thermal damage less likely. To the authors’ knowledge, there is no evidence of adverse fetal heating with a 1.5-T or lower field strength magnet. Similarly, exposure to acoustic noise has not been proven to adversely affect fetal hearing, because the noise gets attenuated while traveling through the amniotic fluid and gets delivered to the fetus at less than 30 dB.
A few animal studies have raised the possibility of adverse effects of noncontrast MR imaging (ranging from 0.35 T to 1.5 T) on mice and chick embryos, whereas another study (4.7-T strength) found no significant adverse effects. The duration of exposure of the embryos to MR imaging in these studies ranged from 6 to 48 hours, which does not parallel the situation in clinical practice. The applicability of these findings to the human embryo is somewhat controversial. Overall, MR imaging has been used safely for imaging obstetric patients for more than the past 2 decades, without any documented adverse fetal effects. The International Commission on Non-Ionizing Radiation Protection, in its statement on MR imaging in pregnancy, published in 2004 and updated in 2009, stated that “there is no clear evidence that exposure to static or low frequency magnetic fields can adversely affect pregnancy outcome,” but concluded that the overall evidence to provide unequivocal guidelines is insufficient. It recommended that MR imaging should be performed in pregnancy only after a critical risk-benefit analysis, particularly in the first trimester, and that imaging time should be minimized. The ACR guidelines on imaging patients in pregnancy do not recommend any special consideration for first trimester MR imaging, given the absence of documented adverse effects.
According to the ACR guidelines, MR imaging can be performed in any stage of pregnancy if, in the medical opinion of a level 2 MR imaging personnel-designated attending radiologist, the examination is indicated after considering the risk-benefit ratio. The following should be documented in the radiology report or in the patient’s medical records after conferring with the referring physician:
- i.
The information was not/cannot be obtained by using ultrasound (US);
- ii.
The information obtained from the examination will potentially directly benefit maternal or fetal care during the pregnancy;
- iii.
The referring physician does not think it is wise to wait until after the patient delivers to obtain the MR imaging.
Safety of intravenous gadolinium in pregnancy
Intravenous (IV) gadolinium in pregnancy is considered a category C drug, with teratogenic effects having been demonstrated in animals without any definite effects on human fetuses. Because IV gadolinium crosses the placenta and remains in the amniotic fluid indefinitely, being recycled by the fetal kidneys, there is a theoretic risk of free gadolinium ions dissociating from the chelate and having an adverse effect on fetal development. According to the ACR guidelines for imaging pregnant patients, IV gadolinium should not be routinely used in pregnancy. Any decision to administer IV gadolinium in pregnancy should be made only after carefully balancing the risk and potential benefit and should be considered only in very select situations. The authors’ practices almost never perform IV contrast-enhanced MR imaging in pregnant patients, cautiously using it only when absolutely necessary for the diagnosis, as in staging of malignancies, for example. Whenever unavoidable, a decision to administer IV gadolinium should be made only after close consultation with the referring physician(s) and with the patient. The ACR recommends obtaining written informed consent from pregnant patients before an MRI examination.
Status of academic radiology practices in abdominal imaging of pregnant patients
In a survey of 85 academic abdominal imaging divisions across the United States published in 2007, 74% had a written departmental policy regarding the use of MR imaging in pregnancy. Over 90% of respondents performed CT and MR imaging in pregnancy, depending on the patient’s needs. CT was preferred over MR imaging in the setting of trauma in all 3 trimesters, and for evaluating suspected appendicitis, abscess, or renal calculus in the second and third trimesters. MR imaging was preferred over CT for diagnosing appendicitis and abscess in the first trimester. A more recent albeit smaller survey of 45 radiologists on the same topic also included nonacademic radiologists in it (48% in academic practice, 19% in community hospitals having residents, and the rest in nonspecialty/subspecialty private practice). Forty-three percent of the respondents had a written policy on imaging in pregnancy, and 72% had dedicated low-radiation-dose CT protocols for imaging pregnant patients. Forty-eight percent preferred noncontrast CT, whereas 45% preferred MR imaging to evaluate suspected renal calculi after an indeterminate US examination. No specific questions were asked on appendicitis, but MR imaging was preferred over CT in evaluating generalized abdominal pain and suspected inflammatory bowel disease (IBD). The authors currently consider MR imaging to be an invaluable tool for evaluating abdominal pain in pregnancy and think that it should be the preferred modality along with US in all settings except trauma, where CT has substantial operational advantages.
MR imaging protocol
Many practices have dedicated MR protocols for imaging the abdomen and pelvis in pregnancy, using sequences that minimize motion artifacts due to respiration, peristalsis, and fetal movements. At the authors’ institutions, they use single-shot fast-spin echo (SSFSE/HASTE [half-Fourier acquisition single-shot turbo-spin echo]) and T2-weighted (T2W) fat-saturated sequences in all three planes, along with axial gradient-echo T1-weighted in-phase and out-of-phase sequences in all patients ( Table 1 ). A large field of view is generally used, but focused smaller field-of-view images can be obtained if necessary. Typically, the examination time is optimized and kept to a minimum. A 2009 study demonstrated MR imaging without oral contrast to be efficacious for diagnosis of the causes of acute pelvic pain in both pregnant and nonpregnant women, which is consistent with the authors’ own experience. Oral contrast is not given before the MR imaging in the authors’ practices.
| Plane | Sequence | Breath-Hold | TR (ms) | TE (ms) | Slice Thickness (mm) | Slice Spacing | SAR | b-value |
|---|---|---|---|---|---|---|---|---|
| Ax/Cor (large FOV) | SSFSE | Yes | 580 | 90 | 5 | 6 | 3 | — |
| Ax/Cor/Sag (focused) | SSFSE | Yes | 577 | 91 | 4–5 | 5.5 | 2 | — |
| Ax/Cor/Sag | SSFSE FS | Yes | 550 | 90 | 5 | 6 | 2 | — |
| Ax | In- and out-of-phase | Yes | 4.6/2.3 | 119 | 7 | 8 | 1.9 | — |
| Ax/Cor | DWI/ADC (sos) | Yes | 6283 | 64 | 6 | 7 | 0.9 | 0, 400, 800 |
| Ax/Cor/Sag | Pre- and post-contrast T1FS (sos) | Yes | 4.4 | 2.2 | 4.4 | 2.2 | 0.4 | — |
General principles of imaging pregnant patients with abdominal and pelvic pain
Evaluation of abdominal pain during pregnancy is more challenging because of multiple reasons. Physiologic changes during pregnancy can mimic various abnormalities and create diagnostic uncertainty (as, for example, nausea and vomiting in early pregnancy). Furthermore, the uterus usually becomes an abdominal organ after 12 weeks, making it difficult to localize pain on physical examination and concealing or delaying various clinical signs and symptoms, making the role of imaging critical for prompt and accurate diagnosis. The most important role of imaging is to differentiate between an urgent surgical and nonsurgical condition. Initial imaging of suspected obstetric causes of abdominal or pelvic pain is usually performed with sonography. US is also usually the first imaging examination performed for evaluating suspected nonobstetric causes of acute abdominal or pelvic pain, with MR imaging increasingly performed as a second-line imaging examination when the sonographic examinations are equivocal or nondiagnostic (which is frequently the case in pregnancy). Many studies in the literature have shown that MR imaging is useful for the diagnosis of pregnant patients presenting with abdominal pain. A study of 118 pregnant patients (mean gestational age 20.6 weeks) presenting with acute abdominal or pelvic pain found MR imaging to have a sensitivity, specificity, positive predictive value, and negative predictive value for diagnoses requiring surgery or an interventional radiology procedure of 89%, 95%, 76%, and 98%, respectively.
The most common causes of abdominal pain in pregnancy are listed in Table 2 . In this article, the authors discuss the role of MR imaging in evaluating the most common entities presenting with an acute abdominal and/or pelvic condition in pregnancy.
| Site | Preferred Imaging Modalities for Diagnosis |
|---|---|
| Upper abdominal pain | |
| Gallbladder disease | US > MR imaging |
| Hepatitis | US > MR imaging |
| Pancreatitis | US/MR imaging > CT |
| Bowel obstruction | US/MR imaging > CT |
| Perforated ulcer | Abdominal radiographs > CT |
| Lower abdominal pain | |
| Appendicitis | US > MR imaging > CT |
| Nephrolithiasis | US > MR imaging/CT |
| Inflammatory bowel disease | MR imaging > CT |
| Gynecologic causes (ovarian torsion, complicated adnexal cysts, degenerating fibroid, pelvic inflammatory disease) | US > MR imaging |
| Diverticulitis | MR imaging > CT |
| Trauma | US > CT (MR imaging may be used in follow-up imaging) |
| Oncologic causes | CT/MR imaging |
Appendicitis
Acute appendicitis is the most common nonobstetric surgical cause of abdominal pain during pregnancy. The incidence is estimated at 1 in 800 to 1 in 1700 pregnancies. The clinical diagnosis of appendicitis in pregnancy is based on the classic triad of right lower quadrant pain, fever, and leukocytosis. Acute appendicitis is relatively difficult to diagnose during pregnancy for several reasons. The gravid uterus can mask underlying tenderness. The appendix is also often displaced from the right lower quadrant in the third trimester, and mild leukocytosis can frequently be physiologic during pregnancy. Furthermore, appendicitis is more morbid during pregnancy because there is a higher rate of perforation and associated complications, which can also result in premature labor, fetal morbidity, and mortality. Pregnancy-related complications are higher in pregnant women with perforated appendicitis compared with those with nonperforated appendicitis. A retrospective review of 778 pregnancies requiring appendectomy found an increased rate of preterm delivery, low birth weight, still births, and neonatal mortality. Another study of 3133 pregnant patients who underwent appendectomy found both complicated appendicitis and negative appendectomy to be associated with a significantly higher rate of fetal demise. Thus, risk of delay in diagnosis must be balanced against the risk of negative laparotomy, making appropriate and timely imaging extremely important.
Role of Ultrasound
Graded-compression US is the preferred initial imaging modality for evaluating patients with suspected appendicitis as per the ACR Appropriateness Criteria due to its safety, availability, and low cost, although it has major limitations, particularly in the later stages of pregnancy. In addition, US is also helpful for the identification of alternate diagnoses, although the accuracy is less than that for MR imaging or CT. The imaging criteria for appendicitis are the same as in nonpregnant patients. These imaging criteria include a dilated (>6 mm) thickened, tubular blind-ending, noncompressible structure, associated with inflammation of the adjacent fat. Associated appendicoliths may be identified.
However, the limitations of US include its operator-dependence, inconsistent visualization of the appendix due to overlying bowel gas and the overlying uterus, and variability with patient body habitus and advanced gestational age, among other reasons, explaining the relatively poor sensitivity and specificity reported in the more recent literature for US for appendicitis in pregnancy. An early study of 42 patients, published in 1992, found US to be 100% sensitive and 96% specific in the diagnosis of appendicitis in pregnancy. However, these results were in Asian women in the earlier stages of gestation, and multiple more recent studies have reported a much lower sensitivity, ranging from 20% to 36%.
Role of MR Imaging
MR imaging is the preferred second-line imaging modality in indeterminate cases of appendicitis, as per the ACR Appropriateness Criteria. Multiple recent studies have shown MR imaging to have a higher sensitivity and specificity for the diagnosis compared with US, besides simultaneously evaluating other potential causes of pain. A meta-analysis of 6 studies described the pooled sensitivity, specificity, and positive and negative predictive values to be 0.91 (95% confidence interval [CI], 0.54–0.99), 0.98 (95% CI, 0.87–0.99), 0.86 (95% CI, 0.38–0.98), and 0.99 (95% CI, 0.93–0.99), respectively.
Protocol
SSFSE sequences in all 3 planes are the most useful for identifying the appendix, particularly the coronal and right lower quadrant sagittal planes. Fat suppression is helpful to increase the conspicuity of inflammatory changes. A few publications have advocated using negative oral contrast to increase diagnostic confidence, giving 300 to 450 mL of oral iron oxides combined with 300 mL of barium sulfate 1 to 1.5 hours before the MR examination. However, multiple other reports have noted similar sensitivity and specificity without administering oral contrast. The authors’ practices do not give oral contrast. Two additional sequences may be used for the MR imaging appendicitis protocol. Adjacent vessels, particularly the gonadal vein and its tributaries, can mimic the appendix on SSFSE images, especially in the later stages of gestation. A transverse 2-dimensional time-of-flight (TOF) gradient-echo sequence can be used to differentiate between the two. Diffusion-weighted imaging (DWI) sequences are not universally used, but can be potentially useful to improve conspicuity. A recent study of 117 pregnant patients with clinically suspected acute appendicitis (compared with 50 control patients) found DWI to increase the conspicuity of the inflamed appendix. Quantitative evaluation of the DW signal intensity and apparent diffusion coefficient (ADC) values revealed a significant difference between the normal and inflamed appendix ( P <.001), with the best discriminatory parameter being the signal intensity ratio on b = 500 value. However, more studies are needed to validate this and compare its utility beyond fat-suppressed T2W images.
Normal appearance of the appendix on MR imaging
The normal appendix appears as a tubular, blind-ending structure arising from the cecum, containing air or oral contrast (if administered). Oral contrast causes blooming on the in-phase and TOF images, also helping to differentiate the appendix from vessels. The normal appendix is 6 mm or less in diameter.
MR imaging features of appendicitis
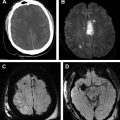
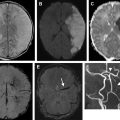
The characteristic MR imaging appearance of acute appendicitis is a fluid-filled appendix, measuring 7 mm or greater in diameter, with associated periappendiceal inflammation ( Figs. 1 and 2 ). Other MR imaging findings include appendiceal wall thickness greater than 2 mm, T2 hyperintense appearance of the appendiceal lumen due to fluid or edema, and the absence of blooming. Periappendiceal fat stranding and fluid are often best appreciated on the fat-suppressed sequence. An appendicolith (or appendicoliths) may also be seen and appears hypointense on all sequences. An associated phlegmon may be visualized as a heterogeneous T2 intermediate to hyperintense mass. Associated abscess formation would appear as a well-defined T2 hyperintense fluid collection. An air pocket within the abscess would demonstrate blooming on the in-phase and TOF images.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree