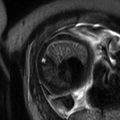
Fig. 18.1
Routine non-contrast MR sequences in the evaluation of abdominal and pelvic pain in the pregnant patient. Example of axial T2-weighted single-shot echo train spin echo image (a) demonstrates a uterine fibroid with mildly increased T2-weighted signal and surrounding fluid suggestive of degeneration (arrow). Example of T2-/T1-weighted steady-state free precession image in a different patient (b). T1-weighted dual-echo gradient-recalled echo images in-phase (c) and opposed phase (d) in a third patient demonstrate a large dermoid (straight arrows) with evidence of internal fat (curved arrow). The lesion did not show evidence of torsion by imaging
Fig. 18.2
Optional non-contrast MR sequences. Examples of axial T2-weighted image with fat suppression showing normal ovaries (a), T1-weighted GRE image with fat suppression in a patient with endometriosis (b), T2-weighted image with oblique angle in a patient with uterine anomaly (c), T2-weighted image with high resolution in a patient with cervical carcinoma diagnosed during pregnancy (d), diffusion-weighted image in a patient with uterine duplication and obstructing vaginal septum (e), and thin-slice 3D heavily T2-weighted image from MR urography in a patient with physiologic hydronephrosis of pregnancy (f)
During the first trimester, extrauterine pelvic anatomy is not yet significantly altered and resembles that of the nonpregnant female. The uterus maintains its version and flexion, typically anterior and best demonstrated on sagittal images. The bladder lies anterior and inferior to the uterus, and the vagina is posterior to the bladder and urethra. The rectum and anus lie posterior to the vagina. Typical location of the ovaries is lateral to the midline uterus, and ovaries are typically easily recognized secondary to high signal intensity of the ovarian follicles on T2-weighted imaging. During the second and third trimesters, the uterus becomes an intra-abdominal organ due to increase in size and displaces many pelvic contents from their normal location. The appendix is often displaced superiorly as are the adnexal structures.
18.2 Causes of Acute Abdominal and Pelvic Pain in Pregnancy
18.2.1 Gastrointestinal
18.2.1.1 Acute Appendicitis
Acute appendicitis is the most common non-obstetric surgical condition in pregnancy [4, 5]. Early and accurate diagnosis is of paramount importance because of increased fetal loss rate of 30 % seen with appendiceal rupture compared to <2 % fetal loss rate in the absence of rupture [6]. The clinical diagnosis of appendicitis can be difficult due to atypical location of pain secondary to cephalad migration of the cecum and appendix by the gravid uterus [2], as well as physiologic leukocytosis observed during pregnancy. MRI can be useful to exclude appendicitis if a normal appendix is visualized (Fig. 18.3). MRI has been shown to be superior in the visualization of the normal appendix compared to ultrasound [7], and the appendix can be visualized with high accuracy in the pregnant patient, estimated at 83–91 % [8–10]. In the acute setting, MRI shows good diagnostic accuracy of appendicitis with sensitivity of 80–100 % and specificity of 93.6–100 % [7, 9].
Fig. 18.3
Normal appendix. Axial T1-weighted (a), axial T2-weighted with fat saturation (b), and coronal T2-weighted (c) MR images demonstrate a nondilated appendix with no adjacent inflammation (curved arrows)
The MR imaging findings of acute appendicitis are similar to that of the nonpregnant patient. T2-weighted imaging demonstrates a dilated appendix and mural thickening (Fig. 18.4). Periappendiceal fluid can be seen as high signal intensity on T2-weighted images and may be more readily visualized utilizing fat suppression techniques. Periappendiceal abscess can be seen in the setting of a ruptured appendix (Fig. 18.5). Contrast is rarely needed for diagnosis; however, if contrast is administered, the appendix would demonstrate mural enhancement.
Fig. 18.4
Acute uncomplicated appendicitis. Axial T2 weighted (a) and T2 weighted with fat saturation (b) MR images demonstrate a dilated, thick-walled appendix with adjacent fat stranding and inflammation (curved arrows). Coronal T2-weighted image in a different patient (c) reveals similar findings of a dilated fluid-filled appendix with mild periappendiceal inflammation (arrow)
Fig. 18.5
Appendicitis with rupture and abscess. Axial T1-weighted (a, b) and T2-weighted (c, d) images show a heterogeneous mass in the right lower quadrant with adjacent inflammation compatible with perforated appendicitis and surrounding mass (arrows, a, c). Notice the small hypointense structure in the center of the inflammation (arrows, b, d) consistent with a small appendicolith
18.2.1.2 Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) has a peak age distribution similar to that of childbearing age in the female, with peak incidence at 15–25 years [11]. IBD is a common mimicker of appendicitis in that the terminal ileum is involved in approximately 80 % of patients with IBD [11, 12]. Patients will typically present with diffuse abdominal pain, diarrhea, nausea, and vomiting. The colon can be involved with associated involvement of the small intestine in approximately 50 % of cases and in isolation in about 15–20 % of cases [11]. MR is accurate in the evaluation of IBD and its complications including abscess, fistula, and strictures [11, 12].
18.2.1.3 Bowel Obstruction
The majority of bowel obstructions during pregnancy are secondary to adhesions, estimated at up to 58 % [15]. Additional causes include volvulus, intussusception, and inflammatory bowel disease. Imaging features consist of dilated fluid-filled bowel loops of small and/or large bowel. Small bowel is considered dilated when measured greater than 2.5 cm in diameter [16] and large bowel when measured greater than 6 cm or greater than 9 cm at the cecum [17]. Bowel obstruction is best depicted utilizing HASTE/SSFSE or FISP/FIESTA images (Fig. 18.6).
Fig. 18.6
Small bowel obstruction. Coronal T2-weighted images (a, b) reveal dilated loops of small bowel within the right lower quadrant of the abdomen (curved arrow, a) with decompression to more normal caliber small bowel in the right lower quadrant (curved arrow, b)
18.2.1.4 Abdominal Wall Hernia
The presence of an enlarged, gravid uterus and displacement of intra-abdominal structures can cause small bowel or omentum to protrude through an existing or acquired ventral or umbilical hernia. This can lead to bowel obstruction or omental ischemia and pain from incarceration (Fig. 18.7). Signs suggestive of incarceration include fluid within the hernia sac, wall thickening of herniated bowel loops, and dilatation of bowel proximal to the hernia [18].
Fig. 18.7
Incarcerated umbilical hernia. Axial T1-weighted (a) and T2-weighted with fat saturation images show a small fat-containing umbilical hernia with surrounding inflammation (arrow, a, b)
18.2.2 Hepatobiliary
18.2.2.1 Acute Cholecystitis
Acute cholecystitis is the second most common condition necessitating surgery during pregnancy [12]. Ninety percent of cases of acute cholecystitis during pregnancy are secondary to gallstones [15]. Pregnancy is a known risk factor for cholelithiasis as the pregnant state leads to increased cholesterol synthesis by estrogen and decreased gallbladder motility by progesterone [19]. Ultrasound is the primary method for diagnosis, but MR boasts relatively high sensitivity of 88 % and specificity of 89 % [15]. Imaging findings include gallbladder wall thickening and edema with pericholecystic fluid, best demonstrated as high signal intensity on T2-weighted images. While these findings are readily diagnosed on ultrasound, it can be very difficult to image choledocolithiasis with ultrasound alone. MRCP can detect stones within the biliary tree with a sensitivity of 89–100 % and specificity of 83–100 % [20]. Choledocolithiasis is depicted as a low signal intensity filling defect on T2-weighted/MRCP images with upstream dilatation above the site of the filling defect [20] (Fig. 18.8). One must be careful not to mistake flow artifact, which is seen as an intermediate signal intensity, centrally located filling defect on a single sequence, for a choledocolith [21]. MRCP can also limit the performance of unnecessary ERCP when no stones are visualized in the biliary system.
Fig. 18.8




Choledocolithiasis. Heavily T2-weighted coronal MRCP images demonstrate numerous hypointense gallstones in the gallbladder (arrowhead, a) and several small filling defects within the dilated cystic duct compatible with small stones (arrow, a). Additional MRCP image reveals numerous fillings defects within the dilated extrahepatic common duct compatible with choledocolithiasis (arrow, b)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree