Magnetic Resonance Imaging of Ischemic Heart Disease
Charles B. Higgins
Karen Ordovas
Stefano Muzzarelli
The evaluation of ischemic heart disease (IHD) by noninvasive imaging techniques has usually involved nuclear imaging and echocardiography for initial diagnosis, monitoring, and assessment of severity. Coronary angiography has been employed for precise definition of coronary arterial stenoses and to guide therapeutic interventions. In the first two decades of cardiovascular magnetic resonance imaging (MRI), its application in IHD was meager. With the introduction of MR imagers adapted for cardiovascular imaging, however, the capability for the comprehensive evaluation of IHD has been demonstrated.
The comprehensive evaluation of IHD requires the following steps:
Detect and assess the severity of IHD
Define the coronary anatomy
Evaluate and monitor myocardial revascularization
Determine myocardial viability
Demonstrate complications of myocardial infarction
The role of MRI in accomplishing each of these tasks will be addressed. The evaluation of IHD by MRI remains technically complex because of the multitude of acquisition sequences used to accomplish a comprehensive evaluation. The various sequences will be described briefly in relation to the specific tasks.
DETECTION OF ISCHEMIC HEART DISEASE
The detection of IHD using noninvasive imaging employs two approaches: stress function and stress perfusion. Stress function is the major technique applied with echocardiography. Stress perfusion is the technique used with nuclear scintigraphy. It is generally felt that stress function has greater sensitivity and stress perfusion has better specificity. MRI uses both techniques for detecting and assessing the severity and extent of myocardial ischemia. The site of myocardial ischemia is assigned to a major coronary artery using the American Heart Association 17 segment model (Fig. 37-1). The 17 segments are evaluated by acquiring functional or perfusion images in multiple short-axis planes and the vertical long-axis planes. The apical segment (segment 17) of the left ventricle (LV) is assessed in the vertical long axis plane while the other 16 segments are inspected in three short-axis planes.
STRESS FUNCTION
Pharmacologic stress is employed to induce a regional contraction abnormality as a functional indicator of a hemodynamically significant coronary arterial stenosis. This is the method used to identify IHD by echocardiography. The pharmacologic stressor is usually an infusion of dobutamine. The dose is gradually increased to stimulate intermediate stress (20 μg/kg/min) and then peak stress (40 μg/kg/min). The maximum level of stress should achieve a heart rate equal to 85% of the maximum heart rate predicted for age. Atropine can be administered to achieve this heart rate.
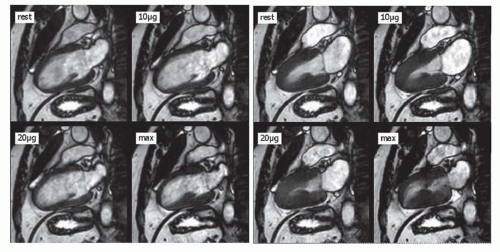
Cine MRI is performed in the short-axis plane at multiple levels and vertical long-axis planes in the baseline state, at intermediate stress, and at peak stress using a balanced steady-state free precession sequence (variably named by the manufacturers as balanced fast field echo [balanced FFE], true fast imaging with steady precession [FISP], or fast imaging employing steady-state acquisition [FIESTA]). With these sequences, cine MR images consisting of 16 to 40 phases can be acquired at three anatomic locations in a breath-hold of 10 to 20 seconds (Fig. 37-2).
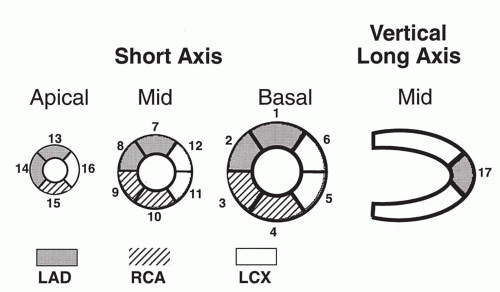 FIG 37.1. Seventeen-segment model suggested by the American Heart Association. The coronary artery territories are shown in the graph. |
 FIG 37.2. End-diastolic (top) and end-systolic (bottom) cine MR images in the short axis extending from apex (left) to base (right) of the ventricles. |
Left ventricular dysfunction during stress is indicated by a segmental decrease in wall thickening, wall motion, or both (Fig. 37-3). The sensitivity and specificity for detecting a hemodynamically significant stenosis (greater than 50% reduction in luminal diameter) of the coronary artery subserving the dysfunctional segment are about 85%. This level of diagnostic accuracy is equivalent to stress echocardiography.
The rationale for stress function to identify a hemodynamically significant coronary arterial stenosis is that patients with such lesions have adequate blood flow in the resting (basal) state. However, when pharmacologic stress is applied flow may increase three- to fivefold in a normal artery. In the stenotic artery flow cannot increase to the appropriate level so regional myocardial contractile dysfunction is induced. Dobutamine is a secondary coronary vasodilator in that flow is stimulated by the beta sympathomimetic stimulation of myocardial contractility and heart rate; these effects increase myocardial oxygen consumption (demand) and consequently the need for increased coronary blood flow. Failure of coronary flow to rise to the appropriate demand is reflected in a regional contraction abnormality (decreased or no wall thickening or motion). Since myocardial ischemia is provoked by this test, careful patient monitoring is essential during this test (see Selected Reading for extensive discussion of the performance; safety precautions; and contraindications for this test).
Another approach for stress function is to administer a primary vasodilator such as dipyridmole or adenosine which increases coronary flow by directly dilating coronary arterioles (resistance vessels). In the presence of a hemodynamically significant stenosis, resistance vessels in the myocardium served by the coronary artery (conductance vessel) are already maximally dilated. Consequently, the primary vasodilator only increases flow to myocardium served by nonstenotic arteries and flow is stolen from the stenotic region inducing regional myocardial ischemia (coronary arterial steal). Dobutamine stress is superior to adenosine stress for inducing wall motion abnormalities.
Some studies have shown greater sensitivity, specificity, and diagnostic accuracy of dobutamine stress function MR compared to dobutamine stress echocardiography. Moreover, most patients with nondiagnostic dobutamine echocardiography had diagnostic stress MR studies. The provocation of regional myocardial dysfunction by dobutamine stress MR has been found to identify patients at risk of myocardial infarction and death.
STRESS PERFUSION
Pharmacologic stress is used to provoke a perfusion deficit in the myocardium supplied by a coronary artery with a hemodynamically significant stenosis. The pharmacologic agents used are dipyridamole and adenosine (primary vasodilators as described above). MR images are acquired
in the short-axis plane at three to five anatomic levels and at one vertical long-axis plane during the first passage of intravenously injected gadolinium chelate (0.03 to 0.05 mmol/kg). A saturation recovery or inversion recovery fast gradient-echo sequence is used to diminish the signal of myocardium before the arrival of the contrast. The images at each anatomic level are acquired at a rate of about 1 per second for about 30 seconds. A regional perfusion deficit is usually visible (Figs. 37-4 and 37-5). The defect may be subendocardial or nearly transmural. Quantitative analysis of the regional intensity-time curve during initial passage of the contrast can improve the diagnostic accuracy. The prime discriminatory parameter is the maximum upslope of the curve.
in the short-axis plane at three to five anatomic levels and at one vertical long-axis plane during the first passage of intravenously injected gadolinium chelate (0.03 to 0.05 mmol/kg). A saturation recovery or inversion recovery fast gradient-echo sequence is used to diminish the signal of myocardium before the arrival of the contrast. The images at each anatomic level are acquired at a rate of about 1 per second for about 30 seconds. A regional perfusion deficit is usually visible (Figs. 37-4 and 37-5). The defect may be subendocardial or nearly transmural. Quantitative analysis of the regional intensity-time curve during initial passage of the contrast can improve the diagnostic accuracy. The prime discriminatory parameter is the maximum upslope of the curve.
The sensitivity and specificity for identifying a hemodynamically significant stenosis are about 85%. The diagnostic accuracy of MR perfusion imaging has been found to be equal or better than single photon emission tomography and positron emission tomography. An expected advantage of MR perfusion imaging is greater sensitivity in detecting small subendocardial perfusion deficits (Fig. 37-5) and for demonstrating triple-vessel disease with diffuse myocardial ischemia (Fig. 37-6).
There are now both single center and multicenter studies comparing MR perfusion and radionuclide perfusion imaging. Receiver Operating Characteristic (ROC) curve analyses of sensitivity and specificity (Fig. 37-7) have shown better performance for MR perfusion in both single center and multicenter trials (see Selected Reading for details of these studies).
CORONARY FLOW RESERVE
Velocity-encoded (VEC; phase contrast) cine MR can be used to measure the flow velocity and flow volume of individual major coronary arteries. This is usually done using a breath-hold version of this sequence. This sequence provides a pair of images at approximately 12 to 16 phases of the cardiac cycle. The pair consists of magnitude and phase images acquired perpendicular to the direction of blood flow (Fig. 37-8). A set of images is acquired in the basal state and in the vasodilated state induced by dipyridamole or adenosine. From these images, peak velocity of flow can be calculated in each state (see Fig. 37-8). Coronary flow reserve is the ratio of maximal flow to basal flow. A normal value is designated as a ratio greater than 2.3 to 2.5. In the presence of a hemodynamically significant stenosis (more than 50% reduction in luminal diameter), it is lower than 2.3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree