Fig. 24.1
Pubic osteitis in a 32-year-old woman at 20 weeks of gestational age, with recurrent pubic pain. Coronal (a) and axial STIR (b) and coronal (c) and axial (d) T1-weighted MRI images show sclerosis of the subchondral bone at the level of the pubic symphysis (arrows) with small subchondral erosions, finding typical of pubic instability
Fig. 24.2
Pubic osteomyelitis in a 35-year-old woman presents with pubic pain, fever, and elevated inflammatory markers. Sagittal (a), coronal (b), and axial (c) T2-weighted HASTE images, and axial STIR images (d) show fluid collection (arrows) at the level of the symphysis pubic bone with hyperintensity of the pubic bone (short arrows). DWI image (e) shows the presence of restriction of diffusion within the fluid collection, which is indicative of an abscess (arrows). These findings are in agreement with osteomyelitis
Fig. 24.3
Pubic chondrosarcoma in a 30-year-old woman at 34 weeks of gestational age, with recurrent pubic pain. (a) Coronal STIR image demonstrates soft tissue mass (arrow) with erosion of the right pubic bone and pericortical extension. Note lobular growth and deep endosteal scalloping. (b) Coronal T1-weighted sequence shows bone destruction and cortical penetration (arrow). A chondrosarcoma was found at biopsy and confirmed at pathology after the delivery
24.2.1 Low Back Pain, Disk Disease, and Sciatica
Low back pain is one of the most common complain during pregnancy and postpartum period, affecting more than 50 % of woman during pregnancy [27, 28]. It is characterized by lumbar region pain, exacerbated in forward flexion, with a restriction of spine movement and painful palpation of the erector spinae muscle [4, 19, 29].
Several factors contribute to pain during pregnancy, including lumbar lordosis, direct pressure from the gravid uterus, and ligamentous laxity due to relaxin hormone.
Overload on the spine is due to increased body weight, anterior displacement of the body’s center of gravity, and loss of the normal abdominal muscle tone that normally acts as a spine stabilizer [19, 20].
True sciatica is rare affecting less than 1 % of women [28]. Clinical diagnosis is easy and MRI is to be reserved in case of uncontrolled symptoms, especially if related to spinal canal stenosis or strength and motor deficiency [1].
Disk herniation causing radiculopathy occurs in 1/10,000 pregnancies; in these cases L5 or S1 root is commonly affected by lateral compression, while large central herniation can cause cauda equina syndrome [27, 28]. Disk herniation is the most common cause of sciatica, but a rare cause could be compression of lumbar nerves from epidural varices [28, 30, 31]. Conditions such as congestive heart failure, hepatic failure, obesity, pregnancy, abdominal compression, and arteriovenous malformation can produce dilatation of the epidural veins, which are part of the valveless venous network communicating with the inferior vena cava, the azygos system, and the pelvic veins [15, 27, 28, 32]. Epidural veins have been reported to cause radiculopathy, urinary retention, myelopathy, and low back pain [30–33].
24.2.2 Pelvic Girdle Syndrome
Pelvic girdle pain is common during pregnancy and childbearing period [2–4]. It is due to overload on the hips, sacroiliac joints, and pubic symphysis and to increased levels of the hormone relaxin that contributes to ligamentous laxity [16].
Pain is usually located in the lower spine, between the posterior iliac crest and the gluteal folds, centered on sacroiliac joints, and radiates posteriorly to the thighs without a true radicular distribution [15]. The pain is usually intermittent and can be precipitated by prolonged sustained postures and simple activities such as walking, sitting, or standing [34]. This condition is usually well assessed clinically and imaging is required only in case of severe uncontrolled symptoms [4, 27].
Stress on the symphysis pubis during pregnancy may cause acute changes, especially in the postpartum period. Even in asymptomatic pregnant women, MRI can depict higher water content in the cartilage and edema in the parasymphyseal bone [35].
Rarely increased load can lead to disruption of the pubic symphysis, with widening of the pubic space and a gap larger than 10 mm as measured by ultrasound or fluid collection in the symphysis [36].
24.2.3 Coccygodynia
Childbirth is a common cause of coccygodynia which consists in pain in the coccyx area in the sitting position [37]. Coccygodynia appears usually the day after delivery, when the patient assumes a sitting position. This condition can be evaluated with radiographies that can show a rigid (fused with the sacrum), dislocated, or hypermobile (>35° on dynamic radiography in flexion or extension) coccyx [38]. However, if coccygodynia appears during pregnancy, as in cases of short perineum [37], MRI is the best imaging modality to assess this condition [39]. Intraosseous edema and changes to the soft tissue surrounding the sacrococcygeal joint are well assessed by MRI fat suppression images and can be considered the source of pain (Fig. 24.4).
Fig. 24.4
Coccygeal instability with anteverted coccyx in a 29-year-old woman with coccydynia 8 weeks after childbirth. Sagittal FSE T2-weighted (a) and STIR (b) images show hypersignal areas at the level of pre-coccygeal and post-coccygeal spaces indicative of edema (arrows)
24.2.4 Osteitis Condensans Ilii
Osteitis condensans ilii consists in bone sclerosis in the inferior aspect of the iliac bone adjacent to sacroiliac joint [6, 40]. This condition has a high prevalence in women with previous pregnancy but it is not unique of this population [41]. Clinically, osteitis condensans manifests with low back pain and tenderness in the sacroiliac joints. Imaging is required if a differential diagnosis with chronic sacroiliitis is needed (Figs. 24.5, 24.6, and 24.7).
Fig. 24.5
Osteitis condensans ilii in a 38-year-old woman. Patient reported progressive left sacral pain occurring at 8 months of pregnancy. Axial oblique T1-weighted (a) and STIR (b) images obtained during early postpartum period show severe subchondral bone sclerosis (arrows) particularly evident on the iliac side. There is also mild marrow bone edema, visible on the axial oblique STIR (arrows in b). Note the absence of bone erosions and reactive synovitis, finding that allows the differential diagnosis with chronic sacroiliitis
Fig. 24.6
Chronic osteitis condensans ilii in a 35-year-old woman at 23 weeks of gestational age. The findings of hypointense signal intensity (arrows) on axial T1-weighted (a) and STIR (b) images at the level of the iliac side are indicative of subchondral bone sclerosis, confirmed by CT (c), performed after delivery
Fig. 24.7
Osteitis condensans ilii, in a 38-year-old woman. Patient reported progressive left sacral pain occurring at 7 months of pregnancy. Coronal T1-weighted (a) and STIR (b) images obtained during early postpartum period show mild marrow subchondral edema (arrow) of the left sacrum iliac joint. Same patients also suffered from lateral hip rotators overload: axial T1-weighted (c) and STIR (d) images show partial tear of the gluteus medius at the trochanteric insertion (arrows) associated with reactive trochanteric bursitis
CT well depicts the presence of triangular-shaped subchondral sclerosis along the iliac side of the sacroiliac joints bilaterally [42]. MRI demonstrates vertical T1 and T2 hypointense linear foci along the sacral alae representing fracture lines and T1 hypointense and T2 hyperintense signal in the surrounding bone marrow representing associated edema [1, 6].
The clinical differential diagnoses include sacroiliitis with inflammatory or infectious causes, osteitis condensans ilii, lumbosacral degenerative spondylosis, and transient regional osteoporosis of the sacrum [6]. The diagnosis of osteitis condensans ilii is more consistent in the presence of only subchondral sclerosis along the iliac side of the sacroiliac joint and absent joint effusion or erosions in conjunction with the clinical history of recent pregnancy and labor [1]. Treatment is usually conservative including bed rest and analgesics until resolution of the pain [40, 41].
24.3 Bone Mineral Density
Major changes occur in maternal calcium homeostasis during pregnancy and breastfeeding [7]. There are discrepant data with some studies reporting that BMD changes in response to the transfer of calcium to the fetus in combination with decreased renal calcium reabsorption, while others have reported unchanged or even increased BMD due to high levels of estradiol and increased intestinal calcium reabsorption due to 1,25-dihidroxyvitamin D levels which protects against bone loss [7, 43–52].
However, there is a large accordance that pregnancy could be a risk factor for developing a new onset or worsening of a preexisting osteoporosis [43–57]. Bone mineral density decreases gradually during pregnancy and breastfeeding, but the occurrence of true osteoporosis is rare [1]. Pregnancy and breastfeeding cause a reversible bone loss, which is in early phases limited to the trabecular bone, but it involves cortical bone during prolonged breastfeeding [46, 58–61].
A controlled cohort study [7] demonstrated that compared to controls BMD decreased in pregnant women of 1.8 % at the lumbar spine, of 3.2 % at the total hip, of 2.4 % at the whole body, and of 4.2 % at the ultradistal forearm. Breastfeeding has an additional effect on BMD decreased in postpartum period. At 9 months postpartum, women who had breastfed for less than 9 months had a BMD similar to that of controls, while those who were still breastfeeding had a further decrease in BMB at the lumbar spine and hip.
During prolonged breastfeeding, BMD started to be regained at sites of most trabecular bone, but it decreases further at sites rich of cortical bone [7]. Similarly amenorrhea length has an impact on BMD changes, being correlated to breastfeeding length [7]. At 19 months postpartum, BMD returns at prepregnancy level, independently of breastfeeding length. Calcium and vitamin D intake is not associated to BMD changes [7].
Body composition also changes during pregnancy with an increase of fat and lean tissue mass. In postpartum, fat mass tends to have a slower decline in women who continue breastfeeding.
BMD changes in pregnancy and breastfeeding may predispose to osteoporosis and increased risk of fractures.
24.4 Fractures
Pregnancy-related fractures can have different origin. Fractures can be caused by an overload on a normal bone, fatigue or stress fractures, or to a normal load on a weakened osteoporotic bone, insufficiency fractures [1]. The vertebras, sacrum, iliac bone, and femoral head can be affected. MRI detects bone fractures as a line of hypointensity in all sequences lining deeply the articular surface, surrounded by bone edema [1].
Risk factors for fatigue sacral stress related to pregnancy and postpartum include vaginal delivery of a high birth weight infant, increased lumbar lordosis, excessive weight gain, and rapid vaginal delivery [1]. Sacral fatigue fractures can occur also in healthy young woman other than in relation to pregnancy, particularly in long-distance runners or athletes [1]. Imaging features of pregnancy-related fractures are similar to those related to involutional osteoporosis. Radiographs may be normal or demonstrate unilateral or bilateral areas of sclerosis along the sacral wings. Sacral stress fracture lines run parallel to the sacroiliac bone with a typical T1 and T2 hypointense vertical line surrounded by T2 hyperintensity representing edema [6, 62, 63]. Differential diagnosis includes sacroiliitis, with inflammatory or infectious cause, osteitis condensans ilii, lumbosacral degenerative spondylosis, and transient regional osteoporosis of the sacrum.
Femoral head stress fractures are usually located on an area of maximum load, the anterior and superior aspect of the femoral head [62]. Subchondral fractures are seen as curvilinear lines or bands paralleling the subchondral bone and surrounded by edema [1, 5, 62, 63]. This finding distinguishes fractures from osteonecrosis where a serpiginous line of demarcation with double signal intensity extends to the subchondral bone on both sides and delineates the zone of infarction [1, 5, 62, 63].
24.5 Hip Disorders
Despite a reported 38 % of hip pain during pregnancy, true hip disease is very rare during pregnancy and early postpartum (with reported data of 3/4900) [5]. However, they cause a significant clinical impairment and must be considered by the clinician. Hip disorders during pregnancy usually involve the femoral head, and the most frequent are transient osteoporosis and stress fractures, while osteonecrosis occurs less frequently [5, 64].
Transient osteoporosis is related to pregnancy, which is a predisposing factor for this condition. It is associated to the third trimester of pregnancy [5, 65–67]. Clinical examination usually doesn’t show a limitation of movements while the pain is so intense to prevent gait [67]. MRI shows bone marrow edema in the femoral head and neck (Fig. 24.8), joint effusion, and capsular thickening (66–74), while x-rays can show regional osteoporosis [67] and osteopenia at DEXA examination [5]. Transient osteoporosis can complicate with secondary spontaneous fractures, subchondral fractures, seen as a line of hypointensity lining deeply of the subchondral bone. Pathogenesis of transient osteoporosis is related to altered calcium homeostasis during pregnancy even if other less convincing hypotheses have been advocated, such as algodystrophy, impaired venous flow in the femoral head, or nerve compression [5, 66–74].
Fig. 24.8
Bilateral transient osteoporosis of the hip in a 35-year-old woman; pain initially occurred on the right lip, after 6 months of pregnancy, followed by contralateral side 1 month later. Coronal T1-weighted (a) and STIR (b) and axial T1-weighted (c) and STIR (d) images obtained during early postpartum period show bilateral bone marrow edema (arrows) of femoral heads and joint effusions. Coronal STIR image (e) after 5 months of treatment detects edema resolution
In stress fractures symptoms occur very late, at 32nd–41st gestational week with severe pain during walking relieved by rest, and resolved spontaneously 2–5 months after onset [1]. This condition has been reported to be the second cause of pregnancy-related hip disease [5]. An explanation could be bone fragility due to transient osteoporosis. They could be secondary fracture, such as complication of osteoporosis, or true stress fractures due to preexisting bone fragility associated to overload or a combination of both [5]. The hypothesis of true stress fracture is supported by the fact that they appear early during pregnancy and visible at MRI if performed soon, as conventional x-ray examinations are usually negative [5, 62]. In later phases x-rays, to be better performed after delivery, can show a subchondral linear radiolucency representing a fracture line or a focal area of sclerosis and sequently a subtle focal depression on femoral head contour [62]. MRI shows fracture as a thin hypointense line in all sequences (Fig. 24.9) occurring in the femoral head and the upper part of the neck or both or a linear band parallel to the subchondral bone [62, 63]. Other findings are marked bone marrow edema, contour abnormalities of the femoral head, and joint effusion, despite lower compared to transient osteoporosis [5, 62]. The finding of a linear hypointense band surrounded by edema is quite specific for subchondral fractures, and it distinguishes them from the well-defined zonal pattern of osteonecrosis [62, 63]. However, in case of advance femoral head collapse, this finding may not be evident so a distinction between the two conditions is more challenging [62].
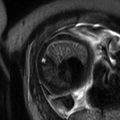
Fig. 24.9
Stress fracture of the right femoral neck in a 40-year-old woman at 22 weeks of gestational age. Coronal T1-weitghted (a) and STIR (b) sequences show hypointense signal of the fracture line (arrow), surrounded by edema. Coronal reformatted CT (c) performed after delivery shows a thin hyperattenuating line
MRI is the modality of choice respect to conventional x-rays, owing to the lack of ionizing radiation and because it can show signs of very early stage (bone edema and joint effusion).
Transient osteoporosis and stress fractures are reversible and self-limiting conditions, with a clinical and radiographic resolution after conservative treatment, and they need to be distinguished from osteonecrosis of the femoral head [1].
Osteonecrosis (ON) of the femoral head occurs rarely. Pregnancy-related ON represents about 2 % of all cases [5, 64, 75–78]. Imaging features do not differ from idiopathic ON; however, a predilection for unilateral involvement, especially the left one, has been reported; moreover women with pregnancy-related ON were also more likely to undergo their first pregnancy at an older age (5). The cause of pregnancy-related ON is not clear; some mechanisms have been postulated such as pelvic venous congestion, lipid disturbance, higher serum cortisol, and state of hypercoagulability [5].
MRI is highly sensitive for the diagnosis of ON of the femoral head [79–84] (Fig. 24.10). A normal fat intensity area with a surrounding low-intensity band on T1-w sequences and a double line sign on T2-w, which represent the boundary of the necrotic lesion, are frequently seen in pre-radiological (stage 1) and radiologically non-collapsed stage (stage 2) of ON, according to ARCO (Association Research Circulation Osseous) classification. In stage 3 (radiological collapsed) and stage 4 diseases, necrotic tissue and reparative tissue coexist with homogeneous and inhomogeneous hypointense areas on T1, although T2 can sometimes differentiate between necrotic tissue (fat like or low intensity) and reactional tissue (intermediate intensity). Hypointense bands should represent necrosis although necrotic cells can still be hyperintense on T2 until the area of necrosis becomes more extensive [63]. A peripheral rim of enhancement after i.v. injection of gadolinium at the boundary of the altered signal intensity area is consistent with reparative fibrous tissue and repaired marrow; the peripheral rim of enhancement corresponds to necrotic trabecular bone [63]. However, the use of gadolinium should be reserved only in case of doubt as potential adverse effects on the fetus are not known. Extralesional reactive changes consist of dilated vessels and bone marrow edema [63]. The presence of edema represents an inflammatory change in the reparative process both in case of collapsed head and in non-collapsed head; in this latter change, it may indicate that the femoral head has begun to collapse microscopically [63].
Fig. 24.10




Bilateral avascular necrosis of femoral head in a 25-year-old woman who accused severe hip pain during late pregnancy, treated with conservative treatment. Coronal and axial T1-weighted (a, b) and axial STIR (c) images performed after delivery show areas of avascular necrosis in the head of femurs, with typical map-like morphology (arrows)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree