Many pathologies of the musculoskeletal system involve nontraumatic causes. MR imaging is used in the diagnosis because of its high sensitivity and specificity compared with other modalities. Osteomyelitis, osteonecrosis of the femoral head, and stress fractures are pathologies of bone where early diagnosis and intervention usually lead to an improved outcome. Joint aspiration and culture is the standard for diagnosing septic arthritis. MR imaging can support the diagnosis and allows evaluation for adjacent abscess and osteomyelitis. Early in the disease process, necrotizing fasciitis may not be clinically suspected and imaging may provide the first indication of the presence of this potentially deadly infection.
Key points
- •
MR imaging is highly sensitive and sometimes specific in the diagnosis of many nontraumatic musculoskeletal emergencies.
- •
Imaging should not delay the treatment of acute compartment syndrome and necrotizing fasciitis.
- •
T1-weighted and fat-suppressed fluid-sensitive sequences (T2-weighted or STIR) are the critical MR imaging protocol components.
Bones
Osteomyelitis
Osteomyelitis is an infection of bone that can involve cortical bone and bone marrow. Typical causes include direct extension from overlying soft tissue including ulcers and posttraumatic infections, and hematologic spread. Delay in diagnosis can lead to significant morbidity, making early detection and diagnosis critically important.
Diabetic ulcers and posttraumatic infections are frequent clinical presentations that may lead the clinician to suspect osteomyelitis from direct extension. A physical examination demonstrates cellulitis and soft tissue defects, although imaging is often performed to evaluate for associated abscess and osseous involvement. These additional imaging findings may affect treatment management.
Hematologic spread of bacteria to bone usually presents with fever and lethargy. Depending on which bone is involved, localized soft tissue swelling, decreased range of motion, and focal pain are additional symptoms. These localizing findings provide an indication of field of view coverage for imaging.
Normal anatomy and imaging technique
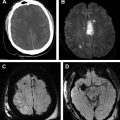
MR imaging is useful for suspected cases of osteomyelitis because of its high sensitivity for detection of disease, for evaluating early changes in bone marrow composition, and for determining the extent of the disease ( Fig. 1 ). MR imaging has been shown to be capable of detecting changes in bone marrow within 3 days of infection. Protocols include T1-weighted and fluid-sensitive sequences, including T2-weighted fat-suppressed or short-tau inversion recovery (STIR). Precontrast and postcontrast T1-weighted sequences are often performed, although osteomyelitis can be diagnosed without such sequences.
Beyond its usefulness for diagnosis, MR imaging can affect how the patient is to be treated. Compared with other modalities, the higher sensitivity of MR imaging leads to earlier treatment and potentially improved patient outcomes. If antibiotics fail and surgery is warranted, the amount of devitalized tissue and adjacent critical structures can be identified, modifying the approach accordingly to minimize complications and morbidity. Imaging planes should include a short axis (axial) and at least one long axis (sagittal or coronal).
One particular anatomic consideration should be raised when dealing with hematologic spread in pediatric cases. The metaphyses of long bones are highly vascularized; with an open physis, vessels do not cross the growth plate. The result is slower flow in the metaphysis and more chances for bacterial seeding in this region of bone in the pediatric population ( Fig. 2 ).
Imaging Protocols
Primary Protocol
- •
T1-weighted non-fat-suppressed
- •
Fluid-sensitive sequence (T2-weighted fat-suppressed or STIR)
- •
Additional Sequences
- •
Precontrast and postcontrast T1-weighted fat-suppressed
- •
Imaging findings and pathology
The characteristic signal of normal fatty bone marrow is critical for the evaluation of osteomyelitis. On T1-weighted sequences, fatty marrow is hyperintense. On fat-suppressed sequences, the signal becomes hypointense. When bone becomes infected, the medullary cavity is filled with bacterial cells, exudative debris, and edema leading to alterations in the normal appearance of the marrow. A T1-weighted sequence demonstrates a geographic, confluent, low signal-intensity, and fluid-sensitive sequences show high signal intensity.
Reactive bone marrow edema from surrounding soft tissue infection or postinfectious granulation tissue within the marrow space may complicate the diagnosis. In these cases, the bone marrow signal demonstrates T2-weighted hyperintensity that is related to osteitis but there is no active bone infection. T1-weighted sequences demonstrate hazy, reticular, and subcortical hypointensity with osteitis.
After the appropriate treatment of osteomyelitis, abnormal marrow signal changes persist for months. A low signal remains on T1-weighted sequences, which can lead to difficulty in evaluating for persistent infection. Comparison with prior examinations or serial MR imaging examinations evaluating the extent of involved bone may provide the only imaging clue to decipher postinfectious granulation tissue from persistent, active infection. However, in these situations, the clinical response to therapy may supersede the imaging findings.
The imaging findings in chronic osteomyelitis vary from those observed in acute osteomyelitis. Acute osteomyelitis is an aggressive process with osteolysis and marked edema. Chronic osteomyelitis demonstrates cortical thickening, sequestrum (a small piece of dead bone with low signal on T1- and T2-weighted sequences), involucrum (periosteal new bone surrounding the sequestrum), and cloaca (sclerotic margin at the periosteal interface surrounding a draining sinus) ( Fig. 3 ). MR imaging is the more desirable modality for the evaluation of acute osteomyelitis. However, in cases of chronic osteomyelitis, computed tomography is more sensitive for detecting a sequestrum, the presence of which indicates active infection.
Postcontrast imaging offers no additional information for the diagnosis of osteomyelitis, although it can help diagnose an associated abscess in the adjacent soft tissues or intraosseous (Brodie abscess). This finding is critically important because interventional or surgical drainage may be required.
Diagnostic Criteria
- •
Primary: geographic, medullary, confluent area of T1-weighted hypointensity
- •
Secondary: bone marrow edema, periosteal reaction, ulcer, cellulitis, sinus tract, abscess, cortical interruption
- •
Chronic osteomyelitis: sequestrum, involucrum, and cloaca
Differential Diagnosis
- •
Charcot joint
- •
Osteitis
- •
Stress reaction
- •
Metastatic lesion
- •
Primary bone neoplasm
- •
Langerhans cell histiocytosis of bone
Pearls
- •
Highly sensitive
- •
Early diagnosis
- •
Evaluate for abscess and other associated complications
Pitfalls
- •
Distinguishing postinfectious granulation tissue versus persistent, active infection
- •
Imaging orthopedic hardware
- •
Acute neuropathic osteolysis and osteomyelitis have similar imaging appearance
What the Referring Physician Needs to Know
- •
MR imaging is highly useful for the diagnosis of osteomyelitis
- •
Diagnosis can be made without intravenous contrast, although contrast helps evaluate for adjacent abscess
- •
Localizing the area of suspected osteomyelitis can lead to increased diagnostic accuracy (high resolution)
- •
Orthopedic hardware and neuropathic joints decrease the sensitivity and specificity of diagnosis
- •
Persistent, active infection can appear similar to posttreatment changes and comparison or serial examinations may be needed
Summary
MR imaging allows for the early detection of osteomyelitis with high sensitivity in the appropriate clinical setting. In addition to diagnosis, MR imaging is useful for guiding patient management and to assess complications that could modify the treatment regime. Postcontrast imaging provides additional information, primarily about the surrounding soft tissues. Difficulties in diagnosis arise in assessing for persistent, active infection, in patients with orthopedic hardware, and in neuropathic joints.
Osteonecrosis of the Femoral Head
The incidence of osteonecrosis of the femoral head (ONFH) is increasing, with causes including exogenous steroid use and trauma. Initially, patients may be asymptomatic, but joint destruction may result if the condition is not recognized early. Once hip pain is present, joint replacement is usually required within 3 years. This may occur in patients younger than 50, but it is not limited by age. Traumatic causes of ONFH are unilateral. When other causes (eg, exogenous steroids, alcohol, smoking, hemoglobinopathies) are suspected, imaging should include both hips to evaluate for clinically occult ONFH.
Normal anatomy and imaging technique
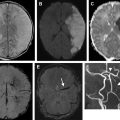
The major blood supply to the epiphysis of the femoral head is the posterior-superior retinacular arteries ( Fig. 4 E ). The vessels are within the joint capsule as they cross the femoral neck and branch into the lateral epiphyseal vessels, which supply the femoral head. Trauma to the femoral head/neck area results in disruption or kinking of the distal posterior superior reticular arteries, whereas other etiologies cause occlusion of the vessels.
MR imaging is a markedly sensitive and specific modality. Protocols should include a large field of view covering both hips given the high incidence of bilateral disease ( Fig. 4 A, B). T1-weighted and fluid-sensitive sequences (T2-weighted fat-suppressed or STIR) are commonly used for diagnosis. Postcontrast sequences are not routinely acquired, although they may provide additional detail when the diagnosis is not definitive.
Imaging Protocols
Large field of view (both hips)
- •
T1-weighted non-fat-suppressed coronal
- •
Fluid-sensitive fat-suppressed coronal
- •
Fluid-sensitive fat-suppressed axial
- •
T1-weighted non-fat-suppressed axial (optional)
- •
Small field of view (affected hip)
- •
T1-weighted non-fat-suppressed (two planes)
- •
Fluid-sensitive fat-suppressed (two planes)
- •
Imaging findings and pathology
A specific staging system (Ficat ) for ONFH includes radiography, MR imaging, and bone scan findings. An MR imaging classification of avascular necrosis has also been developed based on the central avascular segment signal. Earliest changes in the femoral head are usually subchondral at the superior femoral head and starting at the anterior portion.
Ficat Classification (MR imaging findings)
Stage 0: normal
Stage 1: bone marrow edema
Stage 2: geographic defect
Stage 3: crescent sign with possible cortical collapse
Stage 4: secondary degenerative changes
MR Imaging Avascular Necrosis Classification
Class A: signal analogous to fat; hyperintense T1-weighted; intermediate to high T2-weighted signal
Class B: signal analogous to blood; hyperintense T1-weighted and T2-weighted signal
Class C: signal analogous to fluid; hypointense T1-weighted; high T2-weighted signal
Class D: signal analogous to fibrous tissue; hypointense T1-weighted and T2-weighted
T1-weighted findings vary depending on the underlying pathology. If there is subchondral edema then T1-weighted signal is low. With blood products, T1-weighted signal is high. In both cases, there is a peripheral hypointense band outlining the area of osteonecrosis extending to the subchondral plate. This band represents the junction between reparative and necrotic zones.
On T2-weighted sequences, a double-line sign is diagnostic of ONFH. There is a peripheral hypointense band similar to T1-weighted sequences with an additional high signal inner peripheral band. The inner hyperintense band represents granulation tissue and is present in up to 80% of cases. Focal areas of T2-weighted low signal represent necrotic or fibrous tissue ( Fig. 4 C, D). Occasionally a focal lesion may not be present in the femoral head, which makes the diagnosis more difficult. Edema may be the only finding if imaged before an identifiable reactive/necrotic zone interface develops. Contrast imaging may provide additional detail for distinguishing osteonecrosis from transient edema (nonviable from viable tissue).
Diagnostic Criteria
- •
Variable central T1-weighted signal at the superior femoral head with a low signal peripheral rim
- •
Variable central T2-weighted signal at the superior femoral head with low signal peripheral rim; double line sign, if present, is pathognomonic
Differential Diagnosis
- •
Transient osteoporosis of the hip
- •
Transient bone marrow syndrome
- •
Bone contusion
- •
Subchondral fracture
Pearls
- •
Most sensitive modality
- •
Larger MR imaging lesions have a greater tendency for femoral head collapse
- •
Low signal peripheral rim and double line sign provide high diagnostic accuracy
Pitfalls
- •
MR imaging classification has low predictive value in femoral head collapse
- •
Failure to identify associated subchondral fracture
- •
T1-only protocols have higher false-negative rate
What the Referring Physician Needs to Know
- •
In addition to history and physical examination, MR imaging is a critical component for evaluation, especially in younger patients
- •
Stage, extent of necrosis, and degree of joint involvement have prognostic value
- •
Comprehensive quantitative staging system allows for optimal evaluation and treatment, unlike older nonquantitative systems
Summary
ONFH may initially be asymptomatic but can progress to joint destruction if not appropriately identified and treated. MR imaging is the most sensitive and specific modality and screening of both hips should be performed to diagnose clinically occult disease. Imaging with T1- and T2-weighted sequences is optimal for evaluation. Peripheral low signal intensity band and double line sign represent the junction of necrotic and fibrous tissue and are critically important diagnostic criteria. The extent of necrosis and joint involvement has prognostic value compared with older staging methods.
Stress Fracture
Stress fractures encompass two different types of injuries: fatigue fractures and insufficiency fractures. Fatigue fractures arise from abnormal stress on normal bone, seen commonly in young, active individuals. These injuries occur frequently in athletes engaging in repetitive activity, often when the activity is first begun. Running and gymnastics are popular activities that result in fatigue fractures. The lower extremities, more specifically the medial neck of the femur and pelvic ring, are commonly affected and may demonstrate bilateral abnormalities. Upper extremity injuries are less common and typically unilateral.
Insufficiency fracture is normal stress on abnormal bone and is common in elderly women. Pathologic conditions that weaken bone are the leading risk factor, with osteoporosis and long-term bisphosphonate use being common etiologies. This injury occurs almost exclusively in weight-bearing locations including the spine, sacrum, and femurs.
Stress fractures present with pain regardless of cause. With fatigue fractures, performing a repetitive activity exacerbates the pain, which improves with rest. Insufficiency fractures are most commonly atraumatic or result from low-impact mechanisms.
Normal anatomy and imaging technique
MR imaging is the most sensitive and specific modality for stress fractures. Similar to imaging of traumatic injuries, T1- and T2-weighted fat-suppressed sequences are essential to the diagnosis. When imaging the extremities, axial and coronal planes are frequently used. For example, fatigue fractures of the femoral neck are commonly medial and insufficiency fractures lateral, and are most conspicuous in the coronal plane. However, the sagittal plane may provide the most diagnostic information for sternal and vertebral insufficiency fractures.
Imaging Protocols
- •
T1-weighted: coronal and axial planes (sagittal for sternum and spine)
- •
Fluid-sensitive sequence (T2-weighted fat-suppressed or STIR): coronal and axial planes (sagittal for sternum and spine)
- •
Precontrast and postcontrast sequences: performed if pathologic fracture is suspected (discussed separately)
Imaging findings and pathology
MR imaging’s increased sensitivity over radiography and superior specificity compared with bone scan make it the optimal imaging decision. Diagnosis is based on linear T1-weighted hypointensity with associated T2-weighted hyperintensity that commonly extends into the surrounding soft tissues ( Figs. 5 and 6 ). Insufficiency fractures follow a pattern where the lateral periosteum and cortex are initially affected and may present as incomplete fractures.
Bisphosphonate-related insufficiency fractures are typically located at the proximal third of the femur. These fractures have an atypical fracture pattern and are a diagnosis of exclusion. This fracture pattern occurs more frequently in older women treated continuously with bisphosphonates. The causative mechanism is unknown. One theory proposes that long-term bisphosphonate therapy limits bone remodeling from microtrauma, leading to fragility.
Diagnostic Criteria
- •
T1-weighted linear low marrow signal intensity usually arising from the cortex and perpendicular to the surface of bone
- •
Diffuse T2-weighted hyperintensity with low signal fracture line
Differential Diagnosis
- •
Traumatic fracture
- •
Stress reaction
- •
Pathologic fracture
- •
Osteoid osteoma
Pearls
- •
MR imaging is highly sensitive and specific
- •
Identify other causes (soft tissue, bone, or joint) for pain
- •
Linear low signal component is classic criteria for stress fracture (bone contusion is microfracture without discrete low signal line)
Pitfalls
- •
Failure to identify underlying lesion with insufficiency fracture (pathologic fracture)
- •
Delay in obtaining diagnosis (with MR imaging) may lead to a worse outcome, such as complete fracture and lengthened recovery time
What the Referring Physician Needs to Know
- •
Radiographs are frequently normal for suspected stress fractures
- •
MR imaging provides superior sensitivity and the ability to diagnose other causes for pain
- •
MR imaging is performed without contrast unless pathologic fracture is a clinical concern
Summary
Stress fractures encompass fatigue and insufficiency fractures. Fatigue fracture is abnormal stress on normal bone. Insufficiency fracture is normal stress on abnormal bone. Radiographs are frequently normal and MR imaging provides better diagnostic capabilities. T1-weighted and fluid-sensitive sequences provide high diagnostic accuracy and ability to diagnose other etiologies for pain.
Pathologic Fracture
Pathologic fractures are a type of insufficiency fracture. An underlying lesion within the bone weakens the structure so that normal stress leads to fracture. Frequently, these fractures are associated with malignant lesions, with metastasis the most common. Benign lesions, including bone cysts and fibrous lesions, have also been seen with pathologic fractures.
When a patient presents with a fracture, it is important to exclude an underlying lesion. Patient history, atypical fracture pattern, and radiographic findings can lead to suspicion of an underlying lesion. Recent advancements in MR imaging protocols have made this evaluation more sensitive and specific.
Normal anatomy and imaging technique
Typical appearance of fatty bone marrow (high signal) on T1-weighted sequences is useful for detecting the presence of an underlying lesion. A lesion replaces the normal bone marrow, leading to well-defined T1-weighted marrow signal hypointensity. T1-weighted in-phase and opposed-phase (chemical shift) sequences can assist in the diagnosis especially when the fracture site has a heterogeneous T1-weighted signal secondary to hemorrhage ( Fig. 7 ). Fluid-sensitive and contrast sequences are less specific given potential similarities between stress and pathologic fractures. Diffusion-weighted imaging (DWI) is another sequence that may help the radiologist determine the presence of an underlying lesion.
Imaging Protocols
- •
T1-weighted: axial and long-axis planes
- •
T2-weighted fat-suppressed or STIR: axial and long-axis planes
- •
Chemical shift (in-phase and opposed-phase): axial plane
- •
Diffusion imaging with ADC mapping: axial plane
- •
Precontrast and postcontrast T1-weighted fat-suppressed axial, sagittal, and coronal
- •
Precontrast and postcontrast subtraction images
Imaging findings and pathology
Evaluation with T1-weighted, T2-weighted, and postcontrast sequences can be confusing when trying to determine whether a fracture is pathologic. MR imaging signal intensities of an uncomplicated fracture and pathologic fracture can be much alike. T1-weighted sequences are optimal for evaluating the extent of a marrow-replacing tumor because of the contrast between tumor and fatty marrow. However, in the acute phase of a fracture, edema and hemorrhage replace the normal marrow signal resulting in T1-weighted hypointensity and T2-weighted hyperintensity. After contrast administration, there is enhancement at the fracture site. Secondary imaging findings, including endosteal scalloping and adjacent soft tissue abnormalities, have been shown to help with the diagnosis in these cases.
Chemical shift is a fast imaging technique that can distinguish marrow-replacing tumor from hematopoietic marrow or hemorrhage within the medullary cavity. In normal fatty marrow, in-phase demonstrates additive signal from water and fat in the same voxel, but opposed-phase shows dropped signal. When a marrow-replacing tumor is present, the opposed-phase sequence does not show a decreased signal when compared with the in-phase image.
DWI is a method of functional imaging commonly used when evaluating the central nervous system. DWI measures the movement of water in the intracellular and extracellular spaces. Within a tumor there is restricted diffusion because of the high cellularity that limits water motion. Correlation with an ADC map is essential to provide a quantitative assessment of the cellularity of a region rather than relying only on the qualitative assessment of DWI.
Diagnostic Criteria
- •
Well-defined T1-weighted focal hypointensity at the fracture site (chemical shift and DWI imaging may provide additional diagnostic information)
- •
Endosteal scalloping
- •
Associated soft tissue component
Differential Diagnosis
- •
Traumatic fracture
- •
Stress fracture
Pearls
- •
MR imaging increases sensitivity and specificity for diagnosis
- •
Chemical shift and DWI imaging provide additional tools to increase diagnostic accuracy
Pitfalls
- •
Hemorrhage at the fracture site can lead to confusion in interpretation
What the Referring Physician Needs to Know
- •
Pathologic fracture is a type of insufficiency fracture
- •
Patient history, atypical fracture pattern, or radiographic findings may lead to suspicion of a pathologic fracture
- •
MR imaging can be used in indeterminate cases
Summary
Pathologic fracture is a subtype of insufficiency fracture. T1-weighted and chemical shift sequences are important for evaluating changes in the normal marrow signal. If there is clinical or radiographic suspicion of an underlying lesion, MR imaging frequently can assist in the diagnosis and, perhaps, alter the treatment.
Bones
Osteomyelitis
Osteomyelitis is an infection of bone that can involve cortical bone and bone marrow. Typical causes include direct extension from overlying soft tissue including ulcers and posttraumatic infections, and hematologic spread. Delay in diagnosis can lead to significant morbidity, making early detection and diagnosis critically important.
Diabetic ulcers and posttraumatic infections are frequent clinical presentations that may lead the clinician to suspect osteomyelitis from direct extension. A physical examination demonstrates cellulitis and soft tissue defects, although imaging is often performed to evaluate for associated abscess and osseous involvement. These additional imaging findings may affect treatment management.
Hematologic spread of bacteria to bone usually presents with fever and lethargy. Depending on which bone is involved, localized soft tissue swelling, decreased range of motion, and focal pain are additional symptoms. These localizing findings provide an indication of field of view coverage for imaging.
Normal anatomy and imaging technique
MR imaging is useful for suspected cases of osteomyelitis because of its high sensitivity for detection of disease, for evaluating early changes in bone marrow composition, and for determining the extent of the disease ( Fig. 1 ). MR imaging has been shown to be capable of detecting changes in bone marrow within 3 days of infection. Protocols include T1-weighted and fluid-sensitive sequences, including T2-weighted fat-suppressed or short-tau inversion recovery (STIR). Precontrast and postcontrast T1-weighted sequences are often performed, although osteomyelitis can be diagnosed without such sequences.
Beyond its usefulness for diagnosis, MR imaging can affect how the patient is to be treated. Compared with other modalities, the higher sensitivity of MR imaging leads to earlier treatment and potentially improved patient outcomes. If antibiotics fail and surgery is warranted, the amount of devitalized tissue and adjacent critical structures can be identified, modifying the approach accordingly to minimize complications and morbidity. Imaging planes should include a short axis (axial) and at least one long axis (sagittal or coronal).
One particular anatomic consideration should be raised when dealing with hematologic spread in pediatric cases. The metaphyses of long bones are highly vascularized; with an open physis, vessels do not cross the growth plate. The result is slower flow in the metaphysis and more chances for bacterial seeding in this region of bone in the pediatric population ( Fig. 2 ).
Imaging Protocols
Primary Protocol
- •
T1-weighted non-fat-suppressed
- •
Fluid-sensitive sequence (T2-weighted fat-suppressed or STIR)
- •
Additional Sequences
- •
Precontrast and postcontrast T1-weighted fat-suppressed
- •

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree