The treatment of meniscal tears has evolved secondary to a better understanding of the essential roles that the menisci play in the normal function of the knee, including load transmission, stress distribution, shock absorption, joint lubrication, resistance to capsular and synovial impingement, and maintenance of joint congruity. Imaging evaluation of the menisci requires an understanding of the normal anatomy, the imaging criteria necessary to accurately diagnose a meniscal tear, meniscal tear patterns, and awareness of common diagnostic pitfalls.
Key points
- •
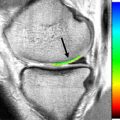
The magnetic resonance (MR) criteria for diagnosing a meniscal tear include either increased signal unequivocally contacting the articular surface or abnormal meniscal morphology in the absence of previous surgery.
- •
Accurate description of tear patterns is vital in guiding treatment options. The ISAKOS (International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine) arthroscopic tear classification system includes longitudinal-vertical, horizontal, radial, vertical flap, horizontal flap, and complex.
- •
Displaced tears may be overlooked on MR imaging and should be sought in the recesses, the posterior intercondylar notch, and popliteal hiatus in the setting of a blunted meniscus.
- •
Secondary signs may accompany meniscal tears and increase diagnostic confidence. The indirect signs with the highest positive predictive value include parameniscal cysts, linear subchondral edema, and meniscal extrusion.
Introduction
Arthroscopic partial meniscectomy is the most common orthopedic surgery performed in the United States. Perspectives on the function of the menisci, biomechanical effects after meniscectomy, and treatment algorithms continue to evolve, placing a greater emphasis on meniscal preservation and outcome measures. The potential deleterious effects of surgery have been known for some time: the landmark study in 1948 by Fairbank recognized that “meniscectomy is not wholly innocuous…” in the sentinel article recognizing the chronic maladaptive changes after a meniscectomy. More recently, studies have shown no difference in long-term improvement between patients undergoing partial meniscectomies and a sham procedure in the treatment of degenerative meniscal tears. In addition, symptomatic patients with meniscal tears and underlying chondrosis showed no difference in functional status when comparing surgery versus physical therapy alone.
Since its inception into clinical practice in the 1980s, magnetic resonance (MR) has become the preferred imaging method for evaluating the meniscus, with reported accuracies, sensitivities, and specificities ranging between 85% and 95% in detecting meniscal tears. Given the evolving treatment strategies, one must not only identify a tear but describe the location, extent, tear pattern, and any associated chondrosis to guide treatment options. The International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) Knee Committee formed a Meniscal Documentation Subcommittee in 2006, with the objective of developing a reliable classification system in the evaluation of the meniscus to facilitate outcome assessment. The tear patterns in this classification system include longitudinal-vertical, horizontal, radial, vertical flap, horizontal flap, and complex.
Therefore, the role of MR imaging has expanded to be not only a simple diagnostic study but a critical decision-making tool providing information that may not only alter the surgical technique but also provide information that would obviate surgery. This review focuses on normal anatomy, technical factors involved when imaging the meniscus, the imaging criteria for diagnosing meniscal tears, the imaging appearance of the various patterns of meniscal tears, secondary signs of meniscal injury, and common diagnostic pitfalls.
Anatomy
The shape and composition of the menisci confer an ability to absorb shock, distribute axial load, assist in joint lubrication, and maintain joint congruity in extremes of flexion and extension. The semilunar, triangular, fibrocartilaginous menisci are C-shaped, with a concave surface tapered centrally, conforming to the morphology of the femoral condyle, and a flat base attached to the condylar surface of the tibia via the anterior and posterior root ligaments ( Fig. 1 ). The intimate anatomic relationship and contiguous fibers between the anterior root ligament of the lateral meniscus and anterior cruciate ligament (ACL) insertion site result in a striated or comblike appearance, which can be mistaken for a meniscal tear ( Fig. 2 ). Although rarely identified on MR, a similar connection between the ACL and medial meniscus through the meniscocruciate ligament has been noted in several anatomic studies. A common variant of the anterior root of the medial meniscus is an insertion along the far anterior margin of the tibia, giving the false impression of extrusion or pathologic subluxation ( Fig. 3 ). The typical meniscal tibial attachment sites and their relationship with the cruciate ligaments are shown in Figs. 1 and 2 .



The configuration of 3 distinct layers of collagen within the meniscus and formation of collagen bundles oriented along both the long and short axes of the menisci allow for efficient load transmission and shock absorption. The longitudinal fibers are circumferentially oriented, resulting in the ability of the meniscus to distribute axial loads and provide what is commonly referred to as hoop strength. The more loosely organized radial fibers help form a lattice and act to tie the longitudinal bundles together and resist forces that would lead to longitudinal splitting of the meniscus ( Fig. 4 ).

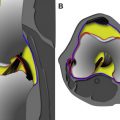
Each meniscus can be divided into thirds: an anterior horn, body, and posterior horn. The shape of the meniscus can be described best as an elongated semilunar triangle, with a concave hypotenuse and tapered ends. The result is a cross-sectional appearance, resembling either a slab or triangle, based on the orientation of the imaging plane in respect to the axis of the meniscus. The menisci resembles a triangle when imaged perpendicular to the free edge or long axis of the meniscus, such as sagittal images through the horns or coronal images through the body. The menisci takes on a more slab or bow tie configuration if the imaging plane parallels the long axis of the meniscus (eg, sagittal images through the body or coronal images through the horns).
Despite the similarities, the medial and lateral menisci are distinctly different. The larger, more open C-shaped medial meniscus increases in width from anterior to posterior, resulting in a larger posterior horn compared with the anterior horn when viewed in cross section. The more circular lateral meniscus maintains a relatively constant width, resulting in the anterior and posterior horns being nearly equal in size in cross section ( Fig. 5 ). Peripherally, the menisci are anchored to the fibrous capsule, with the medial meniscus firmly attached to the deep fibers of the medial collateral ligament, limiting its mobility and presumably leading to an increased susceptibility to injury compared with the more mobile lateral meniscus. The popliteomeniscal fascicles arise from the periphery of the posterior horn of the lateral meniscus and form a posterolateral meniscocapsular extension, which creates the popliteus hiatus. The fascicles not only form the hiatus, which allows the popliteus tendon an avenue to course intra-articularly and maintain the integrity of the joint, but stabilize and control the motion of the posterior horn. On MR imaging, the anteroinferior and posterosuperior fascicles are visualized in approximately 90% of knee examinations and best visualized on the sagittal fluid-sensitive sequences ( Fig. 6 ). Tearing of the posterosuperior fascicle is highly associated with tears of the posterior horn of the lateral meniscus, with a sensitivity, specificity, and positive predictive value of 89%, 96%, and 79% respectively.


Other normal anatomic structures and anatomic variants that can mimic a tear if not recognized include the meniscofemoral ligaments, oblique meniscomeniscal ligament, and the transverse meniscal ligament. The most commonly described meniscofemoral ligaments originate from the posterior horn of the lateral meniscus and insert onto the lateral aspect of the posterior medial femoral condyle, with the ligament of Humphry ( Fig. 7 ) coursing anterior to the genu of the posterior cruciate ligament (PCL) and the ligament of Wrisberg traveling behind the genu of the PCL. One potential pitfall occurs when a peripheral longitudinal tear is confused for a far lateral insertion of the meniscofemoral ligament. As a general rule, the attachment of the meniscofemoral ligaments to the posterior horn of the lateral meniscus should not extend greater than 14 mm beyond the lateral border of the PCL. Therefore, if the meniscofemoral ligament is identified on 4 or more sequential sagittal MR images beyond the PCL, a peripheral longitudinal tear should be suspected and reported as such. The lesser known and extremely uncommon anterior meniscofemoral ligament connects the anterior horn of the medial meniscus to the roof of the intercondylar notch and lies parallel and posterior to the ligamentum mucosum ( Fig. 8 ). This variant should not be confused for a displaced meniscal fragment.


The oblique meniscomeniscal ligament attaches the anterior horn of 1 meniscus to the posterior horn of the contralateral meniscus, coursing through the intercondylar notch between the cruciate ligaments. Present in 1% to 4% of knees, this structure should not be mistaken for a bucket handle meniscal tear.
The anterior transverse meniscal (geniculate) ligament typically connects the anterior horns of the menisci, although variations in its attachment exist. This structure is identified in 90% of dissections and 83% of MR examinations and can simulate an anterior root tear ( Fig. 9 ).
Recognizing and localizing each of these normal anatomic structures on serial images prevent inadvertently reporting a tear.
Introduction
Arthroscopic partial meniscectomy is the most common orthopedic surgery performed in the United States. Perspectives on the function of the menisci, biomechanical effects after meniscectomy, and treatment algorithms continue to evolve, placing a greater emphasis on meniscal preservation and outcome measures. The potential deleterious effects of surgery have been known for some time: the landmark study in 1948 by Fairbank recognized that “meniscectomy is not wholly innocuous…” in the sentinel article recognizing the chronic maladaptive changes after a meniscectomy. More recently, studies have shown no difference in long-term improvement between patients undergoing partial meniscectomies and a sham procedure in the treatment of degenerative meniscal tears. In addition, symptomatic patients with meniscal tears and underlying chondrosis showed no difference in functional status when comparing surgery versus physical therapy alone.
Since its inception into clinical practice in the 1980s, magnetic resonance (MR) has become the preferred imaging method for evaluating the meniscus, with reported accuracies, sensitivities, and specificities ranging between 85% and 95% in detecting meniscal tears. Given the evolving treatment strategies, one must not only identify a tear but describe the location, extent, tear pattern, and any associated chondrosis to guide treatment options. The International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) Knee Committee formed a Meniscal Documentation Subcommittee in 2006, with the objective of developing a reliable classification system in the evaluation of the meniscus to facilitate outcome assessment. The tear patterns in this classification system include longitudinal-vertical, horizontal, radial, vertical flap, horizontal flap, and complex.
Therefore, the role of MR imaging has expanded to be not only a simple diagnostic study but a critical decision-making tool providing information that may not only alter the surgical technique but also provide information that would obviate surgery. This review focuses on normal anatomy, technical factors involved when imaging the meniscus, the imaging criteria for diagnosing meniscal tears, the imaging appearance of the various patterns of meniscal tears, secondary signs of meniscal injury, and common diagnostic pitfalls.
Anatomy
The shape and composition of the menisci confer an ability to absorb shock, distribute axial load, assist in joint lubrication, and maintain joint congruity in extremes of flexion and extension. The semilunar, triangular, fibrocartilaginous menisci are C-shaped, with a concave surface tapered centrally, conforming to the morphology of the femoral condyle, and a flat base attached to the condylar surface of the tibia via the anterior and posterior root ligaments ( Fig. 1 ). The intimate anatomic relationship and contiguous fibers between the anterior root ligament of the lateral meniscus and anterior cruciate ligament (ACL) insertion site result in a striated or comblike appearance, which can be mistaken for a meniscal tear ( Fig. 2 ). Although rarely identified on MR, a similar connection between the ACL and medial meniscus through the meniscocruciate ligament has been noted in several anatomic studies. A common variant of the anterior root of the medial meniscus is an insertion along the far anterior margin of the tibia, giving the false impression of extrusion or pathologic subluxation ( Fig. 3 ). The typical meniscal tibial attachment sites and their relationship with the cruciate ligaments are shown in Figs. 1 and 2 .
The configuration of 3 distinct layers of collagen within the meniscus and formation of collagen bundles oriented along both the long and short axes of the menisci allow for efficient load transmission and shock absorption. The longitudinal fibers are circumferentially oriented, resulting in the ability of the meniscus to distribute axial loads and provide what is commonly referred to as hoop strength. The more loosely organized radial fibers help form a lattice and act to tie the longitudinal bundles together and resist forces that would lead to longitudinal splitting of the meniscus ( Fig. 4 ).
Each meniscus can be divided into thirds: an anterior horn, body, and posterior horn. The shape of the meniscus can be described best as an elongated semilunar triangle, with a concave hypotenuse and tapered ends. The result is a cross-sectional appearance, resembling either a slab or triangle, based on the orientation of the imaging plane in respect to the axis of the meniscus. The menisci resembles a triangle when imaged perpendicular to the free edge or long axis of the meniscus, such as sagittal images through the horns or coronal images through the body. The menisci takes on a more slab or bow tie configuration if the imaging plane parallels the long axis of the meniscus (eg, sagittal images through the body or coronal images through the horns).
Despite the similarities, the medial and lateral menisci are distinctly different. The larger, more open C-shaped medial meniscus increases in width from anterior to posterior, resulting in a larger posterior horn compared with the anterior horn when viewed in cross section. The more circular lateral meniscus maintains a relatively constant width, resulting in the anterior and posterior horns being nearly equal in size in cross section ( Fig. 5 ). Peripherally, the menisci are anchored to the fibrous capsule, with the medial meniscus firmly attached to the deep fibers of the medial collateral ligament, limiting its mobility and presumably leading to an increased susceptibility to injury compared with the more mobile lateral meniscus. The popliteomeniscal fascicles arise from the periphery of the posterior horn of the lateral meniscus and form a posterolateral meniscocapsular extension, which creates the popliteus hiatus. The fascicles not only form the hiatus, which allows the popliteus tendon an avenue to course intra-articularly and maintain the integrity of the joint, but stabilize and control the motion of the posterior horn. On MR imaging, the anteroinferior and posterosuperior fascicles are visualized in approximately 90% of knee examinations and best visualized on the sagittal fluid-sensitive sequences ( Fig. 6 ). Tearing of the posterosuperior fascicle is highly associated with tears of the posterior horn of the lateral meniscus, with a sensitivity, specificity, and positive predictive value of 89%, 96%, and 79% respectively.
Other normal anatomic structures and anatomic variants that can mimic a tear if not recognized include the meniscofemoral ligaments, oblique meniscomeniscal ligament, and the transverse meniscal ligament. The most commonly described meniscofemoral ligaments originate from the posterior horn of the lateral meniscus and insert onto the lateral aspect of the posterior medial femoral condyle, with the ligament of Humphry ( Fig. 7 ) coursing anterior to the genu of the posterior cruciate ligament (PCL) and the ligament of Wrisberg traveling behind the genu of the PCL. One potential pitfall occurs when a peripheral longitudinal tear is confused for a far lateral insertion of the meniscofemoral ligament. As a general rule, the attachment of the meniscofemoral ligaments to the posterior horn of the lateral meniscus should not extend greater than 14 mm beyond the lateral border of the PCL. Therefore, if the meniscofemoral ligament is identified on 4 or more sequential sagittal MR images beyond the PCL, a peripheral longitudinal tear should be suspected and reported as such. The lesser known and extremely uncommon anterior meniscofemoral ligament connects the anterior horn of the medial meniscus to the roof of the intercondylar notch and lies parallel and posterior to the ligamentum mucosum ( Fig. 8 ). This variant should not be confused for a displaced meniscal fragment.